| Clin Mol Hepatol > Volume 28(4); 2022 > Article |
|
ABSTRACT
Background/Aims
Methods
Results
ACKNOWLEDGMENTS
FOOTNOTES
SUPPLEMENTAL MATERIAL
Supplementary┬ĀTable┬Ā2.
Supplementary┬ĀTable┬Ā3.
Supplementary┬ĀFigure┬Ā1.
Supplementary┬ĀFigure┬Ā2.
Supplementary┬ĀFigure┬Ā3.
Supplementary┬ĀFigure┬Ā4.
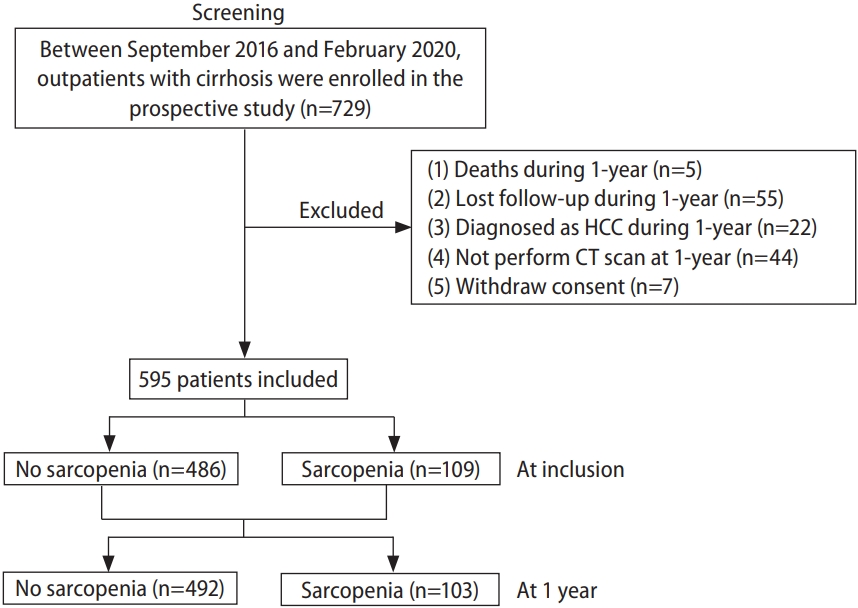
Figure┬Ā1.
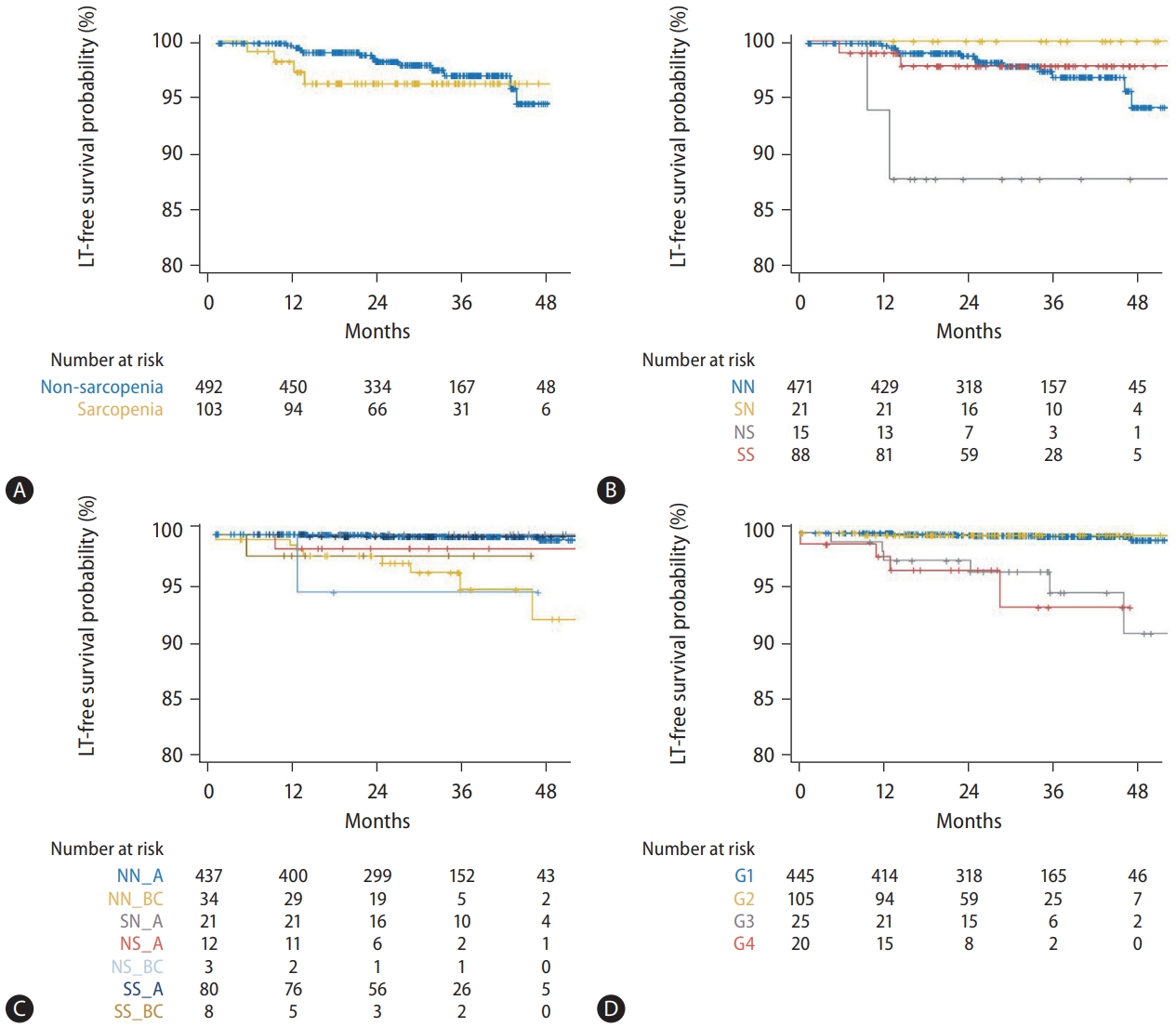
Figure┬Ā2.
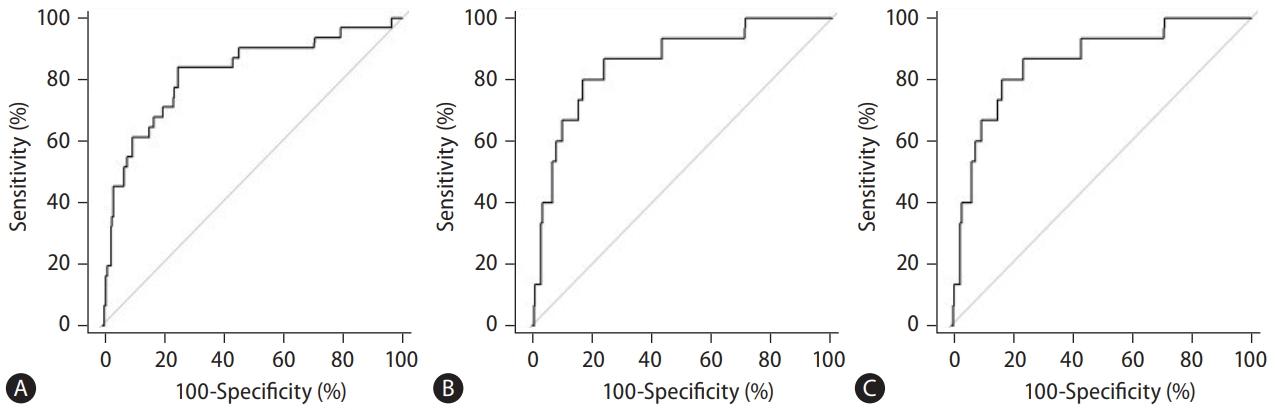
Figure┬Ā3.

