1. Gin├®s P, Quintero E, Arroyo V, Ter├®s J, Bruguera M, Rimola A, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987;7:122-128.


2. DŌĆÖAmico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 2006;44:217-231.


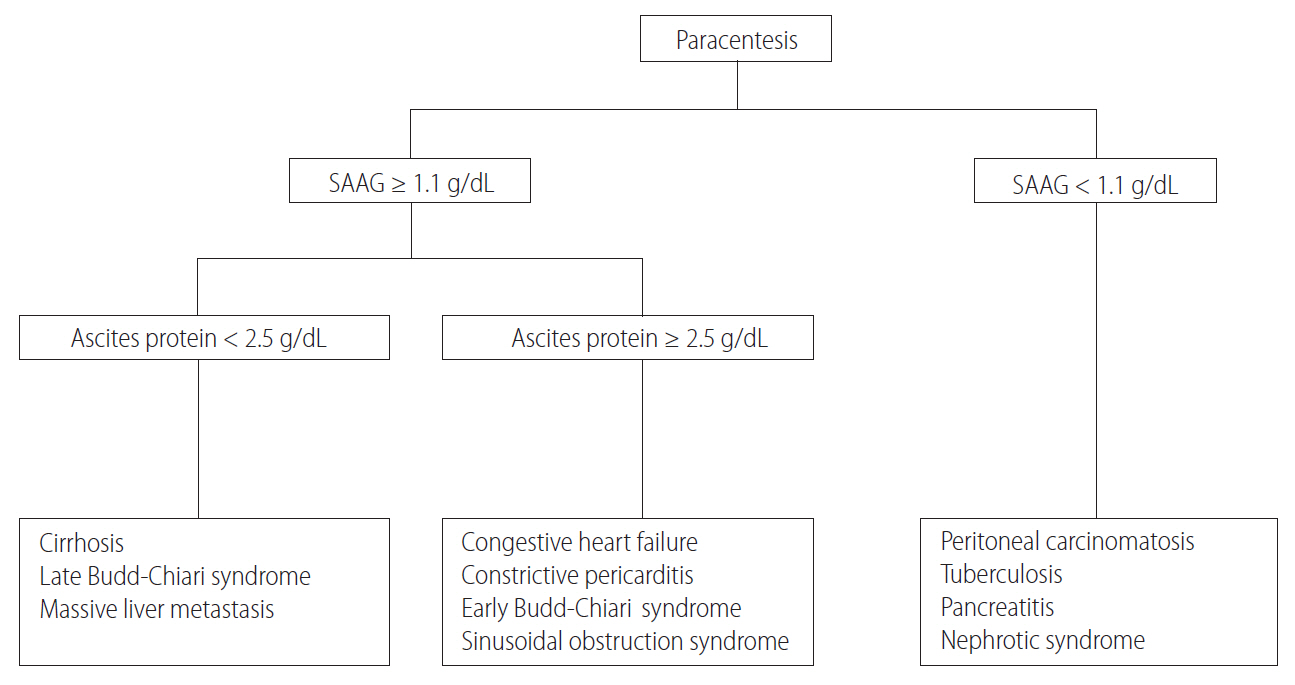
4. Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med 1992;117:215-220.


5. Shaikh MA, Khan J, Almani S, Shaikh D. Frequency of causes of ascites in patients admitted at medical unit of a tertiary medical care facility. J Ayub Med Coll Abbottabad 2010;22:88-92.

6. Runyon BA. Ascites. In: Schiff L, Schiff ER, eds. Diseases of the Liver. 7th ed. Philadelphia: Lippincott; 1993. p. 990-1015.
7. Hwangbo Y, Jung JH, Shim J, Kim BH, Jung SH, Lee CK, et al. Etiologic and laboratory analyses of ascites in patients who underwent diagnostic paracentesis. Korean J Hepatol 2007;13:185-195.

8. Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA 1982;247:1164-1166.


9. Kuiper JJ, de Man RA, van Buuren HR. Review article: management of ascites and associated complications in patients with cirrhosis. Aliment Pharmacol Ther 2007;26 Suppl 2:183-193.


10. Sheer TA, Joo E, Runyon BA. Usefulness of serum N-terminal-ProBNP in distinguishing ascites due to cirrhosis from ascites due to heart failure. J Clin Gastroenterol 2010;44:e23-e26.


11. Runyon BA. Care of patients with ascites. N Engl J Med 1994;330:337-342.


12. Borzio M, Salerno F, Piantoni L, Cazzaniga M, Angeli P, Bissoli F, et al. Bacterial infection in patients with advanced cirrhosis: a multicentre prospective study. Dig Liver Dis 2001;33:41-48.


13. European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol 2010;53:397-417.


14. Sakai H, Sheer TA, Mendler MH, Runyon BA. Choosing the location for non-image guided abdominal paracentesis. Liver Int 2005;25:984-986.


15. Webster ST, Brown KL, Lucey MR, Nostrant TT. Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol 1996;91:366-368.

16. Runyon BA. Paracentesis of ascitic fluid. A safe procedure. Arch Intern Med 1986;146:2259-2261.


17. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther 2005;21:525-529.


18. Liebowitz HR. Hazards of abdominal paracentesis in the cirrhotic patient. N Y State J Med 1962;62:2223-2229.

19. Serbin RA. Fatal hemorrhage from paracentesis; a case of Cruveilhier Baumgarten syndrome. Gastroenterology 1956;30:127-129.


20. Thomson A, Cain P, Kerlin P, Strong R. Serious hemorrhage complicating diagnostic abdominal paracentesis. J Clin Gastroenterol 1998;26:306-308.


21. Arnold C, Haag K, Blum HE, R├Čssle M. Acute hemoperitoneum after large-volume paracentesis. Gastroenterology 1997;113:978-982.


22. Qureshi WA, Harshfield D, Shah H, Netchvolodoff C, Banerjee B. An unusual complication of paracentesis. Am J Gastroenterol 1992;87:1209-1211.

24. Kang JW, Kim YD, Hong JS, Kwon JH, Seo HW, Kim SH, et al. A case of lateral abdominal wall hematoma treated with transcatheter arterial embolization. Korean J Gastroenterol 2012;59:185-188.


25. Martinet O, Reis ED, Mosimann F. Delayed hemoperitoneum following large-volume paracentesis in a patient with cirrhosis and ascites. Dig Dis Sci 2000;45:357-358.


26. McGibbon A, Chen GI, Peltekian KM, van Zanten SV. An evidence-based manual for abdominal paracentesis. Dig Dis Sci 2007;52:3307-3315.


27. Grabau CM, Crago SF, Hoff LK, Simon JA, Melton CA, Ott BJ, et al. Performance standards for therapeutic abdominal paracentesis. Hepatology 2004;40:484-488.


28. Mannucci PM. Abnormal hemostasis tests and bleeding in chronic liver disease: are they related? No. J Thromb Haemost 2006;4:721-723.


29. Caldwell SH, Hoffman M, Lisman T, Macik BG, Northup PG, Reddy KR, et al. Coagulation disorders and hemostasis in liver disease: pathophysiology and critical assessment of current management. Hepatology 2006;44:1039-1046.


30. Jeffries MA, Stern MA, Gunaratnam NT, Fontana RJ. Unsuspected infection is infrequent in asymptomatic outpatients with refractory ascites undergoing therapeutic paracentesis. Am J Gastroenterol 1999;94:2972-2976.


31. Evans LT, Kim WR, Poterucha JJ, Kamath PS. Spontaneous bacterial peritonitis in asymptomatic outpatients with cirrhotic ascites. Hepatology 2003;37:897-901.


32. Runyon BA, Hoefs JC, Morgan TR. Ascitic fluid analysis in malignancy-related ascites. Hepatology 1988;8:1104-1109.


33. Ahadi M, Tehranian S, Memar B, Vossoughinia H, Salari M, Eskandari E, et al. Diagnostic value of carcinoembryonic antigen in malignancy-related ascites: systematic review and meta-analysis. Acta Gastroenterol Belg 2014;77:418-424.

35. Saleh MA, Hammad E, Ramadan MM, Abd El-Rahman A, Enein AF. Use of adenosine deaminase measurements and QuantiFERON in the rapid diagnosis of tuberculous peritonitis. J Med Microbiol 2012;61(Pt 4):514-519.


36. Portillo-G├│mez L, Morris SL, Panduro A. Rapid and efficient detection of extra-pulmonary Mycobacterium tuberculosis by PCR analysis. Int J Tuberc Lung Dis 2000;4:361-370.

37. Inadomi JM, Kapur S, Kinkhabwala M, Cello JP. The laparoscopic evaluation of ascites. Gastrointest Endosc Clin N Am 2001;11:79-91.


39. Singh MM, Bhargava AN, Jain KP. Tuberculous peritonitis. An evaluation of pathogenetic mechanisms, diagnostic procedures and therapeutic measures. N Engl J Med 1969;281:1091-1094.


40. Voigt MD, Kalvaria I, Trey C, Berman P, Lombard C, Kirsch RE. Diagnostic value of ascites adenosine deaminase in tuberculous peritonitis. Lancet 1989;1:751-754.


41. Bhargava DK, Gupta M, Nijhawan S, Dasarathy S, Kushwaha AK. Adenosine deaminase (ADA) in peritoneal tuberculosis: diagnostic value in ascitic fluid and serum. Tubercle 1990;71:121-126.


42. Ribera E, Mart├Łnez V├Īsquez JM, Oca├▒a I, Ruiz I, Jim├Łnez JG, Encabo G, et al. Diagnostic value of ascites gamma interferon levels in tuberculous peritonitis. Comparison with adenosine deaminase activity. Tubercle 1991;72:193-197.


