The role of transjugular intrahepatic portosystemic shunt in patients with portal hypertension: Advantages and pitfalls
Article information
Abstract
Transjugular intrahepatic portosystemic shunt (TIPS) is an effective interventional procedure to relieve portal hypertension, which is a main mechanism for the development of complications of liver cirrhosis (LC), such as variceal hemorrhage, ascites, and hepatorenal syndrome. However, the high incidence of adverse events after TIPS implementation limits its application in clinical practice. Esophageal variceal hemorrhage is one of the major indications for TIPS. Recently, preemptively performed TIPS has been recommended, as several studies have shown that TIPS significantly reduced mortality as well as rebleeding or failure to control bleeding in patients who are at high risk of treatment failure for bleeding control with endoscopic variceal ligation and vasoactive drugs. Meanwhile, recurrent ascites is another indication for TIPS with a proven survival benefit. TIPS may also be considered as an effective treatment for other LC complications, usually as an alternative therapy. Although there are concerns about the development of hepatic encephalopathy and hepatic dysfunction after TIPS implementation, careful patient selection using prognostic scores can lead to excellent outcomes. Assessments of cardiac and renal function prior to TIPS may also be considered to improve patient prognosis.
INTRODUCTION
Complications of decompensated liver cirrhosis (LC) can seriously impair the quality of life and also increase the morbidity and mortality rates of patients. Although liver transplantation (LT) is the best way to reverse the clinical course of patients with decompensated LC, only a limited number of the patients may undergo LT due to a persistent shortage of viable organs. Portal hypertension is the main pathologic mechanism driving the occurrence of LC complications. First-line treatments for such complications, which include sodium restrictions and the use of diuretics for ascites or vasoactive drugs and endoscopic therapy for variceal bleeding, do not aim to alleviate portal hypertension itself but instead manage symptoms; therefore, patients may still suffer from recurrent episodes of these LC complications.
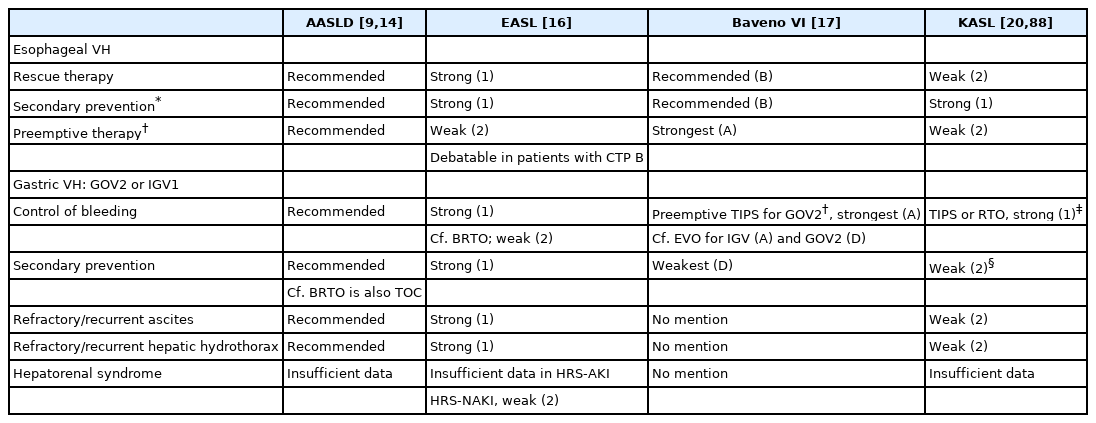
Transjugular intrahepatic portosystemic shunt (TIPS) robustly reduces portal hypertension by establishing a shunt within the liver. The procedure is performed by creating an intrahepatic portosystemic shunt connecting the right or main portal vein to the hepatic vein, aiming to reduce the porto-systemic pressure gradient (PPG) while maintaining adequate liver perfusion (Fig. 1). The most common indications of TIPS are uncontrolled bleeding from the esophageal varix and refractory or recurrent ascites. TIPS can also be considered in patients with gastric variceal hemorrhage, hepatic hydrothorax, Budd-Chiari syndrome (BCS), or noncirrhotic portal hypertension. In addition to the therapeutic purpose of LC complications, TIPS decompresses increased resistance of portal venous blood flow, leading to stabilization of the activated renin–angiotension and sympathetic systems. Moreover, enhanced translocation of the gut microbiome and systemic inflammation in patients with portal hypertension decrease after TIPS implementation [1]. Despite these advantages, however, there are non-negligible adverse events that may arise following TIPS, including hepatic encephalopathy (HE) and hepatic or cardiac dysfunction, which limit the use of TIPS in LC patients.
Overview of TIPS. The main complications of TIPS and their countermeasures are presented. TIPS, transjugular intrahepatic portosystemic shunt; PPG, porto-systemic pressure gradient.
Until 2000, TIPS was performed using bare metal stents, thus carrying a significant drawback of shunt dysfunction due to stent stenosis occurring in more than 50% of patients within 1 year, mainly by the proliferation of the intima [2,3]. Among the remarkable advances in the TIPS procedure, the development of polytetrafluoroethylene (PTFE)-covered stents was the most outstanding achievement to date. PTFE can suppress the proliferation of intima, thus maintaining stent patency [4]. The rate of primary patency of TIPS was significantly improved to 86% and 80% at 1 and 2 years, respectively, compared to 47% and 19%, respectively, in the setting of TIPS with bare stent placement [4].
