Sigmoid colon metastasis from hepatocellular carcinoma
Article information
Abstract
Hepatocellular carcinoma (HCC) is a major health problem worldwide, and it has a poor prognosis. Extrahepatic metastasis from HCC is not unusual, with direct invasion representing the main spreading mode. Sites that are frequently involved are the lung, bone, and lymph nodes. There are few reports of HCC invading the distant gastrointestinal tract, especially hematogenously. Herein we report a case of sigmoid colon metastasis from HCC. The patient was diagnosed with HCC and treated with transcatheter arterial chemoembolization (TACE). Eighteen months after TACE the patient presented with abdominal pain on the left lower quadrant, and a CT scan showed an enhanced mass on the sigmoid colon. Immunohistochemical staining revealed that a tumor cell was positive for polyclonal carcinoembryonic antigen and weakly positive for hepatocyte antigen, supporting the diagnosis of HCC metastasis. The patient underwent anterior resection for the metastatic HCC.
INTRODUCTION
Hepatocellular carcinoma (HCC) is a serious health problem and has a poor prognosis. HCC accounts for 5.6% of all human cancers with more than 1 million deaths annually and the incidence of HCC is increasing.1,2 Despite the implementation of surveillance programs for early HCC, most tumors are diagnosed at intermediate or advanced stages, and only 30% of patients benefit from curative therapies such as resection, liver transplantation, or percutaneous ablation.2,3
In the previous autopsy series, extrahepatic metastasis was present in 30~70% of cases and the major organs involved were lung, lymph nodes, bone, and the adrenal gland.4,5 Interestingly, involvement of the gastrointestinal (GI) tract from HCC seldom occurs, being found in only 4~6% of cases in the same series4,5 and 0.5~2% of cases in another series.6,7 Among the GI metastasis from HCC, colon metastasis, especially the left-sided colon, is very rare and mostly occurs through direct invasion.8,9
Here, we report on a HCC patient who was treated with transarterial chemoembolization (TACE) and had a solitary metastatic tumor from HCC on his sigmoid colon one and a half years after initial treatment.
CASE REPORT
A 47-year-old man was admitted with a hepatic mass incidentally detected by ultrasound. A computed tomography (CT) scan revealed a 1.7 cm-sized mass in the hepatic segment VI with enhancement on the arterial phase and early washout on the portal phase (Fig. 1A), and a tiny enhancing nodule on the arterial phase without early washout on the portal phase in segment IV (Fig. 1B). The patient was a hepatitis B virus (HBV) carrier. Upon physical examination, superficial lymphadenectasis, icteric sclera, liver palm, or spider telangiectasias were not observed. The laboratory findings showed a slight elevation of transaminase (aspartate aminotransferase: AST 78 IU/L, alanine aminotransferase: ALT 50 IU/L) and a mild decrease in platelet count (113,000/mm3). All other values including white blood cell, hemoglobin, protein, albumin, bilirubin, and prothrombin time were within normal limits. HBV surface antigen (HBsAg) and HBV e antigen (HBeAg) were positive but anti-hepatitis C virus antibody was negative. The alpha-fetoprotein (AFP) level was 365 ng/mL. A percutaneous needle biopsy was performed on the mass in segment VI and the pathologic diagnosis of HCC, Edmonson-Steiner grade 3, was made. The patient underwent transcatheter arterial angiography and chemoembolization (TACE) to treat the HCC and differentiate the tiny enhancing nodule from another HCC. On angiography, the enhancing nodule was identified as an AP shunt. After TACE, there had been no evidence of tumor recurrence on follow-up CT scans and AFP levels for one and a half years. In one and a half years, the patient presented with abdominal pain around the left lower quadrant. Physical examination was unremarkable and all laboratory findings including an AFP level were within normal limits except a mild elevation of liver enzymes: AST 46 IU/L and ALT 68 IU/L. On colonoscopy, a bulging contoured hard mass was noted in the sigmoid colon but the overlying mucosa was intact (Fig. 2A). The CT scan revealed a 4×3.5 cm sized, eccentric mass abutting the sigmoid colon without any lymph node enlargement (Fig. 2B). However, the scan did not show any evidence of recurrence in the liver and the portal tract. The patient underwent anterior resection and a well-defined subserosal mass, measuring 5.2×4×3.7 cm, was identified. The cut surface of the mass was grayish white, solid, and granular with hemorrhage and necrosis (Fig. 3A). The mass extended to the proper muscle layer, however, the overlying mucosa was intact. Histologic examination demonstrated sheets of large polygonal tumor cells arranged in a trabecular pattern. The tumor cells exhibited eosinophilic, granular cytoplasm and large nuclei containing prominent nucleoli, resembling HCC (Fig. 3B). The tumor cells were positive for polyclonal carcinoembryonic antigen (pCEA, 1:800, Dako, Glostrup, Denmark) and weakly positive for hepatocyte antigen (1:200, Dako, Denmark), supporting the diagnosis of HCC (Fig. 3C). There was no regional lymph node metastasis at the time of surgery and the patient is free of recurrent disease to date for over 4 months.