43. Dwivedi M, Misra SP, Misra V, Kumar R. Value of adenosine deaminase estimation in the diagnosis of tuberculous ascites. Am J Gastroenterol 1990;85:1123-1125.

44. Hillebrand DJ, Runyon BA, Yasmineh WG, Rynders GP. Ascitic fluid adenosine deaminase insensitivity in detecting tuberculous peritonitis in the United States. Hepatology 1996;24:1408-1412.


45. Lee JS, Kim KA, Lee WJ, Jeon YB, Lee JW, Kim YS, et al. Diagnostic value of ascitic fluid adenosine deaminase activity for diagnosis of tuberculous peritonitis. Korean J Gastroenterol 2003;41:126-132.
46. Liao YJ, Wu CY, Lee SW, Lee CL, Yang SS, Chang CS, et al. Adenosine deaminase activity in tuberculous peritonitis among patients with underlying liver cirrhosis. World J Gastroenterol 2012;18:5260-5265.


47. Cappell MS, Shetty V. A multicenter, case-controlled study of the clinical presentation and etiology of ascites and of the safety and clinical efficacy of diagnostic abdominal paracentesis in HIV seropositive patients. Am J Gastroenterol 1994;89:2172-2177.

48. Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology 1990;98:127-133.


49. Wu SS, Lin OS, Chen YY, Hwang KL, Soon MS, Keeffe EB. Ascitic fluid carcinoembryonic antigen and alkaline phosphatase levels for the differentiation of primary from secondary bacterial peritonitis with intestinal perforation. J Hepatol 2001;34:215-221.


50. Ridinger HA, Kavitt RT, Green JK. Urinary ascites and renal failure from unrecognized bladder rupture. Am J Med 2012;125:e1-e2.


52. Runyon BA. Malignancy-related ascites and ascitic fluid ŌĆ£humoral tests of malignancyŌĆØ. J Clin Gastroenterol 1994;18:94-98.


53. Zuckerman E, Lanir A, Sabo E, Rosenvald-Zuckerman T, Matter I, Yeshurun D, et al. Cancer antigen 125: a sensitive marker of ascites in patients with liver cirrhosis. Am J Gastroenterol 1999;94:1613-1618.


54. Garg H, Sarin SK, Kumar M, Garg V, Sharma BC, Kumar A. Tenofovir improves the outcome in patients with spontaneous reactivation of hepatitis B presenting as acute-on-chronic liver failure. Hepatology 2011;53:774-780.


55. Runyon BA; AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009;49:2087-2107.


56. Veldt BJ, Lain├® F, GuillygomarcŌĆÖh A, Lauvin L, Boudjema K, Messner M, et al. Indication of liver transplantation in severe alcoholic liver cirrhosis: quantitative evaluation and optimal timing. J Hepatol 2002;36:93-98.


58. Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet 2007;370:1915-1922.


59. Moon W, Choi MS, Moon YM, Paik SW, Lee JH, Koh KC, et al. Efficacy and safety of adefovir dipivoxil in patients with decompensated liver cirrhosis with Lamivudine resistance compared to patients with compensated liver disease. Korean J Hepatol 2005;11:125-134.

60. Shim JH, Lee HC, Kim KM, Lim YS, Chung YH, Lee YS, et al. Efficacy of entecavir in treatment-naïve patients with hepatitis B virus-related decompensated cirrhosis. J Hepatol 2010;52:176-182.


61. Yao FY, Bass NM. Lamivudine treatment in patients with severely decompensated cirrhosis due to replicating hepatitis B infection. J Hepatol 2000;33:301-307.


62. Manolakopoulos S, Triantos C, Theodoropoulos J, Vlachogiannakos J, Kougioumtzan A, Papatheodoridis G, et al. Antiviral therapy reduces portal pressure in patients with cirrhosis due to HBeAg-negative chronic hepatitis B and significant portal hypertension. J Hepatol 2009;51:468-474.


63. Curry MP, OŌĆÖLeary JG, Bzowej N, Muir AJ, Korenblat KM, Fenkel JM, et al. Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N Engl J Med 2015;373:2618-2628.


64. Afdhal N, Everson G, Calleja JL, McCaughan G, Symonds WT, Denning J, et al. Sofosbuvir and ribavirin for the treatment chronic HCV with cirrhosis and portal hypertension with and without decompensation: early virologic response and safety. J Hepatol 2014;60:S28.

66. Plauth M, Cabr├® E, Campillo B, Kondrup J, Marchesini G, Sch├╝tz T, et al. ESPEN guidelines on Parenteral Nutrition: hepatology. Clin Nutr 2009;28:436-444.


67. Plauth M, Cabr├® E, Riggio O, Assis-Camilo M, Pirlich M, Kondrup J, et al. ESPEN guidelines on Enteral Nutrition: liver disease. Clin Nutr 2006;25:285-294.


68. Lochs H, Plauth M. Liver cirrhosis: rationale and modalities for nutritional support--the European Society of Parenteral and Enteral Nutrition consensus and beyond. Curr Opin Clin Nutr Metab Care 1999;2:345-349.


70. Zillikens MC, van den Berg JW, Wattimena JL, Rietveld T, Swart GR. Nocturnal oral glucose supplementation. The effects on protein metabolism in cirrhotic patients and in healthy controls. J Hepatol 1993;17:377-383.


71. Chang WK, Chao YC, Tang HS, Lang HF, Hsu CT. Effects of extra-carbohydrate supplementation in the late evening on energy expenditure and substrate oxidation in patients with liver cirrhosis. JPEN J Parenter Enteral Nutr 1997;21:96-99.


72. Plank LD, Gane EJ, Peng S, Muthu C, Mathur S, Gillanders L, et al. Nocturnal nutritional supplementation improves total body protein status of patients with liver cirrhosis: a randomized 12-month trial. Hepatology 2008;48:557-566.


73. Sorrentino P, Castaldo G, Tarantino L, Bracigliano A, Perrella A, Perrella O, et al. Preservation of nutritional-status in patients with refractory ascites due to hepatic cirrhosis who are undergoing repeated paracentesis. J Gastroenterol Hepatol 2012;27:813-822.


74. Stickel F, Hoehn B, Schuppan D, Seitz HK. Review article: nutritional therapy in alcoholic liver disease. Aliment Pharmacol Ther 2003;18:357-373.


75. DiCecco SR, Francisco-Ziller N. Nutrition in alcoholic liver disease. Nutr Clin Pract 2006;21:245-254.


76. Grungreiff K, Reinhold D, Wedemeyer H. The role of zinc in liver cirrhosis. Ann Hepatol 2016;15:7-16.


77. Fialla AD, Israelsen M, Hamberg O, Krag A, Gluud LL. Nutritional therapy in cirrhosis or alcoholic hepatitis: a systematic review and meta-analysis. Liver Int 2015;35:2072-2078.


78. Shiozawa S, Usui T, Kuhara K, Tsuchiya A, Miyauchi T, Kono T, et al. Impact of branched-chain amino acid-enriched nutrient on liver cirrhosis with hepatocellular carcinoma undergoing transcatheter arterial chemoembolization in Barcelona Clinic Liver Cancer Stage B: a prospective study. J Nippon Med Sch 2016;83:248-256.


79. Wong F. Management of ascites in cirrhosis. J Gastroenterol Hepatol 2012;27:11-20.


82. Reynolds TB. Ascites. Clin Liver Dis 2000;4:151-168 vii.


83. Santos J, Planas R, Pardo A, Dur├Īndez R, Cabr├® E, Morillas RM, et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J Hepatol 2003;39:187-192.


84. Angeli P, Dalla Pria M, De Bei E, Albino G, Caregaro L, Merkel C, et al. Randomized clinical study of the efficacy of amiloride and potassium canrenoate in nonazotemic cirrhotic patients with ascites. Hepatology 1994;19:72-79.


85. Gentilini P, Laffi G, La Villa G, Carloni V, Foschi M, Romanelli RG, et al. Torasemide in the treatment of patients with cirrhosis and ascites. Cardiovasc Drugs Ther 1993;7 Suppl 1:81-85.


86. Bernardi M. Optimum use of diuretics in managing ascites in patients with cirrhosis. Gut 2010;59:10-11.


87. Angeli P, Fasolato S, Mazza E, Okolicsanyi L, Maresio G, Velo E, et al. Combined versus sequential diuretic treatment of ascites in non-azotaemic patients with cirrhosis: results of an open randomised clinical trial. Gut 2010;59:98-104.


88. Korean Association for the Study of the Liver. Treatment guideline of complications of liver cirrhosis. Korean J Hepatol 2005;11(Suppl 4):S115-S138.
89. Pockros PJ, Reynolds TB. Rapid diuresis in patients with ascites from chronic liver disease: the importance of peripheral edema. Gastroenterology 1986;90:1827-1833.


91. Stiehm AJ, Mendler MH, Runyon BA. Detection of diuretic-resistace or diuretic-sensitivity by the spot urine Na+/K+ ratio in 729 specimens from cirrhotics with ascites: approximately 90% accuracy as compared to 24-hour urine Na+ excretion. Hepatology 2002;36:222A.
92. Park JE, Lee CH, Kim BS, Shin IH. Diagnostic usefulness of the random urine Na/K ratio in cirrhotic patients with ascites: a pilot study. Korean J Hepatol 2010;16:66-74.


93. Marchesini G, Dioguardi FS, Bianchi GP, Zoli M, Bellati G, Roffi L, et al. Long-term oral branched-chain amino acid treatment in chronic hepatic encephalopathy. A randomized double-blind casein-controlled trial. The Italian Multicenter Study Group. J Hepatol 1990;11:92-101.


95. Hirsch S, Bunout D, de la Maza P, Iturriaga H, Petermann M, Icazar G, et al. Controlled trial on nutrition supplementation in outpatients with symptomatic alcoholic cirrhosis. JPEN J Parenter Enteral Nutr 1993;17:119-124.