TIPS is usually indicated as a rescue therapy in LC patients who have developed complications with no response to first-line treatment, and sometimes as a bridging therapy for LT. However, practical clinicians often hesitate to decide whether to perform TIPS in LC patients due to the adverse effects of TIPS. In this review, we aimed to demonstrate the most suitable timing and candidates for performing TIPS in patients with LC complications. We also summarized the main complications of TIPS, as well as their countermeasures.
PROCEDURE
Since variceal bleeding or ascites usually occurs with a PPG of above 12 mmHg, TIPS is performed to reach a goal of reducing the PPG to below 12 mmHg or by 50% or more of the baseline value [2,5]. However, complications following TIPS, such as HE or hepatic dysfunction, usually occur when the PPG is adjusted to less than 5 to 10 mmHg; therefore, the targeted level is suggested to be higher than 10 mmHg with a narrow therapeutic window [3]. Technically, it is not easy to accurately relocate the target PPG to between 10 to 12 mmHg during the procedure. TIPS is generally performed by full or partial expansion of 8- or 10-mm stents [5,6]. Nowadays, a smaller 8-mm stent has been more commonly used, as it demonstrated similar efficacy to the 10-mm stent but a lower incidence of HE or hepatic dysfunction [7]. In addition, a recent prospective, multicenter study showed that TIPS with 8-mm stents led to significantly higher transplant-free survival rates compared to using 10-mm stents [6].
PATENCY
Although the incidence of shunt dysfunction significantly decreased after using PTFE-covered stents, guidelines suggest performing a doppler ultrasound to examine shunt patency at intervals of 6 or 12 months after the procedure [8,9]. Stenosis of the shunt is mainly caused by intimal proliferation; however, it can rarely result from thrombosis in patients with inadequate coverage of the stent, bile leakage into the stent, or a hypercoagulable condition, such as BCS [5,10,11]. A previous study showed that prophylactic use of antiplatelet or anticoagulation medications for preventing stent thrombosis after TIPS reduced the rate of shunt stenosis, and some centers have adopted the prophylactic use of anticoagulation as a strategy [12,13]. However, evidence is insufficient to encourage the prophylactic use of antiplatelet or anticoagulant drugs in patients with TIPS [14].
INDICATIONS
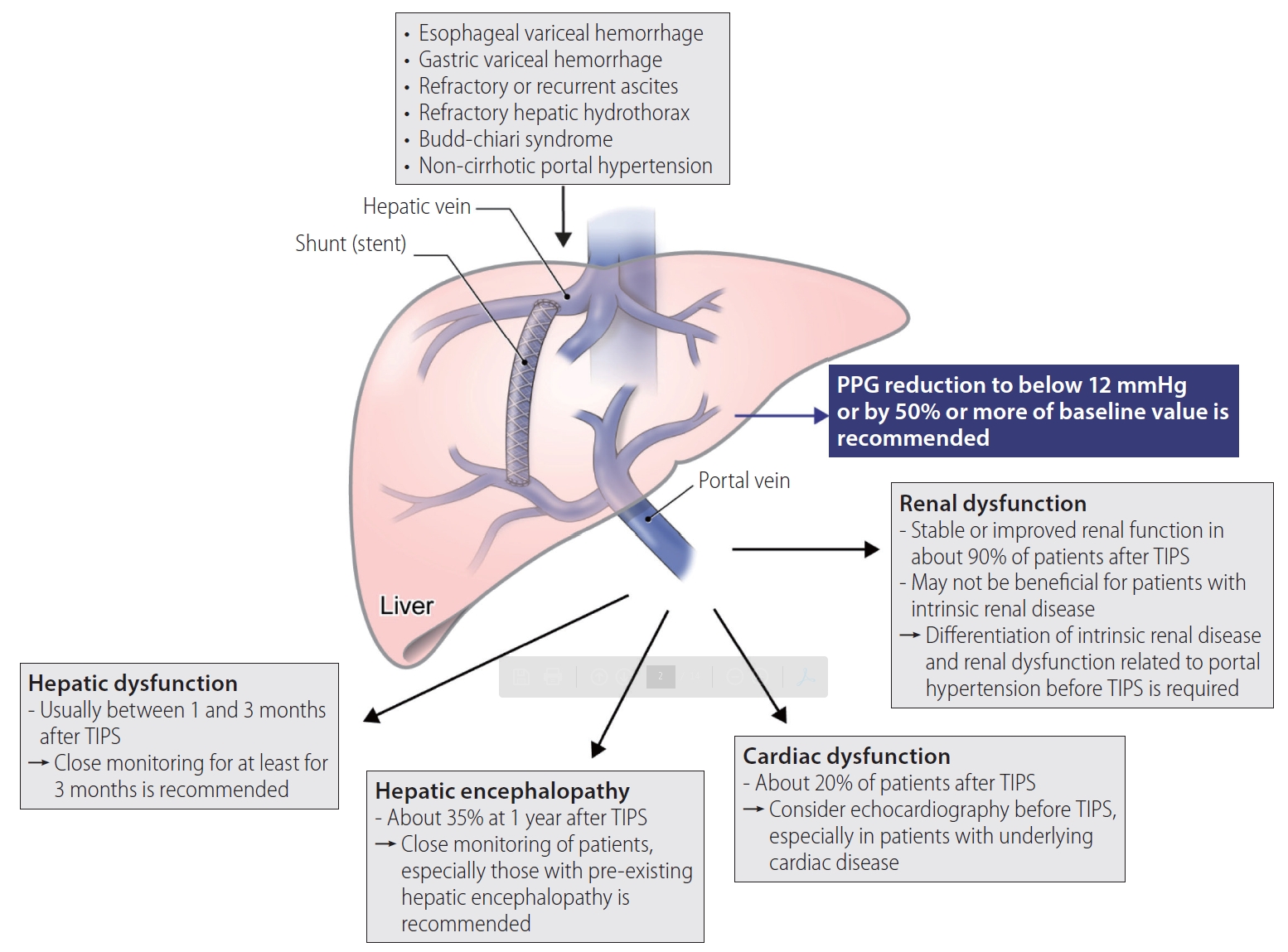
The optimal timing for TIPS in LC complications is schematically shown in Figure 2, and clinical indications for TIPS recommended in each guideline are summarized in Table 1.
