| Clin Mol Hepatol > Volume 28(2); 2022 > Article |
|
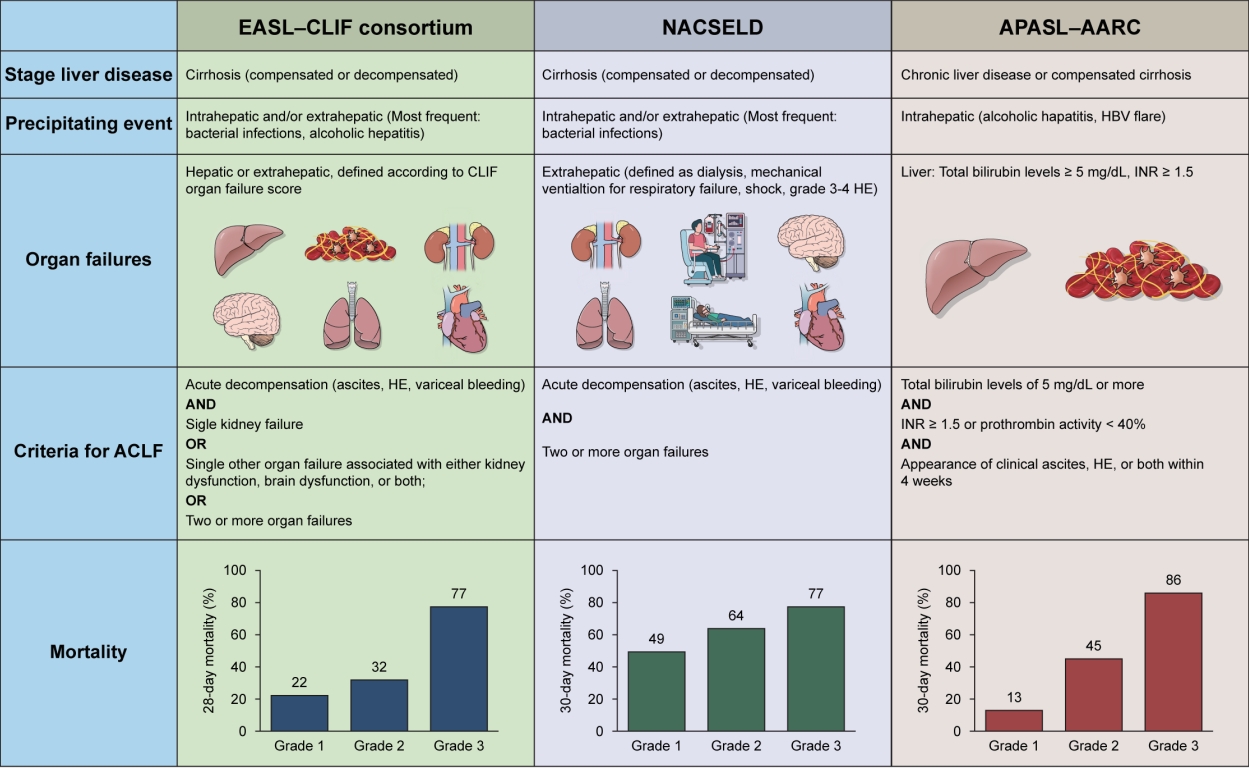
Acute-on-chronic liver failure (ACLF) is a syndrome characterized by an acute decompensation (AD) of chronic liver disease associated with organ failures (OFs; hepatic and/or extrahepatic) [1-3]. ACLF is characterized by a high short-term mortality, but it is potentially reversible. Moreover, ACLF is frequently associated with a precipitating event which can be either hepatic or extrahepatic [2,4]. Systemic inflammation is considered a main driver of the syndrome and responsible for the occurrence of OFs [5]. Unfortunately, there is no unanimous consensus definition of ACLF. At least three different definitions are available from Europe, Asia and North America. Those definitions differ in the baseline stage of liver disease, type of precipitating events, type and definition of OFs.
European Association for the Study of the Liver (EASL)-chronic liver failure (CLIF) consortium proposed a definition based on the results of the CANONIC study [1]. According to EASL-CLIF consortium, ACLF is defined by an AD of cirrhosis (occurring of variceal bleeding, ascites, hepatic encephalopathy [HE]) associated with hepatic or extrahepatic OFs. OFs definition is based on a modified Sequential Organ Failure Assessment (SOFA) score, called CLIF-C OF, which considers the function of six systems (liver, kidney, brain, coagulation, circulation and respiration) [1].
According to the number of OFs, patients with ACLF are stratified into three groups at increasing risk of mortality: 1) ACLF grade 1, patients with a single kidney failure or another single OF if associated with brain or kidney disfunction; 2) ACLF grade 2, patients with two OFs; and 3) ACLF grade 3, patients with three or more OFs.
In EASL-CLIF definition, both hepatic and extra-hepatic factors are considered as precipitants for ACLF, the most frequent being bacterial infections and alcoholic hepatitis [4,6].
North American Consortium for the Study of End-stage Liver Disease (NACSELD) based its definition for ACLF on a clinical study involving 507 cirrhotic patients hospitalized for AD and bacterial infections [3]. ACLF is defined according to the presence of two or more extrahepatic OFs (kidney, brain, circulation and respiration) and patients can be stratified in three groups according to the number of OFs.
The third definition, which is actually the first in chronological order, is the one proposed by the Asian Pacific Association for the Study of the Liver (APASL) in 2009 and modified in 2014 and 2019 by the APASL ACLF Research Consortium (AARC). AARC definition considers extra-hepatic OFs as manifestations of ACLF but not as determinants of the syndrome. ACLF is considered as an acute deterioration of liver function, defined by the appearance of jaundice (with total bilirubin levels Ōēź5 mg/dL), coagulation failure (international normalized ratio [INR] Ōēź1.5 or prothrombin activity <40%), occurring in patients with chronic liver disease or compensated cirrhosis as a consequence of a hepatic insult (e.g., hepatitis B virus-reactivation or acute alcoholic hepatitis), that is complicated by clinically evident ascites, encephalopathy or both within 4 weeks [2]. Patients with decompensated cirrhosis are not only in patients with without prior decompensation and with no AD. In these patients, the severity of ACLF is assessed using the AARC score, which evaluates severity of ACLF according to the levels of total bilirubin, encephalopathy grade, INR, serum creatinine and lactates [7].
Differences in diagnostic criteria lead to different clinical characteristics and epidemiology of ACLF [8]. A meta-analysis of cohort studies found a prevalence of ACLF (EASL-CLIF definition) of 35% in hospitalized patients with cirrhosis [9], while its incidence in cirrhotic outpatients is about 40% at 10 years [10]. Patients with EASL-CLIF ACLF are characterized by a severe systemic inflammation, circulatory dysfunction and oxidative stress [11,12]. Patients with APASL-AARC ACLF have more severe liver failure and coagulation failure, while sepsis can frequently complicate the clinical course of APASL-ACLF [7].
All these definitions have both strengths and limitations, and a shared definition of ACLF would be highly desirable. However, the research in ACLF field has led to important advancements in our understanding of clinical course of cirrhosis and helped to identify patients at high risk of mortality. Indeed, whatever is the definition used, ACLF has a tremendous impact on short-term mortality. Patients with ACLF deserve an aggressive management, including early identification and treatment of precipitating events, prevention and treatment of infections, expedite management of OFs and urgent referral for liver transplantation.
FOOTNOTES
Abbreviations
AARC
APASL ACLF Research Consortium
ACLF
acute-on-chronic liver failure
AD
acute decompensation
APASL
Asian Pacific Association for the Study of the Liver
CLIF
chronic liver failure
EASl
European Association for the Study of the Liver
HE
hepatic encephalopathy
INR
international normalized ratio
NACSELD
North American Consortium for the Study of End-stage Liver Disease
OFs
organ failures
SOFA
Sequential Organ Failure Assessment
REFERENCES
1. Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426-1437 1437.e1-e9.