96. Yatsuhashi H, Ohnishi Y, Nakayama S, Iwase H, Nakamura T, Imawari M. Anti-hypoalbuminemic effect of branched-chain amino acid granules in patients with liver cirrhosis is independent of dietary energy and protein intake. Hepatol Res 2011;41:1027-1035.


97. Kawamura E, Habu D, Morikawa H, Enomoto M, Kawabe J, Tamori A, et al. A randomized pilot trial of oral branched-chain amino acids in early cirrhosis: validation using prognostic markers for preliver transplant status. Liver Transpl 2009;15:790-797.


99. Ruiz-Marg├Īin A, Mac├Łas-Rodr├Łguez RU, R├Łos-Torres SL, Rom├Īn-Calleja BM, M├®ndez-Guerrero O, Rodr├Łguez-C├│rdova P, et al. Effect of a high-protein, high-fiber diet plus supplementation with branched-chain amino acids on the nutritional status of patients with cirrhosis. Rev Gastroenterol Mex 2018;83:9-15.

101. Park JG, Tak WY, Park SY, Kweon YO, Jang SY, Lee YR, et al. Effects of branched-chain amino acids (BCAAs) on the progression of advanced liver disease: a Korean nationwide, multicenter, retrospective, observational, cohort study. Medicine (Baltimore) 2017;96:e6580.



104. Gentilini P, Casini-Raggi V, Di Fiore G, Romanelli RG, Buzzelli G, Pinzani M, et al. Albumin improves the response to diuretics in patients with cirrhosis and ascites: results of a randomized, controlled trial. J Hepatol 1999;30:639-645.


105. Bernardi M, Caraceni P, Navickis RJ, Wilkes MM. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology 2012;55:1172-1181.


106. Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, Ruiz-del-Arbol L, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med 1999;341:403-409.


108. Italian Association for the Study of the Liver (AISF); Italian Society of Transfusion Medicine and Immunohaematology (SIMTI). AISF-SIMTI position paper: the appropriate use of albumin in patients with liver cirrhosis. Dig Liver Dis 2016;48:4-15.


109. Tit├│ L1, Gin├©s P, Arroyo V, Planas R, Pan├®s J, Rimola A, et al. Total paracentesis associated with intravenous albumin management of patients with cirrhosis and ascites. Gastroenterology 1990;98:146-151.


110. Hong SP, Eun YG, Kim HJ, Kim BH, Chang YW, Lee JI, et al. Effects of large volume paracentesis. Korean J Med 1991;40:147-152.
111. Arroyo V, Gin├©s P, Gerbes AL, Dudley FJ, Gentilini P, Laffi G, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club. Hepatology 1996;23:164-176.


112. Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, et al. The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology 2003;38:258-266.


113. Choi CH, Ahn SH, Kim DY, Lee SK, Park JY, Chon CY, et al. LongŌĆÉterm clinical outcome of large volume paracentesis with intravenous albumin in patients with spontaneous bacterial peritonitis: a randomized prospective study. J Gastroenterol Hepatol 2005;20:1215-1222.


115. Gin├©s A, Fern├Īndez-Esparrach G, Monescillo A, Vila C, Dom├©nech E, Abecasis R, et al. Randomized trial comparing albumin, dextran 70, and polygeline in cirrhotic patients with ascites treated by paracentesis. Gastroenterology 1996;111:1002-1010.


116. Moreau R, Valla DC, DurandŌĆÉZaleski I, Bronowicki JP, Durand F, Chaput JC, et al. Comparison of outcome in patients with cirrhosis and ascites following treatment with albumin or a synthetic colloid. Liver Int 2006;26:46-54.


117. Singh V, Dheerendra PC, Singh B, Nain CK, Chawla D, Sharma N, et al. Midodrine versus albumin in the prevention of paracentesis-induced circulatory dysfunction in cirrhotics: a randomized pilot study. Am J Gastroenterol 2008;103:1399-1405.


118. Lata J, Marecek Z, Fejfar T, Zdenek P, Bru┬░ ha R, Safka V, et al. The efficacy of terlipressin in comparison with albumin in the prevention of circulatory changes after the paracentesis of tense ascites--a randomized multicentric study. Hepatogastroenterology 2007;54:1930-1933.

119. Serst├® T, Francoz C, Durand F, Rautou PE, Melot C, Valla D, et al. Beta-blockers cause paracentesis-induced circulatory dysfunction in patients with cirrhosis and refractory ascites: a cross-over study. J Hepatol 2011;55:794-799.


120. Serst├® T, Melot C, Francoz C, Durand F, Rautou PE, Valla D, et al. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology 2010;52:1017-1022.


121. Llach J, Gin├©s P, Arroyo V, Rimola A, Tit├│ L, Badalamenti S, et al. Prognostic value of arterial pressure, endogenous vasoactive systems, and renal function in cirrhotic patients admitted to the hospital for the treatment of ascites. Gastroenterology 1988;94:482-487.


123. Singh V, Dhungana SP, Singh B, Vijayverghia R, Nain CK, Sharma N, et al. Midodrine in patients with cirrhosis and refractory or recurrent ascites: a randomized pilot study. J Hepatol 2012;56:348-354.


124. Yang YY, Lin HC, Lee WP, Chu CJ, Lin MW, Lee FY, et al. Association of the G-protein and ╬▒2-adrenergic receptor gene and plasma norepinephrine level with clonidine improvement of the effects of diuretics in patients with cirrhosis with refractory ascites: a randomised clinical trial. Gut 2010;59:1545-1553.


125. Wong F, Watson H, Gerbes A, Vilstrup H, Badalamenti S, Bernardi M, et al. Satavaptan for the management of ascites in cirrhosis: efficacy and safety across the spectrum of ascites severity. Gut 2012;61:108-116.


126. R├Čssle M, Ochs A, G├╝lberg V, Siegerstetter V, Holl J, Deibert P, et al. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med 2000;342:1701-1707.


127. Salerno F, Camm├Ā C, Enea M, R├Čssle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology 2007;133:825-834.


128. Gin├©s P, Uriz J, Calahorra B, Garcia-Tsao G, Kamath PS, Del Arbol LR, et al. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology 2002;123:1839-1847.


129. Sanyal AJ, Genning C, Reddy KR, Wong F, Kowdley KV, Benner K, et al. The North American study for the treatment of refractory ascites. Gastroenterology 2003;124:634-641.


130. Miraglia R, Maruzzelli L, Tuzzolino F, Petridis I, DŌĆÖAmico M, Luca A. Transjugular intrahepatic portosystemic shunts in patients with cirrhosis with refractory ascites: comparison of clinical outcomes by using 8-and 10-mm PTFE-covered Stents. Radiology 2017;284:281-288.


132. Bureau C, Thabut D, Oberti F, Dharancy S, Carbonell N, Bouvier A, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology 2017;152:157-163.


133. Berry K, Lerrigo R, Liou IW, Ioannou GN. Association between transjugular intrahepatic portosystemic shunt and survival in patients with cirrhosis. Clin Gastroenterol Hepatol 2016;14:118-123.


134. Hosokawa I, Adam R, Allard MA, Pittau G, Vibert E, Cherqui D, et al. Outcomes of surgical shunts and transjugular intrahepatic portasystemic stent shunts for complicated portal hypertension. Br J Surg 2017;104:443-451.


135. Rabie R, Cazzaniga M, Salerno F, Wong F. The effect of cirrhotic cardiomyopathy on the post-TIPS outcome of patients treated for complications of portal hypertension. Hepatology 2006;44:444A.

136. Azoulay D, Castaing D, Dennison A, Martino W, Eyraud D, Bismuth H. Transjugular intrahepatic portosystemic shunt worsens the hyperdynamic circulatory state of the cirrhotic patient: preliminary report of a prospective study. Hepatology 1994;19:129-132.


137. Michl P. Transjugular intrahepatic portosystemic shunt for cirrhosis and ascites: effects in patients with organic or functional renal failure. Scand J Gastroenterol 2000;35:654-658.


139. Heuman DM, AbouŌĆÉAssi SG, Habib A, Williams LM, Stravitz RT, Sanyal AJ, et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology 2004;40:802-810.


141. Luca A, Angermayr B, Bertolini G, Koenig F, Vizzini G, Ploner M, et al. An integrated MELD model including serum sodium and age improves the prediction of early mortality in patients with cirrhosis. Liver Transpl 2007;13:1174-1180.


142. Trotter J, Pieramici E, Everson GT. Chronic albumin infusions to achieve diuresis in patients with ascites who are not candidates for transjugular intrahepatic portosystemic shunt (TIPS). Dig Dis Sci 2005;50:1356-1360.


143. Lenaerts A, Codden T, Henry JP, Legros F, Ligny G. Comparative pilot study of repeated large volume paracentesis vs the combination on clonidine-spironolactone in the treatment of cirrhosis-associated refractory ascites. Gastroenterol Clin Biol 2005;29:1137-1142.


144. Gin├©s P, Arroyo V, Vargas V, Planas R, Casafont F, Pan├®s J, et al. Paracentesis with intravenous infusion of albumin as compared with peritoneovenous shunting in cirrhosis with refractory ascites. N Engl J Med 1991;325:829-835.


145. Bureau C, Adebayo D, Chalret de Rieu M, Elkrief L, Valla D, Peck-Radosavljevic M, et al. Alfapump(R) system vs. large volume paracentesis for refractory ascites: a multicenter randomized controlled study. J Hepatol 2017;67:940-949.


147. Graziotto A, Rossaro L, Inturri P, Salvagnini M. Reinfusion of concentrated ascitic fluid versus total paracentesis. A randomized prospective trial. Dig Dis Sci 1997;42:1708-1714.


148. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013;57:1651-1653.


