Macro-aspartate aminotransferase in a healthy woman
Article information
Dear Editor,
An increase in serum aspartate aminotransferase (AST) may be related to different conditions, including viral hepatitis, alcoholic liver disease, cirrhosis, cholestatic syndromes, acute myocardial infarction, or skeletal muscle trauma [1]. Chronic and isolated elevation of AST in patients with no related clinical signs or symptoms is suggestive for the presence of macro-aspartate aminotransferase (macroAST) [2]. MacroAST is a macroenzyme that circulates in the bloodstream as a high molecular weight complex, either by self-polymerisation or by association with serum proteins such as immunoglobulins (Ig) [1]. The formation of this complex, particularly with Ig, may lead to increased activity and/or reduced inactivation, clearance or excretion [1,3]. Below is a case report of a healthy woman with elevated AST levels due to the presence of macroAST.
A 45-year-old female was admitted to the gastroenterology department of Careggi Hospital in Florence, because of an isolated increase in AST levels. Family history was positive for arterial hypertension and stroke. The patient had a body mass index of 22.0, and her clinical history showed that she had an ovarian cyst 5 years ago and had taken oral contraceptives from the age of 18 to 35 years. No major findings were present at clinical examination.
Abdominal ultrasound did not reveal any alterations, except for a newly formed ovarian cyst on the left side. The electrocardiogram did not show any abnormalities. Blood tests at admission showed: AST 149 U/L (reference interval, 15–37); alanine aminotransferase 19 U/L (reference interval, 12–65); creatine phosphokinase 95 U/L (reference interval, 21–215); haptoglobin 1.01 g/L (reference interval, 0.3–2); troponin I <0.015 μg/L (reference interval, 0–0.09); myoglobin 42 ng/mL (reference interval, 14–106); and creatine kinase-MB 0.7 ng/mL (reference interval, 0.5–3.6). The levels of lactate dehydrogenase and aldolase were also normal. Diagnostic testing for thyroid disease, muscle disorders, haemolysis and coeliac disease was negative. Serology of viral hepatitis B, C, A, Epstein-Barr virus, cytomegalovirus, and human immunodeficiency virus was also negative [4]. Values of the subsequent laboratory investigations were constant and varied only slightly over time. All other haematological and biochemical parameters were normal. Presence of macroAST was hypothesised by the gastroenterologist and the clinical laboratory was asked to perform additional tests to confirm this diagnosis.
For the detection of macroAST, the polyethylene glycol (PEG) precipitation method was used by the clinical laboratory as for the evaluation of macroprolactin [5]. Here, 200 μL of serum was added to an equal volume of PEG 6000 (Merck, Milano, Italy) 250 g/L in distilled water, vortex-mixed for 1 minute and centrifuged at 1,500 rpm for 30 minutes at 4°C, resulting in a clear supernatant with a precipitate at the bottom. The PEG solution was prepared fresh every 3 months and stored at 4°C [5]. Simultaneously, 100 μL of serum was mixed with 100 μL phosphate-buffered saline (PBS). AST activities were measured both on the supernatant and on the PBS dilution with a Siemens VISTA Clinical Chemistry System (Siemens Healthcare, Milano, Italy) and were adjusted with a correction factor of two for the dilution in the preparation. AST recovery was derived as a percentage of the AST activity measured in the supernatant relative to that measured in the PBS dilution [6]. To evaluate the effect of PEG precipitation, a serum sample of a patient previously diagnosed with hepatopathologic disease and negative for macroAST was selected and treated in the same way as the clinical case serum sample.
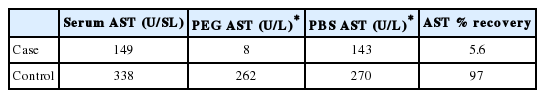
Table 1 shows AST activity after PEG precipitation in the patient from the case report and in the control patient. A recovery of AST activity ≤40% in cases of suspected macroAST indicates the presence of Ig-AST complexes, while this condition is very unlikely at values of AST recovery >50% [5]. The use of PEG at defined concentrations has the effect of subtracting the solvents, and the subsequent precipitation of proteins such as Ig and the complexes formed by them, thus measuring the remaining activity in the supernatant [7]. If macroAST is present, the activity of the enzyme after PEG precipitation is decreased compared to the control. Given this case report finding, the results are consistent with a diagnosis of macroAST and confirm the clinical suspicion. Figure 1 shows how the AST changed from 30, 10 days before diagnosis and during follow-up at 10, 30, and 120 days after diagnosis.
Recently, reports about this disease are increasing; Table 2 collects the macroAST literature previously reported, comparing similarities and differences of each case report. The presence of macroAST can be determined, as shown in Table 2, by laboratory techniques including gel filtration chromatography, ultrafiltration, immunofixation electrophoresis, Ig depletion using protein A and G, refrigerated sample storage for 3–6 days at 4°C and PEG precipitation. In gel filtration chromatography, the molecules are separated according to their size and shape. In this method, the stationary phase is made up of spheres of hydrated material, containing pores that can be crossed only by molecules with certain dimensions. In this way, molecules with dimensions that are too large will cross the column very quickly and be eluted into a smaller volume than the molecules that enter the pores instead. Ultrafiltration is based on the molecular weight of macroAST for separation. It is performed using centrifugal filter units with membranes, and AST activity is measured in the ultracentrifugate after centrifugation for 18 hours [1]. Ultracentrifugation and gel filtration chromatography, which constitute the standard reference method, require highly specialised chromatography, are complex, relatively expensive, and time-consuming and are not available in most clinical laboratories [8]. Electrophoresis for immunofixation with AST staining consists of the electrophoresis of serum proteins using the IgG, IgA and IgM antisera. It allows the nature of enzyme immune complexes to be clarified, but requires high specialisation skills [9]. For the Ig depletion method using protein A and G, instead, proteins A and G are recombinant bacterial proteins used to remove Ig and Ig-AST complexes after incubation with the patient’s serum. AST is determined in the supernatant after centrifugation of the sample. The protein A and G method is straightforward and provides unambiguous results, but this method is more expensive and probably only detects AST-IgG macrocomplexes [1]. Moreover, refrigerated sample storage for 3–6 days at 4°C determines the gradual precipitation of the enzyme-Ig complex. This method is simple and reliable, but it is performed over a long time and there is heterogeneity of the macroAST molecule due to the different types of Ig or other plasma components [8]. Finally, the PEG precipitation, described above, unlike the latter more complicated techniques, is a simple and low-cost method, which is commonly used for the detection of macroprolactin [5], possible in most routine laboratories and can be used for the screening of macroAST, giving a diagnosis in a short period of time. This method, however, has some limitations, like the possibility of interference with some assays, low specificity and the fact that an increase in serum globulins can lead to false positive results, as shown for macroprolactin [6].
Also, as shown in this case report, the fruitful cooperation and clear communication between clinicians and the clinical laboratory can lead to the early and correct diagnosis of macroAST, avoiding diagnostic confusion and unnecessary, time-consuming, expensive and even invasive investigations [3,6].
Notes
Authors’ contribution
Maria Lorubbio wrote the manuscript. Agostino Ognibene, Benedetta Salvadori, Alessandra Fanelli and Giacomo Laffi critically re-viewed the manuscript. All authors participated in final approval of the manuscript.
Conflicts of Interest: The authors have no conflicts of interests to disclose.
Acknowledgements
The authors would like to thank Professor Fabio Marra, MPhil for correction of the English.
Abbreviations
AST
aspartate aminotransferase
Ig
immunoglobulins
macroAST
macroaspartate aminotransferase
PBS
phosphate-buffered saline
PEG
polyethylene glycol