| Clin Mol Hepatol > Volume 30(1); 2024 > Article |
|
Dear Editor,
We read the multi-society statement regarding the updated fatty liver disease nomenclature published by the nonalcoholic fatty liver disease (NAFLD) Nomenclature Consensus Group [1] with great interest. NAFLD is now termed metabolic dysfunction-associated steatotic liver disease (MASLD).
Reflux esophagitis is a common gastrointestinal ailment that affects 10ŌĆō20% of the general population, and its prevalence continues to increase [2]. Major complications of reflux esophagitis include esophageal stricture, esophageal bleeding, BarrettŌĆÖs esophagus, and esophageal adenocarcinoma. Moreover, reflux esophagitis is associated with anxiety, depression [3], and impaired patient-reported outcomes [4].
Reflux esophagitis is often associated with aging, hiatal hernia, and lifestyle-related factors, such as poor eating and exercise habits, and metabolic dysfunction [5,6]. Furthermore, a recent study reported that NAFLD increases the risk of reflux esophagitis [7,8].
Hagstr├Čm et al. [9] previously reported that >99.5% of patients with NAFLD meet the MASLD criteria and that there is no statistical difference in the rate or risk of overall mortality or liver-related outcomes. In addition, Yoon and Jun [10] found that MASLD criteria encompass almost the entire previous NAFLD patient population (>95%), allowing seamless continuation of ongoing clinical trials for NAFLD drugs. Furthermore, Kim et al. [11] emphasized the significance of preserving and building upon existing NAFLD research to avoid unnecessary waste of research resources. However, no studies have examined the association between NAFLD and MASLD during the development of reflux esophagitis.
We aimed to compare the incidence of reflux esophagitis between patients with NAFLD and those with MASLD. A total of 18,958 consecutive patients who underwent routine health checks were evaluated using esophagogastroduodenoscopy and abdominal ultrasonography at three institutions in Japan between May 2008 and January 2021. All patients were of Asian origin. Patients who were diagnosed with reflux esophagitis using esophagogastroduodenoscopy at their initial health checkup (n=1,825), lacked data regarding alcohol consumption (n=779), reported the use of proton pump inhibitors at their initial health checkup (n=423), or had no follow-up esophagogastroduodenoscopy (n=8,315) were excluded. The data of 7,616 patients (58% male; median age 49 years [interquartile range, IQR: 41ŌĆō57 years], median body mass index: 22.6 kg/m2 [IQR: 20.5ŌĆō24.8 kg/m2]) were analyzed.
The diagnosis of steatotic liver disease (SLD) was based on the presence of moderate or severe hepatic steatosis on ultrasound. Esophagogastroduodenoscopy was performed after overnight fasting by endoscopists with experience performing >1,000 procedures. GIF-H260, GIF-H260Z, GIF-H290, GIF-H290Z, and GIF-XP290N endoscopes were used (Olympus, Tokyo, Japan). The endoscopy findings followed the modified version of the Los Angeles classification to describe the different grades of esophagitis severity (including grades M and AŌĆōD) based on the extent of the esophageal lesions [12]. The development of reflux esophagitis during the follow-up period was the primary outcome.
NAFLD was diagnosed in 1,458 patients, including 214 who did not fulfill the metabolic criteria for MASLD. All 214 individuals were classified as having cryptogenic SLD according to the new nomenclature. As a result, 85.4% of patients with NAFLD were also diagnosed with MASLD. The prevalence of hiatal hernia (18.0% and 18.4%), eating habits (eating within two hours before bedtime at least three times/week; 21.1% and 21.1%, respectively), and exercise habits (at least 30 min/session; 18.0% and 18.4%, respectively) were similar between the NAFLD and MASLD groups. Among the five metabolic risk factors listed in the criteria for MASLD, overweight/obesity or central obesity and low HDL cholesterol were the most and least prevalent risk factors, respectively (Supplementary Table 1).
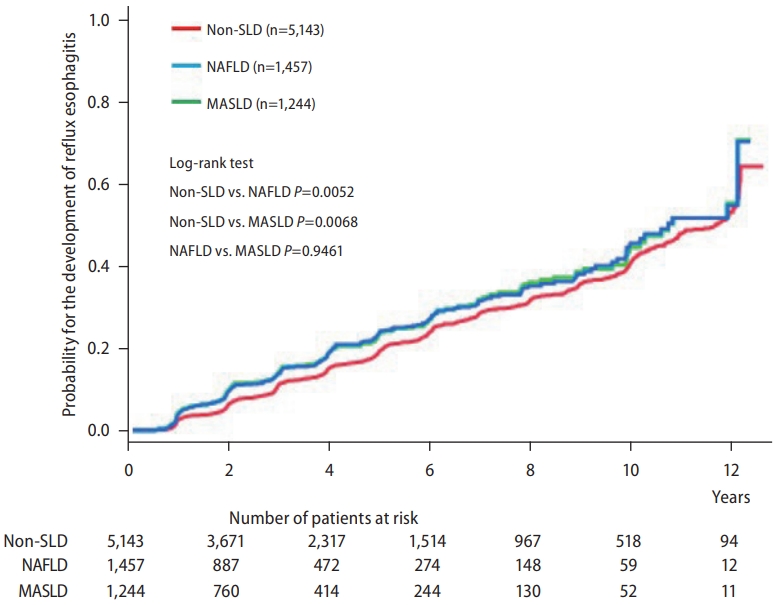
Differences in the cumulative incidence of reflux esophagitis between the non-SLD and NAFLD/MASLD groups were analyzed using log-rank tests. The cumulative incidence of reflux esophagitis was significantly higher in the NAFLD/MASLD group than in the non-SLD group (Fig. 1). However, the cumulative incidence of reflux esophagitis was not significantly different between the NAFLD and MASLD groups. The five-year cumulative incidence of reflux esophagitis was 22.1% in patients with NAFLD and 22.6% in patients with MASLD. These results indicate that excluding cryptogenic SLD from NAFLD did not alter the cumulative incidence of reflux esophagitis. In addition, there was no significant difference in the risk of reflux esophagitis between patients with NAFLD and those with MASLD.
Therefore, the MASLD diagnostic criteria may be useful for the efficient screening of patients at high risk of developing reflux esophagitis.
ACKNOWLEDGMENTS
This research was supported by the Japan Agency for Medical Research and Development (AMED) under grant number JP23fk0210090.
FOOTNOTES
AuthorsŌĆÖ contribution
Shuhei Fukunaga: study concept, design, and statistical analysis; Michita Mukasa: data extraction, interpretation of data, and critical revision of the manuscript; Dan Nakano: interpretation of data, drafting, and critical revision of the manuscript; Tsubasa Tsutsumi: interpretation of data and critical revision of the manuscript; Takumi Kawaguchi: interpretation of data and critical revision of the manuscript.
Conflicts of Interest
Takumi Kawaguchi received lecture fees from Janssen Pharmaceutical K.K., Taisho Pharmaceutical Co., Ltd., Kowa Company, Ltd., Otsuka Pharmaceutical Co., Ltd., Eisai Co., Ltd., ASKA Pharmaceutical Co., Ltd., AbbVie GK., and EA Pharma Co., Ltd. The other authors have no conflicts of interest.
SUPPLEMENTAL MATERIAL
Supplementary material is available at Clinical and Molecular Hepatology website (http://www.e-cmh.org).
Supplementary┬ĀTable┬Ā1.
Baseline characteristics and outcomes of patients with NAFLD and MAFLD, respectively
REFERENCES
1. Lazarus JV, Newsome PN, Francque SM, Kanwal F, Terrault NA, Rinella ME. Reply: A multi-society delphi consensus statement on new fatty liver disease nomenclature. Hepatology 2023 Nov 20. doi: 10.1097/HEP.0000000000000696.