150. Angeli P, Wong F, Watson H, Gin├©s P; CAPPS Investigators. Hyponatremia in cirrhosis: results of a patient population survey. Hepatology 2006;44:1535-1542.


151. Ge PS, Runyon BA. Treatment of patients with cirrhosis. N Engl J Med 2016;375:2104-2105.


152. Abelmann WH. Hyperdynamic circulation in cirrhosis: a historical perspective. Hepatology 1994;20:1356-1358.


153. Kim MY, Baik SK. Hyperdynamic circulation in patients with liver cirrhosis and portal hypertension. Korean J Gastroenterol 2009;54:143-148.


154. Battista S, Bar F, Mengozzi G, Zanon E, Grosso M, Molino G. Hyperdynamic circulation in patients with cirrhosis: direct measurement of nitric oxide levels in hepatic and portal veins. J Hepatol 1997;26:75-80.


156. H├®bert RL, Jacobson HR, Breyer MD. PGE2 inhibits AVP-induced water flow in cortical collecting ducts by protein kinase C activation. Am J Physiol 1990;259(2 Pt 2):F318-F325.


157. Bichet D, Szatalowicz V, Chaimovitz C, Schrier RW. Role of vasopressin in abnormal water excretion in cirrhotic patients. Ann Intern Med 1982;96:413-417.


158. Adrogu├® HJ, Madias NE. Hyponat remia. N Engl J Med 2000;342:1581-1589.


159. Gerbes AL, G├╝lberg V, Gin├©s P, Decaux G, Gross P, Gandjini H, et al. Therapy of hyponatremia in cirrhosis with a vasopressin receptor antagonist: a randomized double-blind multicenter trial. Gastroenterology 2003;124:933-939.


160. Wong F, Blei AT, Blendis LM, Thuluvath PJ. A vasopressin receptor antagonist (VPA-985) improves serum sodium concentration in patients with hyponatremia: a multicenter, randomized, placebo-controlled trial. Hepatology 2003;37:182-191.


162. Martinez-Castelao A. Conivaptan (Yamanouchi). Curr Opin Investig Drugs 2002;3:89-95.

163. Wada K, Tahara A, Arai Y, Aoki M, Tomura Y, Tsukada J, et al. Effect of the vasopressin receptor antagonist conivaptan in rats with heart failure following myocardial infarction. Eur J Pharmacol 2002;450:169-177.


164. Fern├Īndez-Varo G, Ros J, Cejudo-Mart├Łn P, Cano C, Arroyo V, Rivera F, et al. Effect of the V1a/V2-AVP receptor antagonist, Conivaptan, on renal water metabolism and systemic hemodynamics in rats with cirrhosis and ascites. J Hepatol 2003;38:755-761.


167. Ghali JK, Koren MJ, Taylor JR, Brooks-Asplund E, Fan K, Long WA, et al. Efficacy and safety of oral conivaptan: a V1A/V2 vasopressin receptor antagonist, assessed in a randomized, placebo-controlled trial in patients with euvolemic or hypervolemic hyponatremia. J Clin Endocrinol Metab 2006;91:2145-2152.


169. Soupart A, Gross P, Legros JJ, Alf├Čldi S, Annane D, Heshmati HM, et al. Successful long-term treatment of hyponatremia in syndrome of inappropriate antidiuretic hormone secretion with satavaptan (SR121463B), an orally active non-peptide vasopressin V2-receptor antagonist. Clin J Am Soc Nephrol 2006;1:1154-1160.


170. Gin├©s P, Wong F, Watson H, Milutinovic S, del Arbol LR, Olteanu D, et al. Effects of satavaptan, a selective vasopressin V(2) receptor antagonist, on ascites and serum sodium in cirrhosis with hyponatremia: a randomized trial. Hepatology 2008;48:204-213.


171. Wong F, Gines P, Watson H, Horsmans Y, Angeli P, Gow P, et al. Effects of a selective vasopressin V2 receptor antagonist, satavaptan, on ascites recurrence after paracentesis in patients with cirrhosis. J Hepatol 2010;53:283-290.


172. Konstam MA, Gheorghiade M, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, et al. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. JAMA 2007;297:1319-1331.


173. C├Īrdenas A, Gin├©s P, Marotta P, Czerwiec F, Oyuang J, Guevara M, et al. Tolvaptan, an oral vasopressin antagonist, in the treatment of hyponatremia in cirrhosis. J Hepatol 2012;56:571-578.


180. Biggins SW, Rodriguez HJ, Bacchetti P, Bass NM, Roberts JP, Terrault NA. Serum sodium predicts mortality in patients listed for liver transplantation. Hepatology 2005;41:32-39.


181. Guevara M, Baccaro ME, R├Łos J, Mart├Łn-Llah├Ł M, Uriz J, Ruiz del Arbol L, et al. Risk factors for hepatic encephalopathy in patients with cirrhosis and refractory ascites: relevance of serum sodium concentration. Liver Int 2010;30:1137-1142.


182. Pereira G, Guevara M, Fagundes C, Sol├Ī E, Rodr├Łguez E, Fern├Īndez J, et al. Renal failure and hyponatremia in patients with cirrhosis and skin and soft tissue infection. A retrospective study. J Hepatol 2012;56:1040-1046.


185. Caly WR, Strauss E. A prospective study of bacterial infections in patients with cirrhosis. J Hepatol 1993;18:353-358.


187. Rimola A, Garc├Ła-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol 2000;32:142-153.


188. Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic fluid culture technique. Gastroenterology 1988;95:1351-1355.


189. Kim SU, Kim DY, Lee CK, Park JY, Kim SH, Kim HM, et al. Ascitic fluid infection in patients with hepatitis B virus-related liver cirrhosis: culture-negative neutrocytic ascites versus spontaneous bacterial peritonitis. J Gastroenterol Hepatol 2010;25:122-128.


190. Pelletier G, Lesur G, Ink O, Hagege H, Attali P, Buffet C, et al. Asymptomatic bacterascites: is it spontaneous bacterial peritonitis? Hepatology 1991;14:112-115.


191. Runyon BA. Monomicrobial non-neutrocytic bacterascites: a variant of spontaneous bacterial peritonitis. Hepatology 1990;12(4 Pt 1):710-715.


192. Rerknimitr R, Limmathurotsakul D, Bhokaisawan N, Kongkam P, Treeprasertsuk S, Kullavanijaya P. A comparison of diagnostic efficacies among different reagent strips and automated cell count in spontaneous bacterial peritonitis. J Gastroenterol Hepatol 2010;25:946-950.


193. Nousbaum JB, Cadranel JF, Nahon P, Khac EN, Moreau R, Th├®venot T, et al. Diagnostic accuracy of the Multistix 8 SG reagent strip in diagnosis of spontaneous bacterial peritonitis. Hepatology 2007;45:1275-1281.


194. Farmer AD, Cook MJ, Bruckner Holt CE, Syn WK, Lewis MJ. Leucocyte esterase reagent strips for the diagnosis of spontaneous bacterial peritonitis: a systematic review by Koulaouzidis et al. Eur J Gastroenterol Hepatol 2009;21:1102.


195. Soriano G, Castellote J, Alvarez C, Girbau A, Gordillo J, Baliellas C, et al. Secondary bacterial peritonitis in cirrhosis: a retrospective study of clinical and analytical characteristics, diagnosis and management. J Hepatol 2010;52:39-44.


196. Runyon BA, Hoefs JC. Ascitic fluid analysis in the differentiation of spontaneous bacterial peritonitis from gastrointestinal tract perforation into ascitic fluid. Hepatology 1984;4:447-450.


197. Teh SH, Nagorney DM, Stevens SR, Offord KP, Therneau TM, Plevak DJ, et al. Risk factors for mortality after surgery in patients with cirrhosis. Gastroenterology 2007;132:1261-1269.


198. Park MK, Lee JH, Byun YH, Lee Hle, Gwak GY, Choi MS, et al. Changes in the profiles of causative agents and antibiotic resistance rate for spontaneous bacterial peritonitis: an analysis of cultured microorganisms in recent 12 years. Korean J Hepatol 2007;13:370-377.


203. Runyon BA, Akriviadis EA, Sattler FR, Cohen J. Ascitic fluid and serum cefotaxime and desacetyl cefotaxime levels in patients treated for bacterial peritonitis. Dig Dis Sci 1991;36:1782-1786.


204. Felisart J, Rimola A, Arroyo V, Perez-Ayuso RM, Quintero E, Gines P, et al. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology 1985;5:457-462.


205. Ricart E, Soriano G, Novella MT, Ortiz J, S├Ābat M, Kolle L, et al. Amoxicillin-clavulanic acid versus cefotaxime in the therapy of bacterial infections in cirrhotic patients. J Hepatol 2000;32:596-602.


206. Tuncer I, Topcu N, Durmus A, Turkdogan MK. Oral ciprofloxacin versus intravenous cefotaxime and ceftriaxone in the treatment of spontaneous bacterial peritonitis. Hepatogastroenterology 2003;50:1426-1430.

207. Yim HJ, Suh SJ, Jung YK, Kim MY, Baik SK, Kim HS, et al. Comparison of efficacy of cefotaxime, ceftriaxone, and ciprofloxacin for the treatment of spontaneous bacterial peritonitis in patients with liver cirrhosis: a randomized controlled trial. J Hepatol 2017;66:S374-S375.

208. Fran├¦a A, Giordano HM, Sev├Ī-Pereira T, Soares EC. Five days of ceftriaxone to treat spontaneous bacterial peritonitis in cirrhotic patients. J Gastroenterol 2002;37:119-122.


210. Baskol M, Gursoy S, Baskol G, Ozbakir O, Guven K, Yucesoy M. Five days of ceftriaxone to treat culture negative neutrocytic ascites in cirrhotic patients. J Clin Gastroenterol 2003;37:403-405.


