| Clin Mol Hepatol > Volume 26(4); 2020 > Article |
|
ABSTRACT
Alcohol is a well-known risk factor for premature morbidity and mortality. The per capita alcohol consumption of the worldŌĆÖs population rose from 5.5 L in 2005 to 6.4 L in 2010 and was still at the level of 6.4 L in 2016. Alcohol-attributable deaths and disability-adjusted life years (DALYs) declined from 2000 to 2016 by 17.9% and 14.5%, respectively. However, these gains observed in the alcohol-attributable burden have proportionally not kept pace with the total health gains during the same period. In 2016, 3.0 million deaths worldwide and 132 million DALYs were attributable to alcohol, responsible for 5.3% of all deaths and 5.0% of all DALYs. These burdens are the highest in the regions of Eastern Europe and sub-Saharan Africa. The alcohol-attributable burden is particularly heavy among young adults, accounting for 7.2% of all premature mortalities. Among the disease categories to which alcohol is related, injuries, digestive diseases, and cardiovascular diseases are the leading causes of the alcohol-attributable burden. To reduce the harmful use of alcohol in a country, the ŌĆśwhole of governmentŌĆÖ and ŌĆśwhole of societyŌĆÖ approaches are required with the implementation of evidence-based alcohol control policies, the pursuit of public health priorities, and the adoption of appropriate policies over a long period of time. In this review, we summarize previous efforts to investigate the alcohol-attributable disease burden and the best ways to protect against harmful use of alcohol and promote health.
Humans have been consuming fermented alcoholic beverages for more than 10,000 years, primarily to obtain safe drinking water and avoid bacterial contamination [1]. Alcoholic beverages are consumed widely throughout the world, and the health effect of alcohol use can have substantial public health implications [2]. Alcohol is responsible for tremendous perturbations in social and physical well-being worldwide and has been estimated to be the seventh leading risk factor for both morbidity and mortality [3].
A world leading medical journal has been publishing articles describing the ŌĆśsuperhumanŌĆÖ efforts to address the Global Burden of Disease (GBD) since 2010 [4]. This brief communication highlights that alcohol use is a major contributor to injuries, mortality, and the burden of disease, especially among the population aged 15ŌĆō49 years [5-8]. These findings provide a complementary picture to that obtained from the ŌĆśGlobal Status Report on Alcohol and Health 2018ŌĆÖ [9], published by the World Health Organization (WHO). Throughout the manuscript, we mainly use data from the WHO and the GBD.
In this review, we summarize previous efforts to investigate alcohol-attributable disease burden based on deaths and disability-adjusted life-years (DALYs) and the best ways to protect against harmful use of alcohol and promote health.
The total burden attributable to alcohol use is larger than previous evidence has shown and increases with consumption [6]. Alcohol has a monotonic association with some cancers (oropharynx, larynx, esophagus, liver, etc.) but is reportedly associated with protection against diabetes, ischemic stroke, or coronary heart disease when consumed at a moderate level [10,11]. A shortage of estimates from observational studies identifying appropriate reference categories, adequately accounting for survival bias and other residual confounders, may lead to potential overestimation of the protective effects from light or moderate alcohol intake (Ōēż14 standard drinks/week for male and Ōēż7 standard drinks/week for female) [12]. Emerging research with methodological enhancements, including Mendelian randomization, pooled cohort studies, and multivariable adjusted meta-analyses, has shown no beneficial effect of alcohol consumption on mortality or cardiovascular outcomes [13,14]. In line with recent literature, a GBD study presents empirical evidence that there is no safe level of alcohol consumption [6]. Based on weighted relative risk curves for each health outcome associated with alcohol use, the level of consumption that minimizes health loss due to alcohol use is zero [6]. These new findings strongly suggest that alcohol policies aimed at total population-level consumption are needed to reduce the burden attributable to alcohol in a population [6].