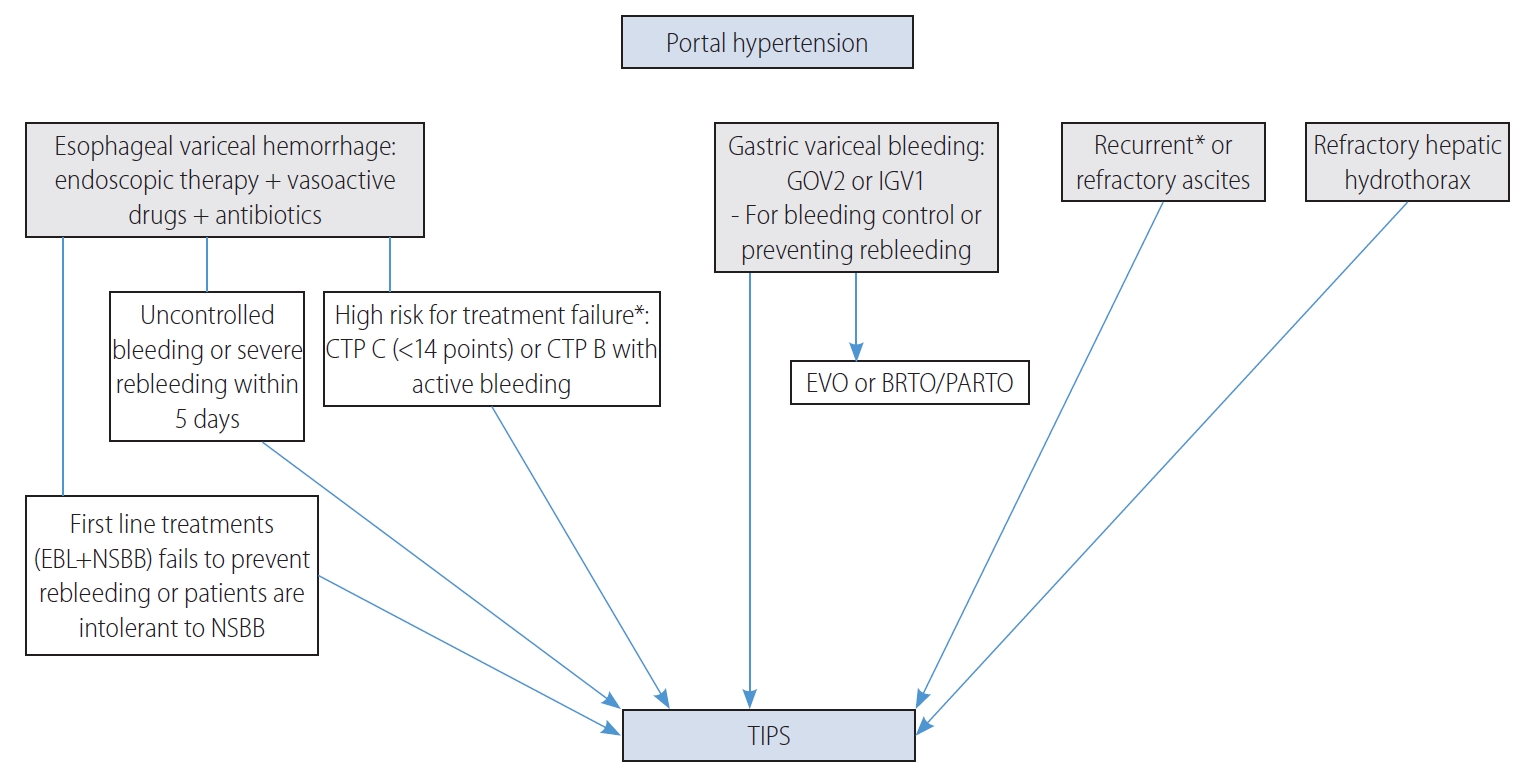
The main indications for TIPS are presented. CTP, Child-Turcotte-Pugh; EBL, endoscopic band ligation; NSBB, nonselective beta-blockers; GOV, gastroesophageal varices; IGV, isolated gastric varices; EVO, endoscopic variceal obliteration; BRTO, balloon occluded retrograde transvenous obliteration; PARTO, plug-assisted retrograde transvenous obliteration; TIPS, transjugular intrahepatic portosystemic shunt. *The survival benefit of TIPS was demonstrated in randomized controlled trials.
Esophageal VH
Acute VH should be managed with endoscopic treatment within 12 hours of admission, if the patient is hemodynamically stable, together with the administration of antibiotics and vasoactive drugs, such as somatostatin, octreotide, or terlipressin. The implementation of TIPS can be considered for uncontrolled VH or for secondary prevention of esophageal VH. TIPS as a preemptive therapy for patients at high risk of treatment failure with standard treatment (e.g., endoscopic therapy, vasoactive drugs, and antibiotics) is nowadays highly recommended. TIPS is not indicated for primary prevention of esophageal VH.