211. Terg R, Cobas S, Fassio E, Landeira G, R├Łos B, Vasen W, et al. Oral ciprofloxacin after a short course of intravenous ciprofloxacin in the treatment of spontaneous bacterial peritonitis: results of a multicenter, randomized study. J Hepatol 2000;33:564-569.


212. Navasa M, Follo A, Llovet JM, Clemente G, Vargas V, Rimola A, et al. Randomized, comparative study of oral ofloxacin versus intravenous cefotaxime in spontaneous bacterial peritonitis. Gastroenterology 1996;111:1011-1017.


213. Kim J, Kang CI, Joo EJ, Ha YE, Cho SY, Gwak GY, et al. Risk factor of community-onset spontaneous bacterial peritonitis caused by fluoroquinolone-resistant Escherichia coli in patients with cirrhosis. Liver Int 2014;34:695-699.


214. Fern├Īndez J, Navasa M, G├│mez J, Colmenero J, Vila J, Arroyo V, et al. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology 2002;35:140-148.


217. Kim MJ, Song KH, Kim NH, Choe PG, Park WB, Bang JH, et al. Clinical outcomes of spontaneous bacterial peritonitis due to extended-spectrum beta-lactamase-producing Escherichia coli or Klebsiella pneumoniae: a retrospective cohort study. Hepatol Int 2014;8:582-587.


218. Park YH, Lee HC, Song HG, Jung S, Ryu SH, Shin JW, et al. Recent increase in antibiotic-resistant microorganisms in patients with spontaneous bacterial peritonitis adversely affects the clinical outcome in Korea. J Gastroenterol Hepatol 2003;18:927-933.


219. Piano S, Fasolato S, Salinas F, Romano A, Tonon M, Morando F, et al. The empirical antibiotic treatment of nosocomial spontaneous bacterial peritonitis: results of a randomized, controlled clinical trial. Hepatology 2016;63:1299-1309.


220. Fern├Īndez J, Acevedo J, Castro M, Garcia O, de Lope CR, Roca D, et al. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology 2012;55:1551-1561.


221. Ariza X, Castellote J, Lora-Tamayo J, Girbau A, Salord S, Rota R, et al. Risk factors for resistance to ceftriaxone and its impact on mortality in community, healthcare and nosocomial spontaneous bacterial peritonitis. J Hepatol 2012;56:825-832.


222. Fern├Īndez J, Tandon P, Mensa J, Garcia-Tsao G. Antibiotic prophylaxis in cirrhosis: good and bad. Hepatology 2016;63:2019-2031.


223. Jalan R, Fernandez J, Wiest R, Schnabl B, Moreau R, Angeli P, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol 2014;60:1310-1324.


224. Wiest R, Krag A, Gerbes A. Spontaneous bacterial peritonitis: recent guidelines and beyond. Gut 2012;61:297-310.


225. Follo A, Llovet JM, Navasa M, Planas R, Forns X, Francitorra A, et al. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: incidence, clinical course, predictive factors and prognosis. Hepatology 1994;20:1495-1501.


226. Ruiz-del-Arbol L, Urman J, Fern├Īndez J, Gonz├Īlez M, Navasa M, Monescillo A, et al. Systemic, renal, and hepatic hemodynamic derangement in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology 2003;38:1210-1218.


229. de Araujo A, de Barros Lopes A, Rossi G, da Silva GV, Ananias P, Ness S, et al. Low-dose albumin in the treatment of spontaneous bacterial peritonitis: should we change the standard treatment? Gut 2012;61:1371-1372.


230. P├®rez-Paramo M, Mu├▒oz J, Albillos A, Freile I, Portero F, Santos M, et al. Effect of propranolol on the factors promoting bacterial translocation in cirrhotic rats with ascites. Hepatology 2000;31:43-48.


231. Senzolo M, Cholongitas E, Burra P, Leandro G, Thalheimer U, Patch D, et al. ╬▓-blockers protect against spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. Liver Int 2009;29:1189-1193.


232. Mandorfer M, Bota S, Schwabl P, Bucsics T, Pfisterer N, Kruzik M, et al. Nonselective ╬▓ blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology 2014;146:1680-1690 e1.


233. Madsen BS, Nielsen KF, Fialla AD, Krag A. Keep the sick from harm in spontaneous bacterial peritonitis: dose of beta blockers matters. J Hepatol 2016;64:1455-1456.


234. Runyon BA, Van Epps DE. Diuresis of cirrhotic ascites increases its opsonic activity and may help prevent spontaneous bacterial peritonitis. Hepatology 1986;6:396-399.


235. Runyon BA, Antillon MR, McHutchison JG. Diuresis increases ascitic fluid opsonic activity in patients who survive spontaneous bacterial peritonitis. J Hepatol 1992;14:249-252.


236. Bernard B, Grang├® JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology 1999;29:1655-1661.


237. Goulis J, Armonis A, Patch D, Sabin C, Greenslade L, Burroughs AK. Bacterial infection is independently associated with failure to control bleeding in cirrhotic patients with gastrointestinal hemorrhage. Hepatology 1998;27:1207-1212.


238. Vivas S, Rodriguez M, Palacio MA, Linares A, Alonso JL, Rodrigo L. Presence of bacterial infection in bleeding cirrhotic patients is independently associated with early mortality and failure to control bleeding. Dig Dis Sci 2001;46:2752-2757.


239. Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila F, Soares-Weiser K, Mendez-Sanchez N, Gluud C, et al. Meta-analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding - an updated Cochrane review. Aliment Pharmacol Ther 2011;34:509-518.


240. Soriano G, Guarner C, Tom├Īs A, Villanueva C, Torras X, Gonz├Īlez D, et al. Norfloxacin prevents bacterial infection in cirrhotics with gastrointestinal hemorrhage. Gastroenterology 1992;103:1267-1272.


241. Fern├Īndez J, Ruiz del Arbol L, G├│mez C, Durandez R, Serradilla R, Guarner C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology 2006;131:1049-1056 quiz 1285.


242. Llach J, Rimola A, Navasa M, Gin├©s P, Salmer├│n JM, Gin├©s A, et al. Incidence and predictive factors of first episode of spontaneous bacterial peritonitis in cirrhosis with ascites: relevance of ascitic fluid protein concentration. Hepatology 1992;16:724-727.


243. Andreu M, Sola R, Sitges-Serra A, Alia C, Gallen M, Vila MC, et al. Risk factors for spontaneous bacterial peritonitis in cirrhotic patients with ascites. Gastroenterology 1993;104:1133-1138.


244. Guarner C, Sol├Ā R, Soriano G, Andreu M, Novella MT, Vila MC, et al. Risk of a first community-acquired spontaneous bacterial peritonitis in cirrhotics with low ascitic fluid protein levels. Gastroenterology 1999;117:414-419.


245. Grang├® JD, Roulot D, Pelletier G, Pariente EA, Denis J, Ink O, et al. Norfloxacin primary prophylaxis of bacterial infections in cirrhotic patients with ascites: a double-blind randomized trial. J Hepatol 1998;29:430-436.


246. Terg R, Fassio E, Guevara M, Cartier M, Longo C, Lucero R, et al. Ciprofloxacin in primary prophylaxis of spontaneous bacterial peritonitis: a randomized, placebo-controlled study. J Hepatol 2008;48:774-779.


247. Fern├Īndez J, Navasa M, Planas R, Montoliu S, Monfort D, Soriano G, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology 2007;133:818-824.


248. Hanouneh MA, Hanouneh IA, Hashash JG, Law R, Esfeh JM, Lopez R, et al. The role of rifaximin in the primary prophylaxis of spontaneous bacterial peritonitis in patients with liver cirrhosis. J Clin Gastroenterol 2012;46:709-715.


249. Vlachogiannakos J, Viazis N, Vasianopoulou P, Vafiadis I, Karamanolis DG, Ladas SD. Long-term administration of rifaximin improves the prognosis of patients with decompensated alcoholic cirrhosis. J Gastroenterol Hepatol 2013;28:450-455.


250. Kang SH, Lee YB, Lee JH, Nam JY, Chang Y, Cho H, et al. Rifaximin treatment is associated with reduced risk of cirrhotic complications and prolonged overall survival in patients experiencing hepatic encephalopathy. Aliment Pharmacol Ther 2017;46:845-855.


252. Tit├│ L, Rimola A, Gin├©s P, Llach J, Arroyo V, Rod├®s J. Recurrence of spontaneous bacterial peritonitis in cirrhosis: frequency and predictive factors. Hepatology 1988;8:27-31.


253. Gin├®s P, Rimola A, Planas R, Vargas V, Marco F, Almela M, et al. Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology 1990;12(4 Pt 1):716-724.


254. Bauer TM, Follo A, Navasa M, Vila J, Planas R, Clemente G, et al. Daily norfloxacin is more effective than weekly rufloxacin in prevention of spontaneous bacterial peritonitis recurrence. Dig Dis Sci 2002;47:1356-1361.


255. Lontos S, Shelton E, Angus PW, Vaughan R, Roberts SK, Gordon A, et al. A randomized controlled study of trimethoprim-sulfamethoxazole versus norfloxacin for the prevention of infection in cirrhotic patients. J Dig Dis 2014;15:260-267.


256. Elfert A, Abo Ali L, Soliman S, Ibrahim S, Abd-Elsalam S. Randomized-controlled trial of rifaximin versus norfloxacin for secondary prophylaxis of spontaneous bacterial peritonitis. Eur J Gastroenterol Hepatol 2016;28:1450-1454.