In 2016, 32.5% of people worldwide were current drinkers [6]. Twenty-five percent of women are current drinkers, as are 39% of men in the previous 12 months (Table 1) [6]. The per capita alcohol consumption in the worldŌĆÖs population rose from 5.5 L of alcohol in 2005 to 6.4 L in 2010 [9], and it is expected to reach 7.6 L by 2030 [15]. The amount of alcohol consumed varies considerably by region and socio-demographic index (SDI), which reflects overall development [6]. The countries with the highest level of alcohol consumption are in the Eastern European region and have high SDI locations [6]. While alcohol consumption has been decreasing in the Western European region, it is increasing in the Western Pacific and South-East Asian regions, including the highly populated countries of China and India, which account for the increases (China: 4.1 L and 7.2 L in 2005 and 2016, respectively; India: 2.4 L and 5.7 L in 2005 and 2016, respectively) [9].
The prevalence of heavy episodic drinking (HED) has decreased globally from 22.6% in 2000 to 18.2% in 2016, but it is expected to increase to 23% in 2030 [15]. HED remains high at over 60%, especially in parts of Eastern Europe and in sub-Saharan African countries [9]. HED among young people (15ŌĆō19 years of age) is particularly prevalent (Ōēź20%) in Europe and high-income countries, including the USA, Canada, Australia, and New Zealand and in some South American countries, such as Chile and Argentina, where per capita alcohol consumption is relatively high [6].
Alcohol-attributable deaths and DALYs declined from 2000 to 2016 by 17.9% and 14.5%, respectively [8]. This decrease is less than the relative decreases in the rates of all deaths of 23.7% and all DALYs of 25.2% during the same period [8]. In 2016, 3.0 million death worldwide (2.3 million among men and 0.7 million among women) and 132 million DALYs (106 million among men and 26 million among women) were attributable to alcohol, representing 5.3% of all deaths and 5.0% of all DALYs [8,9]. This made alcohol the seventh major risk factor for death and disability globally in 2016 [8]. At the regional level, alcohol-attributable rates for death and DALYs are highest in the Eastern European and sub-Saharan African regions [8]. The proportions of alcohol-attributable deaths and DALYs are highest in the European region (10.1% of all deaths and 10.8% of all DALYs) and the Americas (5.5% of deaths and 6.7% of DALYs) [9].
The alcohol-attributable burden is particularly borne among young adults, for whom alcohol ranks as the leading cause of premature deaths [8,9]. Alcohol use accounted for 7.2% of all premature mortality globally in 2016 [9]. Young persons are more disproportionately affected by alcohol than older persons, and the proportion of alcohol-attributable deaths is highest among the population aged 20ŌĆō39 years, representing 13.5% of all deaths in this age group [9]. More than 50% of all alcohol-attributable deaths occur in people younger than 60 years [8].
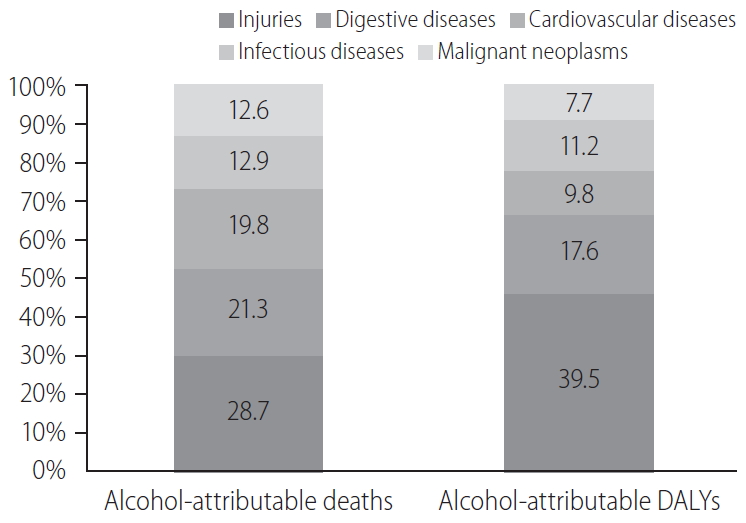
Acute alcohol intoxication negatively affects a number of cognitive functions, including memory, planning and complex motor control [16,17] and this loss can lead to unexpected behavior and injury. In 2016, injury was the leading cause of all deaths attributable to alcohol worldwide, accounting for 28.7% (Fig. 1) [9]. Similarly, injury is the leading contributor to the burden of disease caused by alcohol and accounts for approximately 40% of all alcohol-attributable DALYs [9]. Globally, 0.9 million injury deaths are attributable to alcohol [9], including road injuries (approximately 370,000 deaths), self-harm (approximately 150,000 deaths), interpersonal violence (approximately 90,000 deaths), and falls (approximately 80,000 deaths). Of the road traffic injuries, half of the deaths are among people other than drivers [9]. Geographically, the most alcohol-attributable injury deaths are in the African region and in the European region [9].