2. Sarin SK, Choudhury A, Sharma MK, Maiwall R, Al Mahtab M, Rahman S, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int 2019;13:353-390.

3. Bajaj JS, OŌĆÖLeary JG, Reddy KR, Wong F, Biggins SW, Patton H, et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology 2014;60:250-256.



4. Trebicka J, Fernandez J, Papp M, Caraceni P, Laleman W, Gambino C, et al. PREDICT identifies precipitating events associated with the clinical course of acutely decompensated cirrhosis. J Hepatol 2021;74:1097-1108.

5. Arroyo V, Angeli P, Moreau R, Jalan R, Cl├Āria J, Trebicka J, et al. The systemic inflammation hypothesis: towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis. J Hepatol 2021;74:670-685.


6. Wong F, Piano S, Singh V, Bartoletti M, Maiwall R, Alessandria C, et al. Clinical features and evolution of bacterial infection-related acute-on-chronic liver failure. J Hepatol 2021;74:330-339.


7. Choudhury A, Jindal A, Maiwall R, Sharma MK, Sharma BC, Pamecha V, et al. Liver failure determines the outcome in patients of acute-on-chronic liver failure (ACLF): comparison of APASL ACLF research consortium (AARC) and CLIF-SOFA models. Hepatol Int 2017;11:461-471.


8. Mahmud N, Kaplan DE, Taddei TH, Goldberg DS. Incidence and mortality of acute-on-chronic liver failure using two definitions in patients with compensated cirrhosis. Hepatology 2019;69:2150-2163.



9. Mezzano G, Juanola A, Cardenas A, Mezey E, Hamilton JP, Pose E, et al. Global burden of disease: acute-on-chronic liver failure, a systematic review and meta-analysis. Gut 2022;71:148-155.


10. Piano S, Tonon M, Vettore E, Stanco M, Pilutti C, Romano A, et al. Incidence, predictors and outcomes of acute-on-chronic liver failure in outpatients with cirrhosis. J Hepatol 2017;67:1177-1184.


- TOOLS
-
METRICS

- ORCID iDs
-
Salvatore Piano

https://orcid.org/0000-0002-9356-5830 - Related articles
-
Acute-on-chronic liver failure: Terminology, mechanisms and management2023 July;29(3)
Epidemiology of alcoholic liver disease in Korea2018 June;24(2)
Acute-on-chronic liver failure: a new syndrome in cirrhosis2016 March;22(1)
The use of vaptan in hyponatremic patients with liver cirrhosis2011 December;17(4)
A case of variceal bleeding from the jejunum in liver cirrhosis2013 March;19(1)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