Preemptive TIPS
Considering the high risk of liver decompensation or death after treatment failure for acute VH, the use of preemptive TIPS (pTIPS) was suggested in terms of early application of effective treatment [15]. The pTIPS refers to performing the procedure within 72 hours of initial endoscopy in patients with acute VH at high risk of treatment failure and poor outcome despite standard treatments consisting of vasoactive drugs, antibiotics, and endoscopic therapy [15]. Three randomized controlled trials (RCTs) and several observational studies have proven the efficacy of pTIPS in reducing rebleeding of the esophageal varix and mortality. Based on these results, recent guidelines recommend performing pTIPS in patients who are at high risk, such as those with Child-Turcotte-Pugh (CTP) C (<14 points) or CTP B with active bleeding after initial pharmacological and endoscopic therapy [9,16,17].
In the first RCT for pTIPS, LC patients who were admitted for acute VH and a hepatic venous pressure gradient (HVPG) greater than 20 mmHg were defined as a high-risk group for treatment failure and randomly allocated to undergo pTIPS (within 24 hours after admission) or not. Preemptive TIPS significantly reduced the treatment failure, in-hospital, and 1-year mortality rates compared to medical treatment. However, interpretation of the results should consider the limitations inherent with using medical treatment different from the current standard therapy and when using bare stents, recently exchanged for PTFE-covered stents [18]. In another European multicenter RCT, using PTFE-covered stents, LC patients with acute VH were enrolled to evaluate the efficacy of pTIPS. Patients with CTP C (10–13 points) or those with CTP B and active bleeding at initial endoscopy after admission were defined as a high-risk group for treatment failure and randomly assigned to pTIPS or standard treatment (vasoactive drugs + endoscopic treatment) groups. The incidence of remaining free from treatment failure within 1 year was significantly higher in the pTIPS group than that in the standard treatment group (97% and 50%, respectively; P<0.001). The 1-year survival rate was also significantly high at 86% in the pTIPS group versus 61% in the standard treatment group (P<0.001). There was no significant difference in the incidence of post-TIPS HE between the two groups [15]. Unlike other RCTs, the most recent RCT enrolled LC patients with CTP B regardless of active bleeding at endoscopy or CTP C (<14 points) and set survival benefit as the primary outcome. In this study, pTIPS independently reduced mortality (adjusted hazard ratio [aHR], 0.44; 95% confidence interval [CI], 0.22–0.88; P=0.02] and treatment failure (aHR, 0.25; 95% CI, 0.12–0.54; P<0.0001) compared to standard treatment. The incidence of post-TIPS HE was similar (35% vs. 36%; P=1.00) between the two groups [19]. Therefore, all three RCTs consistently demonstrated that pTIPS not only reduced variceal rebleeding but also improved survival. There was no difference in the incidence of post-TIPS HE between the pTIPS and standard treatment groups. However, this is not because pTIPS is relatively safe from this complication; the reason is that, if pTIPS is not performed, the increased risk of esophageal VH and combined other complications may precipitate the development of HE. Based on these results, the Baveno VI consensus states that pTIPS should be considered in patients at high risk for treatment failure (CTP C [<14 points] or CTP B with active bleeding) after initial pharmacological and endoscopic therapy [17].
However, some observational studies have demonstrated no survival benefit from pTIPS; therefore, guidelines of the American Association for the Study of Liver Diseases (AASLD), European Association for the Study of the Liver (EASL), and Korean Association for the Study of the Liver all recommend pTIPS, with the caveat that further studies are needed [9,16,20-22]. There are also concerns regarding the definition of high-risk patients, such as whether CTP B patients with active bleeding should be classified into this group [23]. A recent meta-analysis confirmed the efficacy of pTIPS in terms of reducing mortality to 56% compared to standard treatments in patients with CTP C (<14 points) or CTP B with active bleeding, but not in subgroup of patients with a CTP score of 7 points due to their good prognosis [24].
Regarding the timing of pTIPS, the procedure was usually performed within 3 days of index bleeding in previous studies, but the same effects have also been demonstrated when pTIPS was performed within 5 days of index bleeding [25]. However, there was no survival benefit when TIPS was performed for secondary prevention within 6–15 days after index bleeding, although clinical indications were somewhat different [26,27]. Considering that the effect of pTIPS is predominantly to reduce early rebleeding [19], it is recommended to perform pTIPS at the earliest time after VH.
Rescue therapy or secondary prevention
Although RCTs are still lacking, current guidelines recommend TIPS as a rescue therapy for patients who experience persistent bleeding or severe rebleeding despite standard treatment within the first 5 days after admission for acute VH, which occurs in 10 to 15% of the patients [9,16,17].