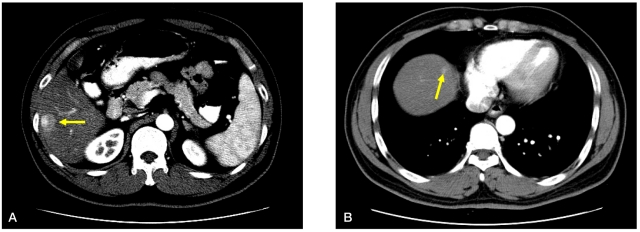
CT scans performed at the initial diagnosis of HCC. (A) The hepatic mass was a 1.7 cm-sized mass with arterial enhancement (arrow) mass in hepatic segment VI, with a patent portal vein and no metastatic lesion evident on CT scans. (B) A tiny subcapsular arterial enhancement (arrow) without early washout was noted in segment IV.
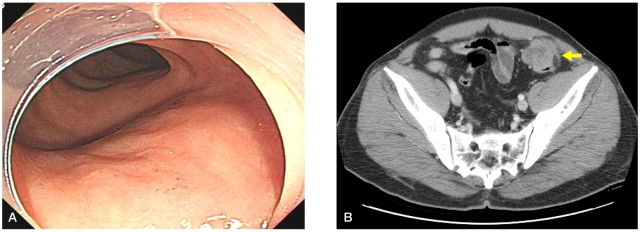
Endoscopy image and CT scan of metastatic HCC. (A) Endoscopy revealed a bulging contoured mass at 20 cm from the anal verge without a mucosal defect or diverticulum. (B) The CT scan revealed a 4×3.5 cm eccentric mass (arrow) abutting the sigmoid colon without lymph node enlargement.

Histopathology of metastatic HCC. (A) Gross specimens of sigmoid colon metastasis showing a well-defined subserosal mass. (B) The tumor cells had eosinophilic granular cytoplasms and large nuclei containing prominent nucleoli, resembling HCC (hematoxylin-eosin stain; ×400), and (C) they were positive for polyclonal carcinoembryonic antigen (pCEA) (×100).
DISCUSSION
HCC with hematogeous metastasis to colon is very rare. This case shows the typical findings of HCC metastasis to sigmoid colon.
Extrahepatic metastasis of HCC is increasing with prolonged survival and the most frequent sites of metastases are lung, bone, and lymph nodes. On the other hand, GI involvement of HCC is known to be not common. The major mode of metastasis to the GI tract is direct invasion to the contiguous GI tract via adhesion to the serosal side by a bulky tumor mass and the most frequently involved site was the duodenum, followed by the stomach, colon, and jejunum.6 Rarely, it is hypothesized that HCC may disseminate hematogenously to distant GI tracts. Portal vein thrombosis may be the key point of hematogenous spread to other sites.7,10 In our case, it is notable that the HCC was initially a small sized single mass without portal vein thrombosis and metastasized to the left-sided colon one and a half years after TACE. Hematogenous spread was suggested because the metastatic site was distant and the lymph nodes were not involved.
Endoscopic findings of GI metastasis from HCC were varied, such as a raised and centrally ulcerated lesion, mimicking gastric carcinoma, polypoid tumor, or submucosal tumor.7,11 Therefore, immunohistochemical findings are important to differentiate HCC from adenocarcinoma in the diagnosis of GI metastasis. Typically, in HCC, Cam 5.2 staining is positive whereas AE1/AE3 staining is negative.12 Polyclonal CEA is highly specific for the lining of the biliary canaliculi.13 Similarly, AFP is another reliable indicator for HCC and it has been reported to be positive in 70~90% of cases.14 In this case, the colonoscopy showed a bulging contoured tumor without any mucosal lesions, suspicious of extrinsic compression. The histopathologic findings were consistent with metastatic HCC, showing eosinophilic granular cytoplasm and large nuclei containing prominent nucleoli with immunopositivity for polyclonal CEA and hepatocyte antigen.
According to previous reports, the interval between the diagnosis of HCC and detection of GI tract involvement ranged from 3 months to 8 years.6,7,9 Mostly, GI metastasis is found in patients with advanced staged HCC. The prognosis of GI involvement from HCC is known to be poor with a median survival period of 7 months.15 However, it was suggested that treatment of extrahepatic metastases may improve survival in some selected HCC patients who have good reserved function, intrahepatic tumor stage (T0-T2), and negative portal vein invasion.16 Similarly, a previous study reported that adrenalectomy for metastatic HCC resulted in improved survival rate especially in patients with well-controlled intrahepatic lesions at the time of adrenal metastasis and good general condition.17 Although there is little data regarding the efficacy of surgical treatment in patients with haematogenous colon metastasis from HCC, our case was treated with surgical management for the metastatic HCC because the patient had good hepatic reserved function and no other metastatic lesions. The patient has been free of recurrent disease to date for over 4 months.
In conclusion, HCC with GI metastasis is uncommon and rarely spreads hematogenously to distant GI tracts. To date, the previously reported colonic metastases were located to the right side of the colon. Herein, to the best of our knowledge, we report the first case of solitary left-sided sigmoid colonic metastasis from HCC treated with surgical resection.
Abbreviations
HCC
hepatocellular carcinoma
GI
gastrointestinal
TACE
transarterial chemoembolization
CT
computed tomography
HBV
hepatitis B virus
HBsAg
hepatitis B virus surface antigen
HBeAg
hepatitis B virus e antigen
AFP
alpha-fetoprotein
CEA
carcinoembryonic antigen