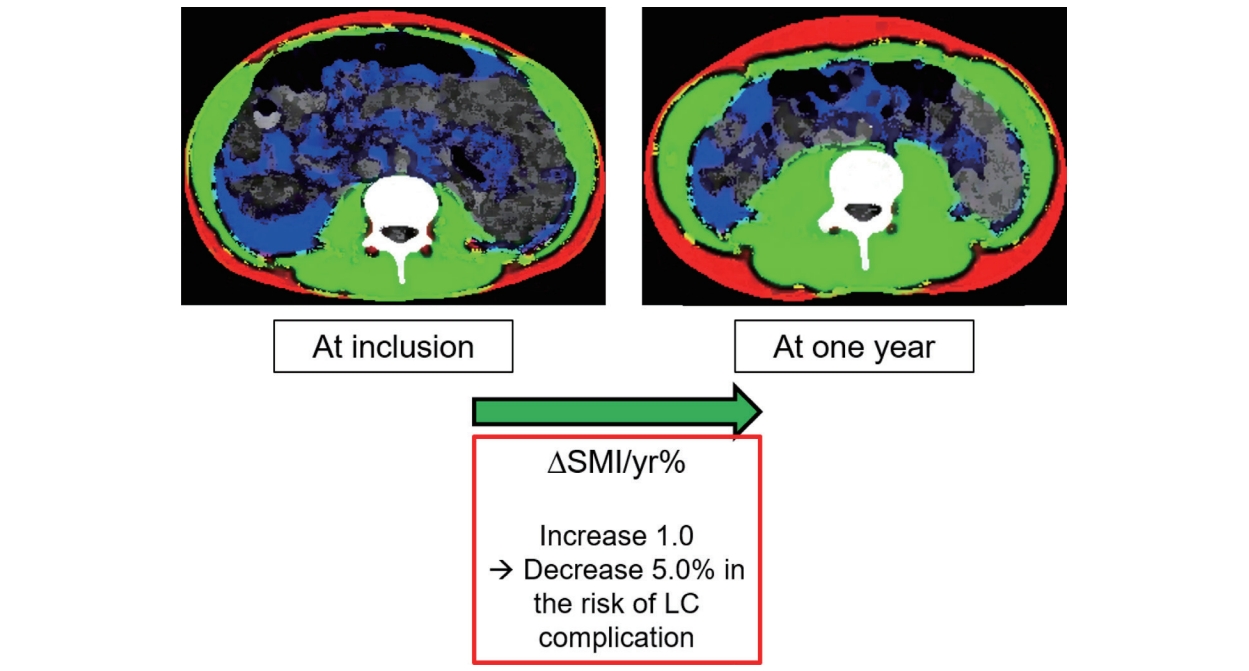
Figure┬Ā4.
Table┬Ā1.
Values are expressed as number (%) or median (interquartile range).
NN, non-sarcopenia to non-sarcopenia; SN, sarcopenia to non-sarcopenia; NS, non-sarcopenia to sarcopenia; SS, sarcopenia to sarcopenia; BMI, body mass index; AST, aspartate aminotransferase; ALT, alanine aminotransferase; INR, international normalized ratio; eGFR, estimated glomerular filtration rate; MELD, model for end-stage liver disease; SMI, skeletal muscle index; ΔSMI/yr%, % change in SMI after 1 year.
Table┬Ā2.
The values of variables were derived by examinations at the 1-year follow-up.
Model 1, multivariable Cox regression analysis with DM, hepatitis B, platelet count, albumin, AST, bilirubin, INR, eGFR, presence of ascites, and SMI, which showed P<0.01 in univariate analyses, except for the conventional prognostic models including Child-Pugh and MELD-Na scores; model 2, multivariable Cox regression analysis with model 1 and Child-Pugh score but excluding the components of Child-Pugh score; model 3, multivariable Cox regression analysis with model 1 and MELD-Na score, but excluding the components of the MELD-Na score.
LT, liver transplantation; CT, computed tomography; HR, hazard ratio; CI, confidence interval; aHR, adjusted hazard ratio; BMI, body mass index; HTN, hypertension; DM, diabetes mellitus; AST, aspartate aminotransferase; ALT, alanine aminotransferase; INR, international normalized ratio; eGFR, estimated glomerular filtration rate; MELD, model for end-stage liver disease; SMI, skeletal muscle index; ΔSMI/yr%, % change in SMI after 1 year.
Table┬Ā3.
The values of variables were derived by examinations at the 1-year follow-up.
Model 1, multivariable Cox regression analysis with HTN, DM, alcohol, hepatitis B, platelet count, albumin, AST, ALT, bilirubin, INR, sodium, presence of ascites, and ΔSMI/yr%, which showed P<0.01 in univariate analyses, except for the conventional prognostic models including Child-Pugh and MELD-Na scores; model 2, multivariable Cox regression analysis with model 1 and Child-Pugh score but excluding the components of Child-Pugh score; model 3, multivariable Cox regression analysis with model 1 and MELD-Na score, but excluding the components of the MELD-Na score.
LC, liver cirrhosis; CT, computed tomography; HR, hazard ratio; CI, confidence interval; aHR, adjusted hazard ratio; BMI, body mass index; HTN, hypertension; DM, diabetes mellitus; AST, aspartate aminotransferase; ALT, alanine aminotransferase; INR, international normalized ratio; eGFR, estimated glomerular filtration rate; MELD, model for end-stage liver disease; SMI, skeletal muscle index; ΔSMI/yr%, % change in SMI after 1 year.
Abbreviations
REFERENCES
- TOOLS
-
METRICS

- ORCID iDs
-
Young Kul Jung

https://orcid.org/0000-0002-6566-1382Hyung Joon Yim

https://orcid.org/0000-0002-6036-2754 - Related articles
-
Prognostic implications of trunk muscle mass in liver cirrhosis2018 September;24(3)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Supplement1
Supplement1 Print
Print



