Fibrolamellar hepatocellular carcinoma-related hyperammonemic encephalopathy: Up to now and next steps
Article information
Dear Editor,
We recently had the opportunity ro read the brilliant paper by Thakral and Simonetto “Hyperammonemic encephalopathy: An unusual presentation of fibrolamellar hepatocellular carcinoma” in the Clinical and Molecular Hepatology [1]. We would appreciate to share some insights about this interesting theme.
Fibrolamellar hepatocellular carcinoma (FLHCC) is indeed a rare primary hepatic tumor that arises in non-cirrhotic livers, more common in males (male to female ratio 1.7), with age-specific incidence with two peaks between ages of 10–30 and 60–69 (although being a tumor usually believed to affect mostly very young individuals) and is associated with better 5-year survival than conventional hepatocellular carcinoma (HCC) [2]. Although FLHCC was usually referred as a subtype of HCC, recent researches have demonstrated that FLHCC is actually an independent entity, with distinctive molecular tumor profile, histological features and clinical presentation [3,4].
One of the most feared complications associated with FLHCC is the development of acute onset hyperammonemic encephalopathy (HAE), which was first reported by Sethi et al. [5] in 2009, this condition is associated with high mortality [6].
High mortality was related to the ignorance of the physiopathology of HAE in patients with FLHCC. Some authors have proposed some explanations, such as portosystemic shunt [5,7]. In 2017, we published a new proposal of the physiopathology of this complication of FLHCC, and initiated with the very unique mutation (a heterozygous deletion of chromosome 19) that is responsible for the development of the tumor. This mutation is responsbile for overexperssion of a chimeric DNAJB1-PRKACA kinase and Aurora Kinase A that culminate with c-Myc and ornithine decarboxylase dysfunction and result in depletion of amino acids crucial to urea cycle function [8]. This urea cycle dysfuntion is then responsible for the acummulation of ammonia in the bloodsteram and occurs HAE.
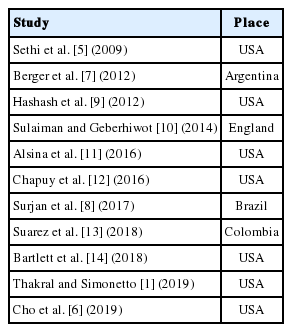
The importance of this finding was, once understanding that an urea cycle disorder due to metabolites consumption was responsible for the hyperammonemia, to guide the developement of new medical treatment options based on a combination of ammonia scavenger drugs (sodium benzoate and phenylbutyrate) with amino acids supplementation (citrulline, ornithine and arginine), thus reducing the mortality of FLHCC-related HAE and allowing complete clinical recovery from HAE [1,6,8]. Table 1 summarizes all published reports on FLHCC-related HAE.
So, we think that question stated by Hashash et al. [9] in 2012 “What is the cause of acute hepatic encephalopathy in a young patient?” regarding an 18-year-old patient with a large FLHCC has been answered, including its precise pathophysiology. Nevetheless, a few more steps must still be taken. First, the molecular basis of the proposed pathophysiology is needed to be proven. Second, there were more studies are warranted to demosntrate the efficacy and safety of these new treatment options. Third, this treatment regimen for hyperammonia may be useful for other causes of liver-related HAE such as portosystemic shunt, acute liver failure and cirrhosis.
Notes
Authors’ contributions
Rodrigo Cañada trofo Surjan designed and wrote the paper, designed the proposal of the pathophysiology described and performed final approval of the article. Elizabeth Santana dos Santos was involved in direct patient care and data collection. Sergio do Prado Silveira performed data collection and paper drafting. Fabio Ferrari Makdissi and Marcel Autran Cesar Machado performed critical review of the article.
Conflicts of Interest
The authors have no conflicts to disclose.
Abbreviations
FLHCC
fibrolamellar hepatocellular carcinoma
HCC
hepatocellular carcinoma
HAE
hyperammonemic encephalopathy