Rebleeding of esophageal VH is accompanied by a significant mortality rate of up to 33%; thus, nonselective beta-blockers (NSBB) in combination with endoscopic band ligation (EBL) are recommended for secondary prevention in patients who experienced a first episode of VH [9,17]. Performing TIPS in order to prevent rebleeding compared to standard treatments (EBL + NSBB) has been evaluated in previous studies. TIPS with an uncovered stent significantly reduced the rebleeding rate compared to medical treatments, but the incidence of HE was significantly higher in patients who underwent TIPS [28]. A recent RCT with PTFE-covered stents investigated the role of TIPS compared to elective EBLs with NSBB in patients who were hemodynamically stabilized after initial treatment for a first or second occurrence of esophageal or gastric VH. TIPS significantly reduced the rate of rebleeding but increased the incidence of post-TIPS HE by 35% within 1 year compared to standard treatment. However, during a long-term follow-up period, the difference in the incidence of post-TIPS HE disappeared (38% vs. 23%; P=0.121). Also, the survival rate was not significantly different between the two groups [26]. Another large randomized study, which enrolled patients with a mean CTP score of 7 points and model for end-stage liver disease (MELD) score of 10 points and who experienced VH more than 5 days ago, compared the effect of TIPS with an 8-mm covered stent to HVPG-guided medical treatment (NSBB therapy). Here, the TIPS group had significantly reduced rebleeding rate compared to the medical treatment group (P=0.002), but the survival rate was not different. In this study, patients in the TIPS group had a slightly greater 2-year incidence of HE (18% vs. 8%; P=0.05), but the quality of life was not different [27]. Collectively, TIPS for secondary prevention definitely reduced the risk of rebleeding with a slight increase in HE incidence compared to medical treatment. Nevertheless, there was no difference in the survival rate. Recent guidelines have recommended NSBB be combined with EBL as a firstline therapy for secondary prevention of esophageal VH; however, if the first-line treatment (NSBB + EBL) fails or patients are intolerant to NSBB, TIPS should be considered [9,16,17,20].
Gastric VH
Acute bleeding from gastroesophageal varices type 1 (GOV1) can be controlled by endoscopic therapy, either by EBL or cyanoacrylate glue injection. In the case of bleeding from cardiofundal varices (GOV2 or isolated gastric varices type 1), the guidelines of AASLD and EASL recommend TIPS as a treatment of choice for the control of acute bleeding and the prevention of rebleeding from cardiofundal varices [9,16]. A RCT evaluating the role of TIPS in the prevention of rebleeding from gastric varices showed that TIPS was more effective than endoscopic cyanoacrylate injection, with similar survival and complication rates [29]. Balloon occluded retrograde transvenous obliteration (BRTO) or technically modified methods, such as plug-assisted retrograde transvenous obliteration or coil-assisted retrograde transvenous obliteration, can also be used instead of TIPS with similar efficacy. A recent RCT demonstrated the high efficacy of BRTO in reducing the rebleeding rate of gastric varices compared to endoscopic cyanoacrylate injection, with similar complication rates or aggravation of esophageal varices [30]. In addition, a meta-analysis showed that the post-procedure rebleeding rate was significantly lower in patients treated with BRTO compared to those treated with TIPS (odds ratio [OR], 0.27; 95% CI, 0.09–0.81; P=0.02) [31]. BRTO has the advantage of being able to preserve blood flow to the liver; however, portal hypertension can be aggravated, leading to worsening of ascites in 9.2% of patients or the recurrence of esophageal varices in 33.3% of patients who received BRTO [32]. In summary, TIPS is recommended for the control of acute bleeding and the prevention of rebleeding from gastric varices. BRTO can also be used instead of TIPS with a similar or higher efficacy rate in reducing the rebleeding rate [31], although more data are needed for determining the best candidate.
Refractory or recurrent ascites
Although large-volume paracentesis (LVP) is the first-line treatment for uncontrolled ascites despite high-dose diuretics and salt restriction, TIPS can be considered an effective alternative in patients who require LVP at frequent intervals [16]. In previous RCTs comparing TIPS and LVP in patients with refractory or recurrent ascites, TIPS significantly improved ascites compared to LVP, but the incidence of post-TIPS HE increased and survival outcomes were inconsistent [33-37]. However, the role of TIPS for refractory or recurrent ascites needs to be reassessed, since these studies used bare stents for TIPS. In a meta-analysis of patients with variceal bleeding, mainly including patients who used PTFE-covered stents, TIPS improved the occurrence of ascites by 74% without increasing the risk of post-TIPS HE [24]. To date, the survival benefit of TIPS in patients with refractory ascites has not been identified. Instead, a recent RCT evaluating the effects of TIPS with PTFE-covered stents compared to LVP with albumin therapy in patients with recurrent ascites demonstrated that TIPS independently improved the 1-year transplant-free survival rate (HR, 2.1; 95% CI, 1.1–4.0). There was no difference in the incidence of post-TIPS HE, which was 35% in both groups [38].
In patients with refractory or recurrent ascites, TIPS can also improve sarcopenia due to increased absorption of intestinal nutrients by relieving portal hypertension and decreased protein loss by paracentesis [39]. Although the timing of TIPS for recurrent or refractory ascites has not yet been determined, a study which demonstrated 1-year survival benefit from TIPS in patients with recurrent ascites enrolled patients who required LVP at least two times within 3 months, while excluding patients who required more than six times during the same period [38]; this strategy of patient selection for early TIPS boasted a degree of cost-effectiveness compared to LVP with albumin therapy [40]. Another study showed that a high frequency of LVP (OR, 1.2; 95% CI, 1.3–2.4) and elevated creatinine level (OR, 2.6; 95% CI, 1.2–6.6) were significantly associated with TIPS failure for controlling ascites [41]. Therefore, performing early TIPS before patients suffer from highly frequent LVP that impairs their quality of life might improve clinical prognosis and also enhance the effectiveness of TIPS.