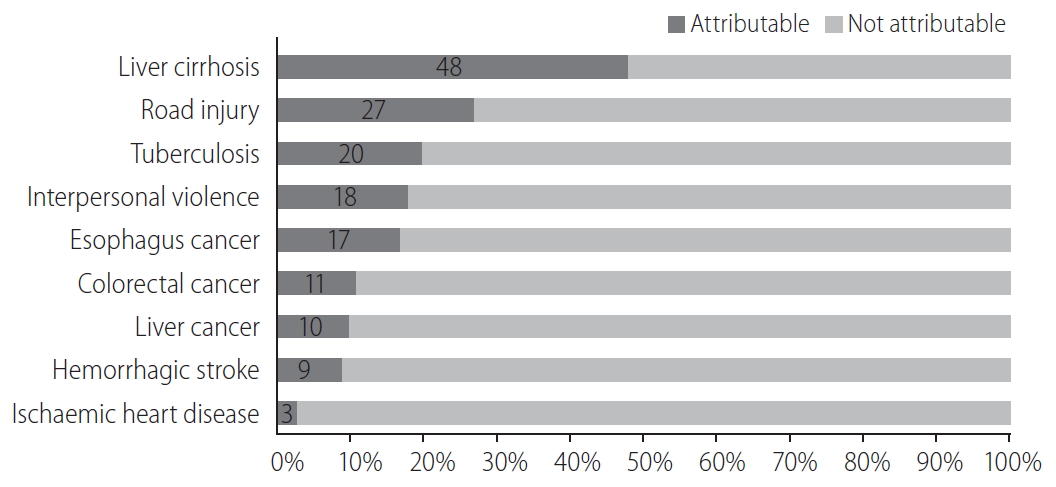
Digestive diseases, particularly liver cirrhosis, are the second leading contributors to alcohol-attributable deaths, representing 21.3% of these deaths (Fig. 1) [9]. Most deaths from alcohol-attributable digestive diseases concern liver cirrhosis (approximately 610,000 deaths) and pancreatitis (30,000 deaths) [9]. Alcohol is the cause of 60% of all liver cirrhosis in developed countries (Europe and North America), and the mortality and morbidity due to alcohol-related liver cirrhosis presents an increasing trend [18]. In the Asia-Pacific region, one-quarter of deaths due to cirrhosis and other chronic liver diseases are attributable to alcohol use [19]. Digestive disease deaths due to alcohol are highest in Africa (16.9 deaths per 100,000 people) and the Western Pacific regions (10.8 deaths per 100,000 people) [9]. Moreover, the contribution of alcohol to digestive diseases is highest in the European region, accounting for approximately 30% of all digestive disease deaths [9]. The contribution of alcohol to deaths from cirrhosis is approximately 50%; this figure would disappear in the absence of alcohol use at the global level (Fig. 2) [9].
It is worth mentioning that if the liver is already damaged by hepatitis B or C virus infection, even relatively low amounts of alcohol consumption can lead to death [9]. Consequently, tabulation by etiological coding of liver cirrhosis according to the artificially defined amount of alcohol is apt to underestimate the effects of alcohol [9].
CVDs are the number 1 cause of death globally, causing an estimated 17.8 million or 31% of all deaths and 413.2 million or 16% of all DALYs worldwide in 2017 [20]. Alcohol causes an estimated net CVD burden of approximately 600,000 deaths (3.3% of all CVD deaths) and 13 million CVD DALYs (3.2% of all CVD DALYs) [9]. CVDs account for 19.8% and 9.8% of alcohol deaths and DALYs, respectively (Fig. 1) [9]. At the regional level, alcohol-attributable CVD deaths and DALYs are highest in the European region and the African region [9]. In a similar fashion, the contribution of alcohol as a cause of CVD is highest in the European region, where alcohol accounts for 10.5% of all CVD deaths and 11.0% of CVD DALYs [9].
When described precisely by cause of CVD, alcohol has a net detrimental effect on hemorrhagic strokes, hypertensive heart disease, cardiomyopathy, and ischemic heart disease [9]. The leading contributors to the alcohol-attributable CVD burden are hemorrhagic strokes and ischemic heart disease, accounting for 47.5% and 42.5% of all alcohol-attributable CVD deaths, respectively [9]. Although alcohol has a net protective effect on ischemic stroke (preventing 33,000 ischemic stroke deaths), these preventive effects may have been overestimated by a potential confounding by the ADH1B genotype [21]. Genetic polymorphism of ADH1B (A-allele variant) has a protective effect against the development of alcohol dependence [22]. A-allele carriers again drink less and have lower risk of cardiovascular disease [21]. Furthermore, alcohol, even at light or moderate intake, increases the risk of atrial fibrillation and flutter [23].
Alcohol is a major contributor to the burden of communicable, maternal, perinatal and nutritional conditions, with 0.4 million alcohol-attributable deaths (3.3% of the total) and 13.9 million alcohol-attributable DALYs (1.9% of the total) [8]. The leading cause of attributable deaths from these conditions is tuberculosis, responsible for approximately 250,000 or 19.6% of all tuberculosis deaths [9]. Geographically, alcohol-attributable infectious disease deaths are highest in Africa and South-East Asian regions, accounting for 33% and 14%, respectively, of all alcohol-attributable deaths [9]. Furthermore, alcohol has multiple effects on the risk of communicable diseases, including vulnerability to infection, the likelihood of unprotected sex, and poor adherence to a medication regimen [24].