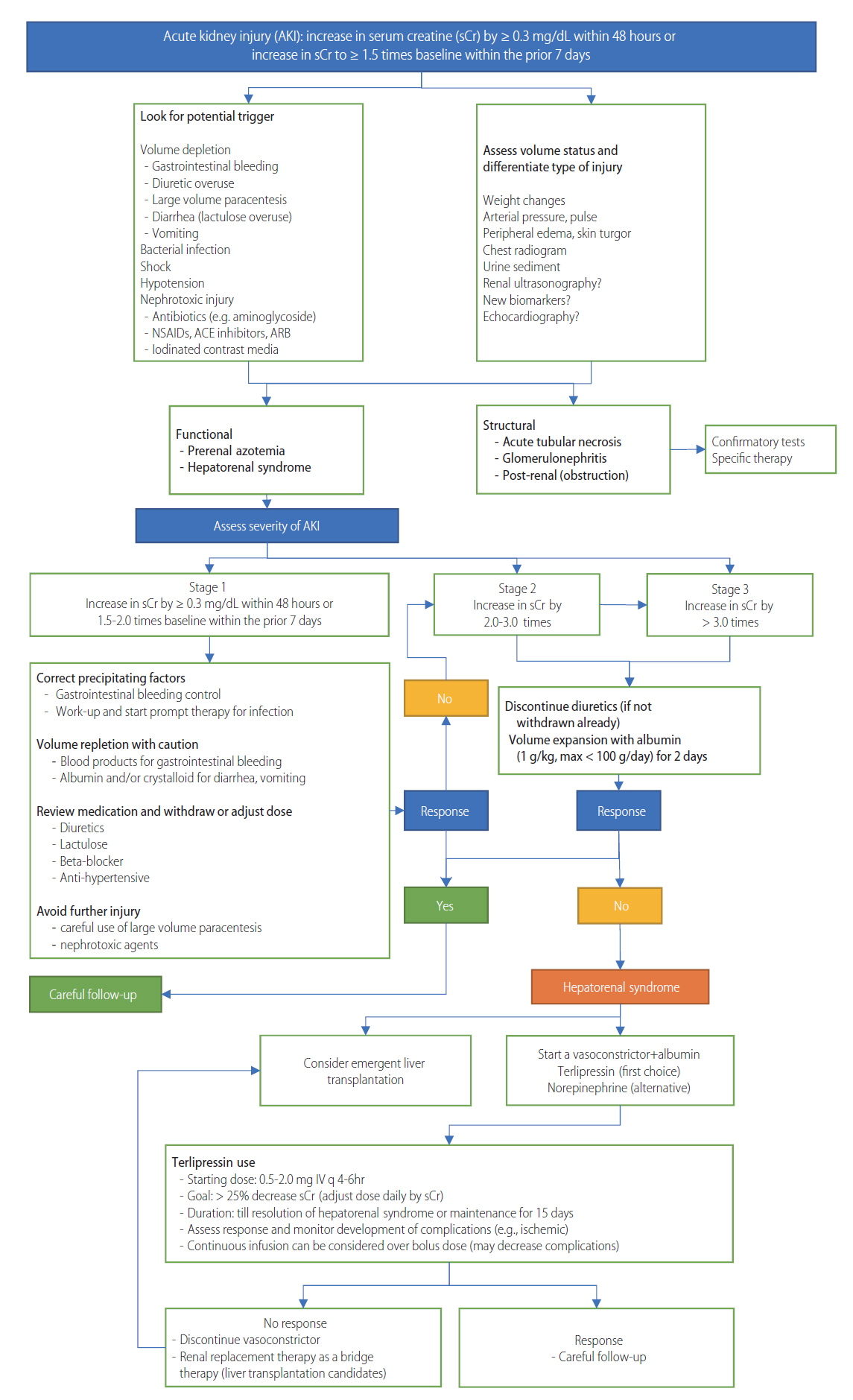
257. Garcia-Tsao G, Parikh CR, Viola A. Acute kidney injury in cirrhosis. Hepatology 2008;48:2064-2077.


259. C├Īrdenas A, Gin├©s P, Uriz J, Bessa X, Salmer├│n JM, Mas A, et al. Renal failure after upper gastrointestinal bleeding in cirrhosis: incidence, clinical course, predictive factors, and short-term prognosis. Hepatology 2001;34(4 Pt 1):671-676.


261. Bucsics T, Mandorfer M, Schwabl P, Bota S, Sieghart W, Ferlitsch A, et al. Impact of acute kidney injury on prognosis of patients with liver cirrhosis and ascites: a retrospective cohort study. J Gastroenterol Hepatol 2015;30:1657-1665.


262. Tsien CD, Rabie R, Wong F. Acute kidney injury in decompensated cirrhosis. Gut 2013;62:131-137.


264. Tan HK, Marguez M, Wong F, Renner EL. Pretransplant type 2 hepatorenal syndrome is associated with persistently impaired renal function after liver transplantation. Transplantation 2015;99:1441-1446.


265. Gonwa TA, Klintmalm GB, Levy M, Jennings LS, Goldstein RM, Husberg BS. Impact of pretransplant renal function on survival after liver transplantation. Transplantation 1995;59:361-365.


266. Warner NS, Cuthbert JA, Bhore R, Rockey DC. Acute kidney injury and chronic kidney disease in hospitalized patients with cirrhosis. J Investig Med 2011;59:1244-1251.


268. Schrier RW, Arroyo V, Bernardi M, Epstein M, Henriksen JH, Rod├®s J. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 1988;8:1151-1157.


269. Ruiz-del-Arbol L, Monescillo A, Arocena C, Valer P, Gin├©s P, Moreira V, et al. Circulatory function and hepatorenal syndrome in cirrhosis. Hepatology 2005;42:439-447.


270. Arroyo V, Colmenero J. Ascites and hepatorenal syndrome in cirrhosis: pathophysiological basis of therapy and current management. J Hepatol 2003;38 Suppl 1:S69-S89.


271. Ru├Łz-del-├ürbol L, Ach├®car L, Serradilla R, Rodr├Łguez-Gand├Ła M├ü, Rivero M, Garrido E, et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology 2013;58:1732-1741.


272. Acevedo J, Fern├Īndez J, Prado V, Silva A, Castro M, Pavesi M, et al. Relative adrenal insufficiency in decompensated cirrhosis: relationship to short-term risk of severe sepsis, hepatorenal syndrome, and death. Hepatology 2013;58:1757-1765.


277. Orlando R, Floreani M, Padrini R, Palatini P. Evaluation of measured and calculated creatinine clearances as glomerular filtration markers in different stages of liver cirrhosis. Clin Nephrol 1999;51:341-347.

278. Sherman DS, Fish DN, Teitelbaum I. Assessing renal function in cirrhotic patients: problems and pitfalls. Am J Kidney Dis 2003;41:269-278.


279. Caregaro L, Menon F, Angeli P, Amodio P, Merkel C, Bortoluzzi A, et al. Limitations of serum creatinine level and creatinine clearance as filtration markers in cirrhosis. Arch Intern Med 1994;154:201-205.


280. Spencer K. Analytical reviews in clinical biochemistry: the estimation of creatinine. Ann Clin Biochem 1986;23(Pt 1):1-25.


282. Angeli P, Gines P, Wong F, Bernardi M, Boyer TD, Gerbes A, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. Gut 2015;64:531-537.


284. Jenq CC, Tsai MH, Tian YC, Lin CY, Yang C, Liu NJ, et al. RIFLE classification can predict short-term prognosis in critically ill cirrhotic patients. Intensive Care Med 2007;33:1921-1930.


285. Cholongitas E, Calvaruso V, Senzolo M, Patch D, Shaw S, OŌĆÖBeirne J, et al. RIFLE classification as predictive factor of mortality in patients with cirrhosis admitted to intensive care unit. J Gastroenterol Hepatol 2009;24:1639-1647.


287. Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 2004;15:1597-1605.


288. Tu KH, Jenq CC, Tsai MH, Hsu HH, Chang MY, Tian YC, et al. Outcome scoring systems for short-term prognosis in critically ill cirrhotic patients. Shock 2011;36:445-450.


289. Radhakrishnan J, Cattran DC. The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines--application to the individual patient. Kidney Int 2012;82:840-856.


291. Angeli P, Gatta A, Caregaro L, Menon F, Sacerdoti D, Merkel C, et al. Tubular site of renal sodium retention in ascitic liver cirrhosis evaluated by lithium clearance. Eur J Clin Invest 1990;20:111-117.


292. Francoz C, Pri├® D, Abdelrazek W, Moreau R, Mandot A, Belghiti J, et al. Inaccuracies of creatinine and creatinine-based equations in candidates for liver transplantation with low creatinine: impact on the model for end-stage liver disease score. Liver Transpl 2010;16:1169-1177.


293. Rosi S, Piano S, Frigo AC, Morando F, Fasolato S, Cavallin M, et al. New ICA criteria for the diagnosis of acute kidney injury in cirrhotic patients: can we use an imputed value of serum creatinine? Liver Int 2015;35:2108-2114.


295. Trawal├® JM, Paradis V, Rautou PE, Francoz C, Escolano S, Sall├®e M, et al. The spectrum of renal lesions in patients with cirrhosis: a clinicopathological study. Liver Int 2010;30:725-732.


297. Rodr├Łguez E, Elia C, Sol├Ā E, Barreto R, Graupera I, Andrealli A, et al. Terlipressin and albumin for type-1 hepatorenal syndrome associated with sepsis. J Hepatol 2014;60:955-961.


298. Th├®venot T, Bureau C, Oberti F, Anty R, Louvet A, Plessier A, et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol 2015;62:822-830.


301. Sola-Vera J, Mi├▒ana J, Ricart E, Planella M, Gonz├Īlez B, Torras X, et al. Randomized trial comparing albumin and saline in the prevention of paracentesis-induced circulatory dysfunction in cirrhotic patients with ascites. Hepatology 2003;37:1147-1153.