Hepatic hydrothorax
About 5–10% of patients with LC suffer from hepatic hydrothorax, and 20–25% of them have refractory hepatic hydrothorax that does not respond to salt restriction or high-dose diuretics [42,43]. In these patients, repeated thoracentesis is required, but procedure-related complications frequently accompany this procedure, such as pneumothorax, bleeding, or infection. For the same reasons, chronic drainage of pleural effusion is not recommended. Although pleurodesis can be considered for refractory hepatic hydrothorax, it is rarely used in practice due to its complication rate of about 82% [44]. Although there has been limited evidence to support the efficacy of TIPS for refractory hepatic hydrothorax, especially when using PTFE-covered stents, complete or partial resolution of hepatic hydrothorax after TIPS was reported to range from 59% to 81% in case series [45-50]. In addition, a recent study that compared TIPS using PTFE-covered stents with other modalities (i.e., medical treatment, thoracentesis, and catheter drainage) in patients with hepatic hydrothorax showed no difference in mortality among the various treatment groups [51]. Therefore, TIPS is the preferred alternative treatment in patients who require repeated thoracentesis due to refractory hepatic hydrothorax. Further investigation is required to disclose the efficacy of TIPS using PTFE-covered stents in refractory hepatic hydrothorax.
Others
Hepatocellular carcinoma (HCC)
Although HCC is a relative contraindication to TIPS, it can be considered if anatomically accessible and clinically necessary [14,52]. A few studies have evaluated the effect of TIPS implementation on HCC patients. A previous study including 209 HCC patients who underwent TIPS before or after an HCC diagnosis reported that TIPS successfully decreased HVPG, leading to an improvement in portal hypertension symptoms, such as esophageal VH or refractory ascites [53]. In a small number of HCC patients with refractory ascites, TIPS implementation improved CTP scores in 78% of the study population, mainly by controlling ascites. Improvements in CTP scores increase the chance of receiving treatments for HCC, which leads to a survival benefit [54]. TACE, a major treatment modality for HCC, can cause hepatic ischemia through arterial embolization; therefore, liver perfusion can be further reduced after TACE in patients with TIPS, which diverts the portal venous inflow. A previous study showed that TACE with drug-eluting beads in HCC patients with TIPS significantly reduced the incidence of hepatotoxicity after TACE and improved the overall survival rate compared to conventional TACE [55]. However, there are still concerns regarding the occurrence of hepatic dysfunction or HE after TIPS, which deprives patients of the opportunity to receive treatments for HCC or tumor dissemination during the procedure. TIPS implementation in HCC patients should be decided while considering each patient’s individual situation.
Hepatorenal syndrome (HRS)
There has been no RCT that compared the use of TIPS to medical treatment (i.e., vasoconstrictors and albumin) in patients with HRS. To date, the role of TIPS in HRS remains controversial. TIPS can alleviate circulatory and neurohormonal derangement by reducing portal hypertension; therefore, theoretically, TIPS can be beneficial for patients with HRS. In patients with type 1 or 2 HRS who received TIPS, limited data showed that renal function was improved [56,57]. In addition, a recent study using a large population cohort demonstrated a survival benefit from TIPS in patients with LC and HRS relative to non-TIPS (adjusted OR, 0.43; 95% CI, 0.30–0.62; P<0.001) [58]. However, TIPS is rarely indicated in patients with HRS, a complication of end-stage liver disease, as these individuals frequently have severe hepatic dysfunction and TIPS can further deteriorate their renal function due to reduced systemic arterial pressure.
BCS and noncirrhotic portal hypertension
Regarding BCS, current guidelines recommend TIPS to be performed in symptomatic patients if anticoagulation therapy or hepatic vein interventions, such as stenting or angioplasty, have failed [8,59]. Portal hypertensive complications resolved in more than 70% of BCS patients who received TIPS, and the 5-year survival rate was greater than 70% [8]. TIPS can also be used in patients with noncirrhotic portal hypertension with indications similar to those of LC patients [8]. The 1-year rebleeding rate range was 5–11% and the 5-year survival rate was nearly 90% in patients with noncirrhotic portal hypertension who underwent TIPS for recurrent VH [60,61].
CONTRAINDICATIONS
General contraindications for TIPS, as stated in guidelines, are as follows: congestive heart failure, pulmonary hypertension (absolutely contraindicated when pulmonary pressure is above a mean value of 45 mmHg), progressive renal failure, HE of grade 2 or higher according to the West Haven criteria, uncontrolled systemic infection, severe thrombocytopenia, or coagulopathy (Table 2) [14,16]. TIPS implementation increases blood flow to the central circulation, which can cause serious problems in patients with underlying cardiopulmonary diseases and worsen renal function in patients with underlying renal disease. TIPS implementation should be decided cautiously in patients aged over 65 years, as these patients are more prone to developing HE [8]. Existing guidelines suggest TIPS to be performed at experienced centers [16]. Medical centers that have performed TIPS at least 20 times per year had a significantly lower inpatient mortality rate compared to those that did not (adjusted OR, 2.5; P=0.04) [62].
TIPS is relatively contraindicated in patients with severe hepatic dysfunction, such as a serum bilirubin level of greater than 4 mg/dL or MELD score of greater than 15 to 18 points [14]. However, it is unclear whether the effects of TIPS outweigh the risk of complications that can develop after TIPS in these patients. A few studies showed that pTIPS contributed to improving the prognosis in patients with severe hepatic dysfunction. A previous study of three French hospitals, which enrolled patients with a mean MELD score of 29 points and CTP score of 13, showed that 6-week and 1-year survival rates were significantly improved in patients treated with pTIPS compared to those treated with standard treatment: the 6-week survival rates were 76.5% and 35.3% in the pTIPS and control groups (P=0.023), respectively, and the 1-year survival rates were 76.5% and 23.5% (P=0.005), respectively [63]. In patients with acute on chronic liver failure (ACLF) due to acute VH, pTIPS was associated with a reduced 1-year mortality rate compared to standard treatments (22.7% vs. 56.5%; P=0.002). Preemptive TIPS also achieved survival benefit in patients with ACLF and a bilirubin level of greater than 5 mg/dL [64]. In a meta-analysis, the survival rate of the pTIPS group was significantly higher than that in the standard treatment group among patients with bilirubin levels of above 5 mg/dL or even those with levels of above 10 mg/dL [24]. However, these studies only included a small number of patients, and additional studies are needed to recommend TIPS in patients with severe hepatic dysfunction. Careful patient selection for TIPS is important to balance the benefits of TIPS over the occurrence of complications after TIPS.