Globally, the burden of cancer is estimated to have risen to 18.1 million new cases and 9.6 million deaths in 2018 [25]. One in five men and one in six women develop cancer during their lifetime, and one in eight men and one in 11 women die from the cancer [25]. The International Agency for Research on Cancer (IARC), a specialized WHO agency, has determined a causal link between alcohol consumption and cancers, including oral cavity, pharynx, larynx, esophagus, liver, colorectal and female breast cancer [26].
It is estimated that approximately 0.4 million or 4.2% of all cancer deaths worldwide were attributed to alcohol use in 2016 [9]. The three leading causes of the alcohol-attributable cancer burden are colorectal, liver, and esophageal cancers [9]. Regionally, the burden of alcohol-attributable cancers was highest in the European (8.4 deaths per 100,000 people) and American regions (5.1 deaths per 100,000 people) [9].
Although the global burden caused by the harmful use of alcohol is enormous, alcohol consumption is not homogenous and varies widely across the world [9]. More than half (57%) of the worldŌĆÖs adults (Ōēź15 years) have not consumed alcohol in the previous 12 months [9].
Alcohol consumption is deeply affected by many factors at the individual and population levels [15,18]. Identifying those factors is important. Of those factors, three stand out as the most important: religion (especially Islam), economic development, and the implementation of alcohol policies [15,18].
The wealth of a country is associated with higher alcohol consumption and a higher prevalence of current drinkers across all WHO regions [9]. Historically, in many European countries, industrialization of alcoholic beverages was an early aspect of the industrial revolution, and the rates of heavy alcohol drinking and alcohol-related harm rose steeply as the relative alcohol price dropped and alcoholic beverages became more widely available in many European empires and their colonies [9]. As societies become more affluent, there is a strong tendency in general for the amount of alcohol consumption to increase up to a certain level, after which no further increases in alcohol consumption occur [15]. Usually, the lowest percentages of abstainers (<40%) are found in high-income countries [9]. In low-income countries, most people simply do not have enough money to buy alcoholic beverages, and consequently, the percentage of abstainers is high, with alcohol consumption mainly restricted to the more affluent individuals in the country [15]. In most low- and middle-income countries, industrialization offers more people disposable income for alcoholic beverages, and the commercialization of alcohol increases [15]. A dramatic example can be found in Eastern European countries [9]. With the commercialization of the alcohol markets after the dissolution of the Soviet Union, the level of alcohol consumption and alcoholrelated harm increased markedly [9].
Although economic factors play a large part, Islam plays a more dominant role [15]. For example, in countries such as Saudi Arabia or Brunei, alcohol consumption is apparently low despite the high gross domestic product per capita at purchasing power parity (GDP-PPP) due to the presence of Islamic alcohol policies [15]. The highest percentages (more than 80%) of past 12-month abstainers are found in Muslim-majority countries [9].
In addition to religious and economic factors, alcohol policies can have an impact [9,15]. One of the prime examples is Russia, where the WHOŌĆÖs ŌĆśBest BuysŌĆÖ interventions and minimum alcohol pricing were implemented, resulting in dramatic changes in both alcohol consumption and the alcohol-attributable burden of disease (see below) [15]. In contrast, the USA, a high-income country, is another example where life expectancies are stagnant or not increased primarily due to alcohol-related causes of death [15]. Between 1990 and 2016, overall death rates in the USA declined, however, there are wide differences by age and at the state level [27]. The change in the probability of death from birth to age 20 years