2. El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014;63:871-880.



3. Jansson C, Nordenstedt H, Wallander MA, Johansson S, Johnsen R, Hveem K, et al. Severe gastro-oesophageal reflux symptoms in relation to anxiety, depression and coping in a populationbased study. Aliment Pharmacol Ther 2007;26:683-691.


4. Fuller G, Bolus R, Whitman C, Talley J, Erder MH, Joseph A, et al. PRISM, a patient-reported outcome instrument, accurately measures symptom change in refractory gastroesophageal reflux disease. Dig Dis Sci 2017;62:593-606.



5. Fujiwara Y, Machida A, Watanabe Y, Shiba M, Tominaga K, Watanabe T, et al. Association between dinner-to-bed time and gastro-esophageal reflux disease. Am J Gastroenterol 2005;100:2633-2636.


6. Mohammadi M, Ramezani Jolfaie N, Alipour R, Zarrati M. Is metabolic syndrome considered to be a risk factor for gastroesophageal reflux disease (non-erosive or erosive esophagitis)?: A systematic review of the evidence. Iran Red Crescent Med J 2016;18:e30363.



7. Tomeno W, Imajo K, Takayanagi T, Ebisawa Y, Seita K, Takimoto T, et al. Complications of non-alcoholic fatty liver disease in extrahepatic organs. Diagnostics (Basel) 2020;10:912.



8. Yi M, Peng W, Feng X, Teng F, Tang Y, Kong Q, et al. Extrahepatic morbidities and mortality of NAFLD: an umbrella review of meta-analyses. Aliment Pharmacol Ther 2022;56:1119-1130.



9. Hagstr├Čm H, Vessby J, Ekstedt M, Shang Y. 99% of patients with NAFLD meet MASLD criteria and natural history is therefore identical. J Hepatol 2023 Sep 9. doi: 10.1016/j.jhep.2023.08.026.
10. Yoon EL, Jun DW. Waiting for the changes after the adoption of steatotic liver disease. Clin Mol Hepatol 2023;29:844-850.




- TOOLS
-
METRICS

- ORCID iDs
-
Shuhei Fukunaga

https://orcid.org/0000-0002-2715-7564 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement
Supplement Print
Print