PROGNOSIS
Hepatic dysfunction
Hepatic dysfunction can develop after TIPS, since the portal blood flow bypasses intrahepatic circulation and travels directly to the inferior vena cava through a portosystemic shunt. The liver can also be affected by hypotension during the procedure. A previous study reported a significant incidence of hepatic failure (death, LT, or MELD score >18 points) within 3 months after TIPS as 9.3% among patients with baseline MELD scores of 9.6 points (range, 6–12). In these patients, MELD scores of 11–12 points, low hemoglobin concentrations, and low platelet counts were independently associated with the development of early hepatic failure. However, the relatively high rate of hepatic failure might be due to the fact that this study enrolled patients who underwent TIPS between 1999 and 2012 at a single center [65].
The deterioration of hepatic function is usually a transient event after TIPS, and is manifested by the elevation of bilirubin level [5]. In a recent RCT for evaluating the role of pTIPS in acute VH, serum bilirubin level, international normalized ratio, and MELD score were slightly increased at 1 and 3 months and improved at 6 months after TIPS. In addition, the effect of pTIPS was evident in reducing liver-related mortality compared to standard treatments [19]. Therefore, although concerns about hepatic dysfunction after TIPS still exist, hepatic failure is not a common event if TIPS is performed according to indications. Close monitoring of hepatic function is warranted, at least for a short period of time, after TIPS.
HE
HE is the most concerning complication that may develop after TIPS; therefore, guidelines do not recommend TIPS implementation in patients on recurrent or persistent overt HE (grade ≥2 according to the West Haven criteria) [16]. For patients with covert HE, there are differences in suggestions according to the guidelines. A recent guideline does not recommend TIPS in patients with covert HE, while the AASLD guideline suggests avoiding TIPS only when the HE is uncontrollable with standard therapy [8,14]. Post-TIPS HE was more common in patients with minimal HE, and there was no case of recurrent overt HE after TIPS in patients with no history of overt HE and no current minimal HE diagnosed with the critical flicker frequency [66]. However, several prospective studies which evaluated the effect of TIPS in LC patients excluded only patients with overt HE and 1-year incidence of HE after TIPS was about 35%, similar to that in patients who received standard therapy [7,38,66]. Strict criteria in patients with HE might limit candidates for TIPS since the procedure is restricted to patients with decompensated LC. Therefore, although TIPS is not recommended for patients with overt HE, those with covert HE can receive TIPS, with close monitoring for the occurrence of post-TIPS HE.
A significant proportion of LC patients have sarcopenia and are at an increased risk of developing HE, as the role of muscle in the disposal of ammonia is enhanced in LC patients [67]. Previously, sarcopenia was identified as a predictor for the development of HE in patients who underwent TIPS [68]. However, in a recent study, although the risk of post-TIPS HE was significantly reduced in patients with a higher skeletal muscle index (SMI) used for evaluating sarcopenia in LC patients, sarcopenia itself was not associated with post-TIPS HE. Furthermore, SMI improved after TIPS in LC patients [39]. An average SMI increased as 17% after a mean 10 months of TIPS [69]. Therefore, although close monitoring of the development of HE after TIPS is important in patients with sarcopenia, performing TIPS in patients with sarcopenia should not necessarily be avoided.
A previous RCT showed that prophylactic use of rifaximin or lactitol was not effective in reducing the development of post-TIPS HE [70]. Therefore, guidelines do not recommend routine prophylactic treatment for HE in patients who underwent TIPS [71]. However, the most recent RCT evaluating the role of rifaximin as a prophylactic treatment for post-TIPS HE demonstrated that the incidence of overt HE after TIPS was significantly lower in patients who received rifaximin compared to that in patients who received placebo during a follow-up period of 6 months (34% vs. 53%, respectively; P=0.012) [72]. A possible reason for the relatively high incidence of HE in this study could be that PPG after TIPS was too low, at 6 mmHg. Further study of prophylactic treatments for the development of post-TIPS HE is required to gather long-term data.
Cardiac dysfunction
LC patients are in a vulnerable state for developing cardiac dysfunction. The prevalence of cirrhotic cardiomyopathy, which refers to cardiac dysfunction in LC patients without known cardiac disease, ranges from 26% to 81%, according to existing studies [73,74]. Although TIPS implementation can have the positive effects of increasing the cardiac preload and output as the portal flow directly enters the inferior vena cava through the shunt, sudden hemodynamic changes caused by TIPS can overwhelm the hearts of LC patients and lead to severe cardiac decompensation.