declined in all states. For ages 20 to 55 years, the probability of death actually increased in 21 states (Kentucky, Oklahoma, New Mexico, West Virginia, and Wyoming showed an increase of greater than 10%). For ages 55 to 90 years, all states experienced a considerable reduction in probabilities of death [27]. Moreover, recent data (between 2010 and 2015) showed life expectancy at birth for the USA has not increased or stagnant although the most important causes of death (such as CVDs or cancer) have declined [28,29]. A detailed inspection of this data showed that most of the causes of death are markedly impacted by alcohol and illicit drug use [28,29]. Furthermore, a high proportion of the increased premature mortality happened in lower socio-economic strata [28,29] led by the ŌĆśdeaths of despairŌĆÖ [30-32].
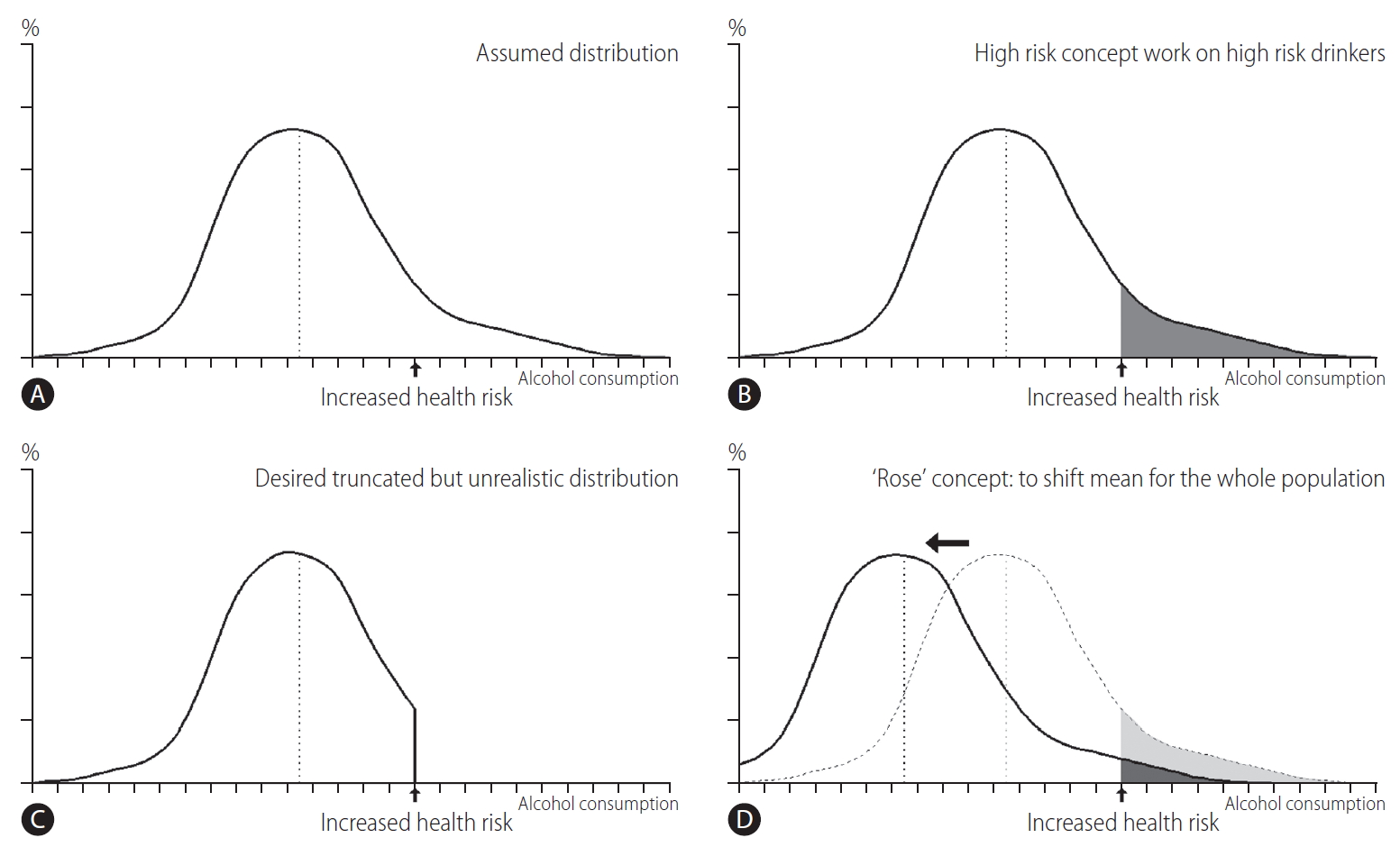
Health problems, such as alcohol-related problems, usually show a continuous distribution in terms of the intensity of risk factors or derangements. Figure 3 illustrates the strategic difference between the high-risk versus population-based approaches. People at one end of the distribution are not particularly deviant but a continuing part of one end (Fig. 3) [33].
An assumed distribution of alcohol consumption in a population is shown in Figure 3A. As the level of alcohol consumption increases, the health risks also rise. At a certain point, the increased health risk is considered as unacceptable (arrow). The shaded area of Figure 3B is the high-risk group. The high-risk approach focuses on this group. If the high-risk approach is fully successful, the end result would be as shown in Figure 3C, a highly unlike result. The population-based approach, in contrast to high-risk approach, emerges because a distribution such as that in Figure 3C is not feasible in the real world. Population-based approach is to change the entire distribution to reduce the risk within a population. The main difference between the high-risk versus population-based approaches is in the fact that high-risk approach focuses on high-risk ŌĆśindividualsŌĆÖ instead of the total sum of risk factors in a ŌĆśpopulationŌĆÖ [33]. On RoseŌĆÖs argument [34] in Figure 3D, the reduction of alcohol-related problems in a population should be directed to shift the entire distribution of alcohol consumption leftward, and with that shift, the average and total consumption in the population consequently declines. Such a shift in the distribution requires social actions that address the levels of total alcohol consumption with the aim to reduce the harm in the population as a whole, not merely confined in high-risk individuals [33].
Alcohol policies are laws, rules, and regulations that aim to prevent and reduce alcohol-related harm [9]. The ŌĆśGlobal action plan for the prevention and control of noncommunicable diseases (NCDs) 2013ŌĆō2020ŌĆÖ proposed in the WHOŌĆÖs global strategy which endorsed by the World Health Assembly in 2010 [35] included recommended interventions to reduce alcohol-related harm at the national level with focus on the most cost-effective measures [9,36,37]. These WHO recommended interventions, so-called ŌĆśbest buysŌĆÖ, include increased taxation on alcoholic beverages, enforced restrictions on the physical availability of alcohol and comprehensive restrictions or bans on advertising alcoholic beverages (Table 2) [9,18].
It has been suggested that the most effective measure is a combination of various alcohol policies, especially in countries with high alcohol-related burdens [18]. The ultimate goal is to design a package of population-based alcohol policies considering the specific characteristics of a country to have the highest impact on both alcohol consumption and the alcohol-related burden [18,38].
Alcohol policy development and implementation have advanced [9] but are still far from satisfactory in effectively protecting populations from alcohol-related harm. The challenges in implementing optimal alcohol policies to reduce the alcohol-related harm and burden include low levels of political commitment to coordinate multi-sector actions to reduce harmful use, the strong influence of commercial interests that go against implementing effective alcohol policies, and the drinking culture and traditions in a society [9].