302. Elia C, Graupera I, Barreto R, Sol├Ā E, Moreira R, Huelin P, et al. Severe acute kidney injury associated with non-steroidal anti-inflammatory drugs in cirrhosis: a case-control study. J Hepatol 2015;63:593-600.


303. Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology 2000;119:1637-1648.


304. Thursz MR, Richardson P, Allison M, Austin A, Bowers M, Day CP, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med 2015;372:1619-1628.


309. Garcia-Martinez R, Caraceni P, Bernardi M, Gines P, Arroyo V, Jalan R. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology 2013;58:1836-1846.


310. Garcia-Martinez R, Noiret L, Sen S, Mookerjee R, Jalan R. Albumin infusion improves renal blood flow autoregulation in patients with acute decompensation of cirrhosis and acute kidney injury. Liver Int 2015;35:335-343.


311. Neri S, Pulvirenti D, Malaguarnera M, Cosimo BM, Bertino G, Ignaccolo L, et al. Terlipressin and albumin in patients with cirrhosis and type I hepatorenal syndrome. Dig Dis Sci 2008;53:830-835.


312. Mart├Łn-Llah├Ł M, P├®pin MN, Guevara M, D├Łaz F, Torre A, Monescillo A, et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: a randomized study. Gastroenterology 2008;134:1352-1359.


313. Ortega R, Gin├©s P, Uriz J, C├Īrdenas A, Calahorra B, De Las Heras D, et al. Terlipressin therapy with and without albumin for patients with hepatorenal syndrome: results of a prospective, nonrandomized study. Hepatology 2002;36(4 Pt 1):941-948.


314. Rodriguez E, Henrique Pereira G, Sol├Ā E, Elia C, Barreto R, Pose E, et al. Treatment of type 2 hepatorenal syndrome in patients awaiting transplantation: effects on kidney function and transplantation outcomes. Liver Transpl 2015;21:1347-1354.


317. Egerod Israelsen M, Gluud LL, Krag A. Acute kidney injury and hepatorenal syndrome in cirrhosis. J Gastroenterol Hepatol 2015;30:236-243.


318. Cavallin M, Piano S, Romano A, Fasolato S, Frigo AC, Benetti G, et al. Terlipressin given by continuous intravenous infusion versus intravenous boluses in the treatment of hepatorenal syndrome: a randomized controlled study. Hepatology 2016;63:983-992.


319. Nazar A, Pereira GH, Guevara M, Mart├Łn-Llahi M, Pepin MN, Marinelli M, et al. Predictors of response to therapy with terlipressin and albumin in patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 2010;51:219-226.


320. Facciorusso A, Chandar AK, Murad MH, Prokop LJ, Muscatiello N, Kamath PS, et al. Comparative efficacy of pharmacological strategies for management of type 1 hepatorenal syndrome: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol 2017;2:94-102.


321. Sharma P, Kumar A, Shrama BC, Sarin SK. An open label, pilot, randomized controlled trial of noradrenaline versus terlipressin in the treatment of type 1 hepatorenal syndrome and predictors of response. Am J Gastroenterol 2008;103:1689-1697.


322. Singh V, Ghosh S, Singh B, Kumar P, Sharma N, Bhalla A, et al. Noradrenaline vs. terlipressin in the treatment of hepatorenal syndrome: a randomized study. J Hepatol 2012;56:1293-1298.


324. Nadim MK, Durand F, Kellum JA, Levitsky J, OŌĆÖLeary JG, Karvellas CJ, et al. Corrigendum to ŌĆ£Management of the critically ill patients with cirrhosis: a multidisciplinary perspectiveŌĆØ. J Hepatol 2016 May 27. pii: S0168-8278(16)30185-4. doi:
10.1016/j.jhep.2016.05.001. [Epub ahead of print].

325. Wong F, Pantea L, Sniderman K. Midodrine, octreotide, albumin, and TIPS in selected patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 2004;40:55-64.


326. Esrailian E, Pantangco ER, Kyulo NL, Hu KQ, Runyon BA. Octreotide/midodrine therapy significantly improves renal function and 30-day survival in patients with type 1 hepatorenal syndrome. Dig Dis Sci 2007;52:742-748.


327. Skagen C, Einstein M, Lucey MR, Said A. Combination treatment with octreotide, midodrine, and albumin improves survival in patients with type 1 and type 2 hepatorenal syndrome. J Clin Gastroenterol 2009;43:680-685.


328. Cavallin M, Kamath PS, Merli M, Fasolato S, Toniutto P, Salerno F, et al. Terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: a randomized trial. Hepatology 2015;62:567-574.


329. Wong LP, Blackley MP, Andreoni KA, Chin H, Falk RJ, Klemmer PJ. Survival of liver transplant candidates with acute renal failure receiving renal replacement therapy. Kidney Int 2005;68:362-370.


330. Zhang Z, Maddukuri G, Jaipaul N, Cai CX. Role of renal replacement therapy in patients with type 1 hepatorenal syndrome receiving combination treatment of vasoconstrictor plus albumin. J Crit Care 2015;30:969-974.


331. Guevara M, Gin├©s P, Bandi JC, Gilabert R, Sort P, Jim├®nez W, et al. Transjugular intrahepatic portosystemic shunt in hepatorenal syndrome: effects on renal function and vasoactive systems. Hepatology 1998;28:416-422.


332. R├Čssle M, Gerbes AL. TIPS for the treatment of refractory ascites, hepatorenal syndrome and hepatic hydrothorax: a critical update. Gut 2010;59:988-1000.


334. Senzolo M, Cholongitas E, Tibballs J, Burroughs A, Patch D. Transjugular intrahepatic portosystemic shunt in the management of ascites and hepatorenal syndrome. Eur J Gastroenterol Hepatol 2006;18:1143-1150.


335. Wong F, Sniderman K, Liu P, Allidina Y, Sherman M, Blendis L. Transjugular intrahepatic portosystemic stent shunt: effects on hemodynamics and sodium homeostasis in cirrhosis and refractory ascites. Ann Intern Med 1995;122:816-822.


336. Trebicka J. Emergency TIPS in a child-pugh B patient: when does the window of opportunity open and close? J Hepatol 2017;66:442-450.


337. Jalan R, Sen S, Steiner C, Kapoor D, Alisa A, Williams R. Extracorporeal liver support with molecular adsorbents recirculating system in patients with severe acute alcoholic hepatitis. J Hepatol 2003;38:24-31.


338. Mitzner SR, Stange J, Klammt S, Risler T, Erley CM, Bader BD, et al. Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: results of a prospective, randomized, controlled clinical trial. Liver Transpl 2000;6:277-286.


339. Wong F, Raina N, Richardson R. Molecular adsorbent recirculating system is ineffective in the management of type 1 hepatorenal syndrome in patients with cirrhosis with ascites who have failed vasoconstrictor treatment. Gut 2010;59:381-386.


340. Nair S, Verma S, Thuluvath PJ. Pretransplant renal function predicts survival in patients undergoing orthotopic liver transplantation. Hepatology 2002;35:1179-1185.


342. Wong F, Leung W, Al Beshir M, Marquez M, Renner EL. Outcomes of patients with cirrhosis and hepatorenal syndrome type 1 treated with liver transplantation. Liver Transpl 2015;21:300-307.


344. Goldaracena N, Marquez M, Selzner N, Spetzler VN, Cattral MS, Greig PD, et al. Living vs. deceased donor liver transplantation provides comparable recovery of renal function in patients with hepatorenal syndrome: a matched case-control study. Am J Transplant 2014;14:2788-2795.


345. Lee JP, Kwon HY, Park JI, Yi NJ, Suh KS, Lee HW, et al. Clinical outcomes of patients with hepatorenal syndrome after living donor liver transplantation. Liver Transpl 2012;18:1237-1244.


346. Malagari K, Nikita A, Alexopoulou E, Brountzos E, Papathanasiou M, Mitromaras J, et al. Cirrhosis-related intrathoracic disease. Imaging features in 1038 patients. Hepatogastroenterology 2005;52:558-562.

348. Huang PM, Chang YL, Yang CY, Lee YC. The morphology of diaphragmatic defects in hepatic hydrothorax: thoracoscopic finding. J Thorac Cardiovasc Surg 2005;130:141-145.


349. Machicao VI, Balakrishnan M, Fallon MB. Pulmonary complications in chronic liver disease. Hepatology 2014;59:1627-1637.


350. Mirouze D, Juttner HU, Reynolds TB. Left pleural effusion in patients with chronic liver disease and ascites. Prospective study of 22 cases. Dig Dis Sci 1981;26:984-988.


351. Xiol X, Castellote J, Cortes-Beut R, Delgado M, Guardiola J, Ses├® E. Usefulness and complications of thoracentesis in cirrhotic patients. Am J Med 2001;111:67-69.


353. Xiol X, Castellvi JM, Guardiola J, Ses├® E, Castellote J, Perell├│ A, et al. Spontaneous bacterial empyema in cirrhotic patients: a prospective study. Hepatology 1996;23:719-723.


354. Chen TA, Lo GH, Lai KH. Risk factors for spontaneous bacterial empyema in cirrhotic patients with hydrothorax. J Chin Med Assoc 2003;66:579-586.

355. Sese E, Xiol X, Castellote J, Rodr├Łguez-Fari├▒as E, Tremosa G. Low complement levels and opsonic activity in hepatic hydrothorax: its relationship with spontaneous bacterial empyema. J Clin Gastroenterol 2003;36:75-77.


356. Xiol X, Tremosa G, Castellote J, Gornals J, Lama C, Lopez C, et al. Liver transplantation in patients with hepatic hydrothorax. Transpl Int 2005;18:672-675.