Several previous studies have focused on predicting cardiac complications after TIPS. In a retrospective study, 50.4% of LC patients had abnormal findings on echocardiography performed before TIPS, but the results of the exam did not predict mortality. However, this study was limited in that the predictive role of echocardiography for the development of cardiac complications after TIPS was not evaluated [75]. A recent prospective study showed that cardiac decompensation occurred in 20% of LC patients treated with TIPS. Brain natriuretic peptide (BNP), NT-proBNP level, and echocardiography before TIPS implementation discriminated patients at high risk for such. Cardiac decompensation did not occur in patients with a BNP level of less than 40 pg/mL and NT-proBNP level of less than 120 pg/mL before TIPS insertion, but developed in 51.4% of patients with echocardiographic findings, suggesting diastolic dysfunction [76]. Collectively, a significant proportion of LC patients have combined cardiac dysfunction, and many of them can develop cardiac decompensation after TIPS. To date, there is no consensus regarding the use of echocardiography to predict cardiac complications after TIPS. The EASL guideline recommends performing routine echocardiography before elective TIPS, while the AASLD guideline does not take a clear stance on the role of the examination [14,16]. A recent guideline suggests performing echocardiography if abnormal findings are found in preprocedure evaluations, such a 12-lead electocardiogram or cardiac markers, including NT-proBNP [8]. Further research is needed to evaluate the role and cost-effectiveness of echocardiography before performing TIPS in LC patients.
Renal function
TIPS restores hemodynamic and neurohormonal derangement, increasing natriuresis within 4 weeks, which may lead to an improvement in renal function [77,78]. TIPS implementation for LC patients with refractory ascites and an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 m2 at baseline significantly improved the eGFR (the expected change in eGFR after 90 days, TIPS vs. serial LVP as reference, 21; 95% CI, 13–29; P<0.001), while there was no change in the eGFR level in patients with an eGFR of 60 mL/min/1.73 m2 or greater [79]. Other studies have also demonstrated an improvement in renal function after TIPS [80,81]. However, TIPS might not be beneficial in patients who already have intrinsic renal disease [82]. A high creatinine level was significantly associated with post-TIPS HE [83]. In addition, the contrast agents used when performing TIPS can also worsen renal function in these individuals. A recent study that enrolled 673 patients who underwent TIPS showed that 10% of the patients experienced deterioration in renal function at 30 days after TIPS. Patients with nonalcoholic fatty liver disease and diabetes who were susceptible to having intrinsic renal disease were at high risk of post-TIPS renal impairment [81]. A recent guideline does not recommend performing TIPS in patients with intrinsic renal disease of stage 4 or 5 [8]. Collectively, although renal dysfunction caused by portal hypertension usually improves after TIPS, performing TIPS should be carefully decided in patients with intrinsic renal disease.
PROGNOSTIC SCORES AND PATIENT SELECTION
Several prognostic scores for predicting survival after TIPS have been developed, such as the CTP, MELD, or MELD-Na scores [84,85]. A bilirubin-platelet model was developed for LC patients with refractory ascites and introduced in the EASL guideline [16]. The 1-year survival rate was significantly lower at 31.2% in patients with a platelet count of less than 75×109/L or a bilirubin level of greater than 3 mg/dL compared to 73.1% in patients with a platelet count of greater than 75×109/L and a bilirubin of less than 3 mg/dL [86]. Recently, a new score of the Freiburg index of post-TIP survival (FIPS) using age and bilirubin, albumin, and creatinine levels was introduced to improve the prognostic predictability for patients undergoing elective TIPS implementation. FIPS indicated that the median overall survival was significantly shorter as 3.1–5.0 months in patients in the high-risk group compared to the low-risk group [87]. However, the result should be validated in future studies.
CONCLUSIONS
Although clinicians may have concerns about performing TIPS due to the non-negligible complications, recent studies have shown high efficacy of TIPS compared to other treatments and presented an acceptable complication rate, albeit not different from when TIP was not performed. Moreover, the survival benefit of pTIPS was proved in patients who are at high risk for treatment failure of esophageal VH. Early TIPS before patients suffer from repeated LVP for refractory or recurrent ascites showed improved quality of life and cost-effectiveness compared to LVP, as well as a significantly higher 1-year transplant-free survival. In the context of organ shortage for LT, the role of TIPS needs to be actively considered in clinical practice. However, to achieve the benefits of TIPS, proper timing and patient selection are crucial.
Notes
Authors’ contribution
Guarantor of the article: Sung Won Lee
Specific author contributions: Study concept and design: Sung Won Lee and Hae Lim Lee; Wrote the paper: Sung Won Lee and Hae Lim Lee. All authors have approved this final version of the manuscript.
Conflicts of Interest: The authors have no conflicts to disclose.
Abbreviations
AASLD
American Association for the Study of Liver Diseases
ACLF
acute on chronic liver failure
aHR
adjusted hazard ratio
BCS
Budd-Chiari syndrome
BNP
brain natriuretic peptide
BRTO
balloon occluded retrograde transvenous obliteration
CI
confidence interval
CTP
Child-Turcotte-Pugh
EASL
European Association for the Study of the Liver
EBL
endoscopic band ligation
eGFR
estimated glomerular filtration rate
FIPS
Freiburg index of post-TIP survival
GOV1
gastroesophageal varices type 1
HCC
hepatocellular carcinoma
HE
hepatic encephalopathy
HRS
hepatorenal syndrome
HVPG
hepatic venous pressure gradient
LC
liver cirrhosis
LT
liver transplantation
LVP
large-volume paracentesis
MELD
model for end-stage liver disease
NSBB
nonselective beta-blockers
OR
odds ratio
PPG
porto-systemic pressure gradient
PTFE
polytetrafluoroethylene
pTIPS
preemptive transjugular intrahepatic portosystemic shunt
RCT
randomized controlled trial
SMI
skeletal muscle index
TACE
transarterial chemoembolization
TIPS
transjugular intrahepatic portosystemic shunt