The responsibility for the implementation of effective alcohol policies is often dispersed between diverse systems, governmental departments, intergovernmental agencies and professions ŌĆō for which alcohol problems are not a major concern [9]. This ŌĆśdivision of laborŌĆÖ makes alcohol policies difficult to run effectively and coherently at the national level [9]. Therefore, reducing the harmful use of alcohol at the population level and the alcohol-related burden in a country requires the ŌĆśwhole of governmentŌĆÖ and ŌĆśwhole of societyŌĆÖ approaches with appropriate public health-oriented engagement [9]. Partnerships and the appropriate engagement of all relevant stakeholders, such as nongovernmental organizations and professional and civil societies, are required to implement cost-effective measures that can ensure returns to the ŌĆśwhole countryŌĆÖ and the ŌĆśwhole nationŌĆÖ by reducing the harmful use of alcohol and the alcohol-related burden [9].
From the 2nd WHO report in 2004, it has given examples of leadership of member states. The latest 5th WHO report in 2018 lists eight countries as examples, including the Russian Federation, Thailand and Brazil [9]. In Thailand, only a minority of adults drink alcohol, but the country experiences substantial alcohol-attributable harms [9]. The likelihood of domestic violence increased fourfold when one person drinks, and two in five crimes committed by young people involve alcohol [9]. Thailand has managed this problem through the ŌĆśtriangle that moves the mountainŌĆÖ. The three legs are strong scientific communities, energetic grassroots movements and evidence-based policies [9]. In Brazil, traffic crashes are the leading cause of death among young male and 78% of drivers in fatal crashes test positive for alcohol [9]. ŌĆśVida UrgenteŌĆÖ (urgent life), a community-based drinking driving campaign in the state of Rio Grande do Sul, had an impressive success during Carnival, an event that is often marked by high rates of traffic crash fatalities [9]. There was not a single road traffic fatality on the major roads near Carnival in Porto Alegre in the years that the ŌĆśBuzoomŌĆÖ(driver) event, the campaign provided buses to transport, was in place [9].
Russia has long been regarded as one of the heavy alcohol-consuming countries in the world [9]. Heavy alcohol consumption has been established as one of the main causes of the Russian mortality crisis of the 1990s and 2000s [9,39]. Alcohol consumption was the primary culprit of the mortality increase that started in the 1980s and led to 75% of deaths among men aged 15ŌĆō55 years [6]. Life expectancy in men plummeted by more than 6 years reaching its absolute low of 57 years between 1990 and 1994 [39,40]. However, these trends have been impressively reversed in recent years [41].
After 2003, per capita alcohol consumption dropped substantially from 18.7 L in 2005 to 11.7 L in 2016 as a result of the staggered implementation of alcohol policies [9]. Life expectancy started to increase in 2003 and reached its all-time high of 68 years for men and 78 years for women in 2018 [41]. Between 2003 and 2018, all-cause mortality dropped by 39% in men and by 36% in women [42].
Over time, the Russian governmentŌĆÖs alcohol policies started with very basic attempts to reinstate control over alcohol production and sales and to eliminate unrecorded alcohol production [41]. In the early 1990s, the government slowly regained control over alcohol production and sales, with the enactment of Federal Law No. 171 in 1995 [41]. After 2000, the Russian alcohol market was substantially reorganized to reduce the proportion of unrecorded alcohol [40,41]. Alcohol policies at that time mainly targeted control over alcohol production and sales, not individual consumers [41].