357. Feller-Kopman D, Berkowitz D, Boiselle P, Ernst A. Large-volume thoracentesis and the risk of reexpansion pulmonary edema. Ann Thorac Surg 2007;84:1656-1661.


358. Siegerstetter V, Deibert P, Ochs A, Olschewski M, Blum HE, R├Čssle M. Treatment of refractory hepatic hydrothorax with transjugular intrahepatic portosystemic shunt: long-term results in 40 patients. Eur J Gastroenterol Hepatol 2001;13:529-534.


359. Gordon FD, Anastopoulos HT, Crenshaw W, Gilchrist B, McEniff N, Falchuk KR, et al. The successful treatment of symptomatic, refractory hepatic hydrothorax with transjugular intrahepatic portosystemic shunt. Hepatology 1997;25:1366-1369.


361. Spencer EB, Cohen DT, Darcy MD. Safety and efficacy of transjugular intrahepatic portosystemic shunt creation for the treatment of hepatic hydrothorax. J Vasc Interv Radiol 2002;13:385-390.


362. Chalasani N, Clark WS, Martin LG, Kamean J, Khan MA, Patel NH, et al. Determinants of mortality in patients with advanced cirrhosis after transjugular intrahepatic portosystemic shunting. Gastroenterology 2000;118:138-144.


363. Milanez de Campos JR, Filho LO, de Campos Werebe E, Sette H Jr, Fernandez A, Filomeno LT, et al. Thoracoscopy and talc poudrage in the management of hepatic hydrothorax. Chest 2000;118:13-17.


364. Ferrante D, Arguedas MR, Cerfolio RJ, Collins BG, van Leeuwen DJ. Video-assisted thoracoscopic surgery with talc pleurodesis in the management of symptomatic hepatic hydrothorax. Am J Gastroenterol 2002;97:3172-3175.


365. Runyon BA, Greenblatt M, Ming RH. Hepatic hydrothorax is a relative contraindication to chest tube insertion. Am J Gastroenterol 1986;81:566-567.

367. Singh A, Bajwa A, Shujaat A. Evidence-based review of the management of hepatic hydrothorax. Respiration 2013;86:155-173.


368. Baker EM, Melander S. Management of recurrent pleural effusions with a tunneled catheter. Heart Lung 2010;39:314-318.


369. Chalhoub M, Harris K, Castellano M, Maroun R, Bourjeily G. The use of the pleurX catheter in the management of non-malignant pleural effusions. Chron Respir Dis 2011;8:185-191.


370. Herlihy JP, Loyalka P, Gnananandh J, Gregoric ID, Dahlberg CG, Kar B, et al. PleurX catheter for the management of refractory pleural effusions in congestive heart failure. Tex Heart Inst J 2009;36:38-43.


372. Odom SR, Gupta A, Talmor D, Novack V, Sagy I, Evenson AR. Emergency hernia repair in cirrhotic patients with ascites. J Trauma Acute Care Surg 2013;75:404-409.


375. Runyon BA, Juler GL. Natural history of repaired umbilical hernias in patients with and without ascites. Am J Gastroenterol 1985;80:38-39.

376. Telem DA, Schiano T, Divino CM. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery 2010;148:538-543.


377. Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis - a practical guide. Aliment Pharmacol Ther 2013;37:1132-1156.


378. Verbeeck RK. Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol 2008;64:1147-1161.


379. Elbekai RH, Korashy HM, El-Kadi AO. The effect of liver cirrhosis on the regulation and expression of drug metabolizing enzymes. Curr Drug Metab 2004;5:157-167.


380. Kr├żhenb├╝hl S, Reichen J. Pharmacokinetics and pharmacodynamics in cirrhosis. Medicine 2002;30:24-27.

381. Villeneuve JP, Verbeeck RK, Wilkinson GR, Branch RA. Furosemide kinetics and dynamics in patients with cirrhosis. Clin Pharmacol Ther 1986;40:14-20.


382. Chalasani N, Gorski JC, Patel NH, Hall SD, Galinsky RE. Hepatic and intestinal cytochrome P450 3A activity in cirrhosis: effects of transjugular intrahepatic portosystemic shunts. Hepatology 2001;34:1103-1108.


383. Vuppalanchi R, Juluri R, Ghabril M, Kim S, Thong N, Gorski JC, et al. Drug-induced QT prolongation in cirrhotic patients with transjugular intrahepatic portosystemic shunt. J Clin Gastroenterol 2011;45:638-642.


385. Ahn BM. Acetaminophen-induced acute hepatic failure. J Korean Med Assoc 2006;49:846-883.

386. Manyike PT, Kharasch ED, Kalhorn TF, Slattery JT. Contribution of CYP2E1 and CYP3A to acetaminophen reactive metabolite formation. Clin Pharmacol Ther 2000;67:275-282.


389. Bosilkovska M, Walder B, Besson M, Daali Y, Desmeules J. Analgesics in patients with hepatic impairment: pharmacology and clinical implications. Drugs 2012;72:1645-1669.


390. Cl├Āria J, Kent JD, L├│pez-Parra M, Escolar G, Ruiz-Del-Arbol L, Gin├©s P, et al. Effects of celecoxib and naproxen on renal function in nonazotemic patients with cirrhosis and ascites. Hepatology 2005;41:579-587.


391. Williams RL, Upton RA, Cello JP, Jones RM, Blitstein M, Kelly J, et al. Naproxen disposition in patients with alcoholic cirrhosis. Eur J Clin Pharmacol 1984;27:291-296.


392. Hayes PC, Davis JM, Lewis JA, Bouchier IA. Meta-analysis of value of propranolol in prevention of variceal haemorrhage. Lancet 1990;336:153-156.


394. Ge PS, Runyon BA. The changing role of beta-blocker therapy in patients with cirrhosis. J Hepatol 2014;60:643-653.


395. Leithead JA, Rajoriya N, Tehami N, Hodson J, Gunson BK, Tripathi D, et al. Non-selective ╬▓-blockers are associated with improved survival in patients with ascites listed for liver transplantation. Gut 2015;64:1111-1119.


396. Mookerjee RP, Pavesi M, Thomsen KL, Mehta G, Macnaughtan J, Bendtsen F, et al. Treatment with non-selective beta-blockers is associated with reduced severity of systemic inflammation and improved survival of patients with acute-on-chronic liver failure. J Hepatol 2016;64:574-582.


397. Franz CC, Egger S, Born C, R├żtz Bravo AE, Kr├żhenb├╝hl S. Potential drug-drug interactions and adverse drug reactions in patients with liver cirrhosis. Eur J Clin Pharmacol 2012;68:179-188.


399. Gentilini P, Romanelli RG, La Villa G, Maggiore Q, Pesciullesi E, Cappelli G, et al. Effects of low-dose captopril on renal hemodynamics and function in patients with cirrhosis of the liver. Gastroenterology 1993;104:588-594.


400. Pariente EA, Bataille C, Bercoff E, Lebrec D. Acute effects of captopril on systemic and renal hemodynamics and on renal function in cirrhotic patients with ascites. Gastroenterology 1985;88(5 Pt 1):1255-1259.


401. Lewis JH, Mortensen ME, Zweig S, Fusco MJ, Medoff JR, Belder R, et al. Efficacy and safety of high-dose pravastatin in hypercholesterolemic patients with well-compensated chronic liver disease: results of a prospective, randomized, double-blind, placebo-controlled, multicenter trial. Hepatology 2007;46:1453-1463.


402. Athyros VG, Tziomalos K, Gossios TD, Griva T, Anagnostis P, Kargiotis K, et al. Safety and efficacy of long-term statin treatment for cardiovascular events in patients with coronary heart disease and abnormal liver tests in the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) Study: a post-hoc analysis. Lancet 2010;376:1916-1922.


403. Chang FM, Wang YP, Lang HC, Tsai CF, Hou MC, Lee FY, et al. Statins decrease the risk of decompensation in hepatitis B virus- and hepatitis C virus-related cirrhosis: a population-based study. Hepatology 2017;66:896-907.


406. Tsan YT, Lee CH, Wang JD, Chen PC. Statins and the risk of hepatocellular carcinoma in patients with hepatitis B virus infection. J Clin Oncol 2012;30:623-630.


407. Abraldes JG, Villanueva C, Aracil C, Turnes J, Hernandez-Guerra M, Genesca J, et al. Addition of simvastatin to standard therapy for the prevention of variceal rebleeding does not reduce rebleeding but increases survival in patients with cirrhosis. Gastroenterology 2016;150:1160-1170 e3.


408. Drug Information Handbook. 26th ed. Hudson: Wolters Kluwer Clinical Drug Information, Inc.; 2017.
409. Dam G, Vilstrup H, Watson H, Jepsen P. Proton pump inhibitors as a risk factor for hepatic encephalopathy and spontaneous bacterial peritonitis in patients with cirrhosis with ascites. Hepatology 2016;64:1265-1272.


411. Goel GA, Deshpande A, Lopez R, Hall GS, van Duin D, Carey WD. Increased rate of spontaneous bacterial peritonitis among cirrhotic patients receiving pharmacologic acid suppression. Clin Gastroenterol Hepatol 2012;10:422-427.


412. Deshpande A, Pant C, Pasupuleti V, Rolston DD, Jain A, Deshpande N, et al. Association between proton pump inhibitor therapy and Clostridium difficile infection in a meta-analysis. Clin Gastroenterol Hepatol 2012;10:225-233.


414. Tsai CF, Chen MH, Wang YP, Chu CJ, Huang YH, Lin HC, et al. Proton pump inhibitors increase risk for hepatic encephalopathy in patients with cirrhosis in a population study. Gastroenterology 2017;152:134-141.


415. Vaezi MF, Yang YX, Howden CW. Complications of proton pump inhibitor therapy. Gastroenterology 2017;153:35-48.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Supplement1
Supplement1 Print
Print