Alcohol policies evolved into comprehensive approaches, taking a long-term view aimed at reducing the harmful use of alcohol, the alcohol-related burden and the total level of alcohol consumption in the population [41]. In 2009, evidence-based measures, including increased alcohol excise taxes, an increased minimum unit price, and a substantial reduction in the availability of retail alcohol, were implemented [41,43].
Despite ongoing efforts for alcohol control, alcohol remains a leading global risk factor for premature mortality, with 3 million alcohol-attributable deaths. Its toll will remain substantial if there are no concerted and sustained policy initiatives. Recommendations for abstaining from alcohol should be prioritized because the level of consumption that minimizes an individualŌĆÖs risk is zero.
To reduce the harmful use of alcohol in a country, the ŌĆśwhole of governmentŌĆÖ and ŌĆśwhole of societyŌĆÖ approaches are required with the implementation of evidence-based alcohol control policies, the pursuit of public health priorities, and the adoption of appropriate policies over a long period of time.
ACKNOWLEDGMENTS
This research was supported by Basic Science Research Program (2020R1A6A1A03043026) through the National Research Foundation of Korea (NRF) funded by the Ministry of Education.
FOOTNOTES
Figure┬Ā1.
Distribution of all alcohol-attributable burden by broad disease category, 2016. Data available from global status report on alcohol and health 2018 [9].
Figure┬Ā2.
Alcohol-attributable fractions (AAF) for selected causes of death, 2016; AAF: the proportion of deaths which would disappear if there had not been any alcohol. Data available from global status report on alcohol and health 2018 [9].
Figure┬Ā3.
(A-D) The actual, high risk, truncated, and shifted distributions of alcohol-related problems. X axis denotes amount of alcohol consumed, Y axis denotes prevalence in a given population. Modified from Bhopal [33].
Table┬Ā1.
Definitions of related terms [9]
Table┬Ā2.
WHOŌĆÖs recommended interventions to reduce the harmful use of alcohol [36]
| ŌĆśBest buysŌĆÖ: effective interventions with cost effectiveness analysis (CEA) ŌēżI$100 per DALY averted in LMICs | Increase excise taxes on alcoholic beverages* |
| Enact and enforce bans or comprehensive restrictions on exposure to alcohol advertising (across multiple types of media)ŌĆĀ | |
| Enact and enforce restrictions on the physical availability of retailed alcohol (via reduced hours of sale)ŌĆĪ | |
| Effective interventions with CEA >I$100 per DALY averted in LMICs | Enact and enforce drink-driving laws and blood alcohol concentration limits via sobriety checkpoints┬¦ |
| Provide brief psychosocial intervention for persons with hazardous and harmful alcohol useŌłź | |
| Other recommended interventions from WHO guidance (CEA not available) | Carry out regular reviews of prices in relation to level of inflation and income |
| Establish minimum prices for alcohol where applicable | |
| Enact and enforce an appropriate minimum age for purchase or consumption of alcoholic beverages and reduce density of retail outlets | |
| Restrict or ban promotions of alcoholic beverages in connection with sponsorships and activities targeting young people | |
| Provide prevention, treatment and care for alcohol use disorders and comorbid conditions in health and social services | |
| Provide consumer information about, and label, alcoholic beverages to indicate, the harm related to alcohol |
CEA, cost-effectiveness analysis; I$, international dollars; DALY, disability-adjusted life-year; LMIC, lower middle income countries; WHO, World Health Organization.
* Requires an effective system for tax administration and should be combined with efforts to prevent tax avoidance and tax evasion.
Abbreviations
CVDs
cardiovascular diseases
DALYs
disability-adjusted life-years
GBD
Global Burden of Disease
GDP-PPP
gross domestic product per capita at purchasing power parity
HED
heavy episodic drinking
IARC
International Agency for Research on Cancer
NCD
noncommunicable disease
SDI
socio-demographic index
WHO
World Health Organization
REFERENCES
1. Schwartz JM, Reinus JF. Prevalence and natural history of alcoholic liver disease. Clin Liver Dis 2012;16:659-666.


3. GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659-1724.


4. Das P, Samarasekera U. The story of GBD 2010: a ŌĆ£super-humanŌĆØ effort. Lancet 2012;380:2067-2070.


5. GBD 2013 Risk Factors Collaborators, Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287-2323.



6. GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018;392:1015-1035.


7. GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry 2018;5:987-1012.



8. Shield K, Manthey J, Rylett M, Probst C, Wettlaufer A, Parry CDH, et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Health 2020;5:e51-e61.


9. World Health Organization (WHO). Global status report on alcohol and health 2018. Geneva: WHO; 2018.
10. Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671.



11. Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 2006;166:2437-2445.


12. Naimi TS, Stockwell T, Zhao J, Xuan Z, Dangardt F, Saitz R, et al. Selection biases in observational studies affect associations between ŌĆśmoderateŌĆÖ alcohol consumption and mortality. Addiction 2017;112:207-214.


13. Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018;391:1513-1523.



14. Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do ŌĆ£moderateŌĆØ drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J Stud Alcohol Drugs 2016;77:185-198.



15. Manthey J, Shield KD, Rylett M, Hasan OSM, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet 2019;393:2493-2502.


16. Peterson JB, Rothfleisch J, Zelazo PD, Pihl RO. Acute alcohol intoxication and cognitive functioning. J Stud Alcohol 1990;51:114-122.


17. Cherpitel CJ, Ye Y, Bond J, Borges G, Monteiro M. Relative risk of injury from acute alcohol consumption: modeling the dose-response relationship in emergency department data from 18 countries. Addiction 2015;110:279-288.



18. Ventura-Cots M, Ballester-Ferr├® MP, Ravi S, Bataller R. Public health policies and alcohol-related liver disease. JHEP Rep 2019;1:403-413.



19. Sarin SK, Kumar M, Eslam M, George J, Al Mahtab M, Akbar SMF, et al. Liver diseases in the Asia-Pacific region: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol Hepatol 2020;5:167-228.



20. Jagannathan R, Patel SA, Ali MK, Narayan KMV. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr Diab Rep 2019;19:44.



21. Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014;349:g4164.



22. Kang G, Bae KY, Kim SW, Kim J, Shin HY, Kim JM, et al. Effect of the allelic variant of alcohol dehydrogenase ADH1B*2 on ethanol metabolism. Alcohol Clin Exp Res 2014;38:1502-1509.


23. Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol 2014;64:281-289.


24. Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr 2009;52:180-202.



25. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424.


26. Secretan B, Straif K, Baan R, Grosse Y, El Ghissassi F, Bouvard V, et al. A review of human carcinogens--part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. Lancet Oncol 2009;10:1033-1034.


27. The US Burden of Disease Collaborators, Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, et al. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US States. JAMA 2018;319:1444-1472.



28. Imtiaz S, Probst C, Rehm J. Substance use and population life expectancy in the USA: interactions with health inequalities and implications for policy. Drug Alcohol Rev 2018;37 Suppl 1:S263-S267.


29. Rehm J, Probst C. Decreases of life expectancy despite decreases in non-communicable disease mortality: the role of substance use and socioeconomic status. Eur Addict Res 2018;24:53-59.


30. Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015;112:15078-15083.



31. Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act 2017;2017:397-476.



32. WHO Regional Office for Europe. Status report on alcohol consumption, harm and policy responses in 30 European countries 2019. WHO web site, <https://www.euro.who.int/en/health-topics/disease-prevention/alcohol-use/publications/2019/status-report-on-alcohol-consumption,-harm-and-policy-responses-in-30-european-countries-2019>. Accessed 10 Aug 2020.
33. Bhopal R. Sick Populations and sick individuals. In: Raj S, ed. Concepts of Epidemiology: an integrated introduction to the ideas, theories, principles and methods of epidemiology. New York: Oxford University Press; 2002. p. 26-31.
34. Rose G. The strategy of preventive medicine. New York: Oxford University Press; 1994.
35. World Health Organization (WHO). Global strategy to reduce the harmful use of alcohol. WHO web site, <http://www.who.int/substance_abuse/publications/global_strategy_reduce_harmful_use_alcohol/en/>. Accessed 17 Jun 2020.
36. World Health Organization (WHO). Tackling NCDs: ŌĆ£best buysŌĆØ and other recommended interventions for the prevention and control of noncommunicable diseases. WHO web site, <https://apps.who.int/iris/bitstream/handle/10665/259232/WHO-NMH-NVI-17.9-eng. pdf?sequence=1&isAllowed=y>. Accessed 17 Jun 2020.
37. World Health Organization (WHO). Global action plan for the prevention and control of NCDs 2013ŌĆō2020. WHO web site, <https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1>. Accessed 17 Jun 2020.
38. Chisholm D, Moro D, Bertram M, Pretorius C, Gmel G, Shield K, et al. Are the ŌĆ£best buysŌĆØ for alcohol control still valid? An update on the comparative cost-effectiveness of alcohol control strategies at the global level. J Stud Alcohol Drugs 2018;79:514-522.


39. Leon DA, Saburova L, Tomkins S, Andreev E, Kiryanov N, McKee M, et al. Hazardous alcohol drinking and premature mortality in Russia: a population based case-control study. Lancet 2007;369:2001-2009.


40. Zaridze D, Lewington S, Boroda A, Sc├®lo G, Karpov R, Lazarev A, et al. Alcohol and mortality in Russia: prospective observational study of 151,000 adults. Lancet 2014;383:1465-1473.



41. World Health Organization (WHO). Alcohol policy impact case study: the effects of alcohol control measures on mortality and life expectancy in the Russian Federation. Copenhagen: WHO Regional Office for Europe; 2019.
42. The Lancet Gastroenterology Hepatology. Alcohol and health: time for an overdue conversation. Lancet Gastroenterol Hepatol 2020;5:229.


- TOOLS
-
METRICS

- ORCID iDs
-
Dong Joon Kim

https://orcid.org/0000-0002-5792-1500 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



