Prevalence of renal dysfunction in patients with cirrhosis according to ADQI-IAC working party proposal
Article information
Abstract
Background/Aims
A revised classification system for renal dysfunction in patients with cirrhosis was proposed by the Acute Dialysis Quality Initiative and the International Ascites Club Working Group in 2011. The aim of this study was to determine the prevalence of renal dysfunction according to the criteria in this proposal.
Methods
The medical records of cirrhotic patients who were admitted to Konkuk University Hospital between 2006 and 2010 were reviewed retrospectively. The data obtained at first admission were collected. Acute kidney injury (AKI) and chronic kidney disease (CKD) were defined using the proposed diagnostic criteria of kidney dysfunction in cirrhosis.
Results
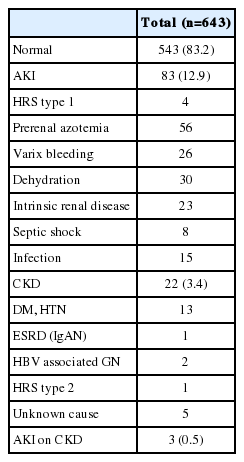
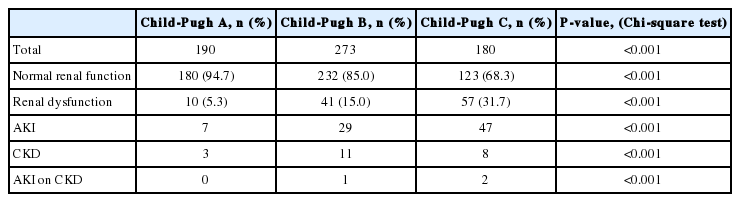
Six hundred and forty-three patients were admitted, of whom 190 (29.5%), 273 (42.5%), and 180 (28.0%) were Child-Pugh class A, B, and C, respectively. Eighty-three patients (12.9%) were diagnosed with AKI, the most common cause for which was dehydration (30 patients). Three patients had hepatorenal syndrome type 1 and 26 patients had prerenal-type AKI caused by volume deficiency after variceal bleeding. In addition, 22 patients (3.4%) were diagnosed with CKD, 1 patient with hepatorenal syndrome type 2, and 3 patients (0.5%) with AKI on CKD.
Conclusions
Both AKI and CKD are common among hospitalized cirrhotic patients, and often occur simultaneously (16.8%). The most common type of renal dysfunction was AKI (12.9%). Diagnosis of type 2 hepatorenal syndrome remains difficult. A prospective cohort study is warranted to evaluate the clinical course in cirrhotic patients with renal dysfunction.
INTRODUCTION
Kidney dysfunction is a common and potentially life-threatening event in patients with cirrhosis, and underlying mechanisms for renal dysfunction are highly variable.1,2,3 Acute kidney injury (AKI) occurs in approximately 19% of hospitalized patients with cirrhosis.4,5,6,7,8 In addition, chronic kidney disease (CKD) occurs in approximately 1% of all patients with cirrhosis.9
In a systematic review of studies evaluating predictors of survival in cirrhosis, parameters of renal dysfunction were found to be powerful predictors of death in decompensated cirrhosis, together with Child -Pugh score and its components.10,11,12 With improved understanding of pathophysiology of renal complications in cirrhosis, it is necessary to diagnose renal dysfunction in cirrhosis exactly.
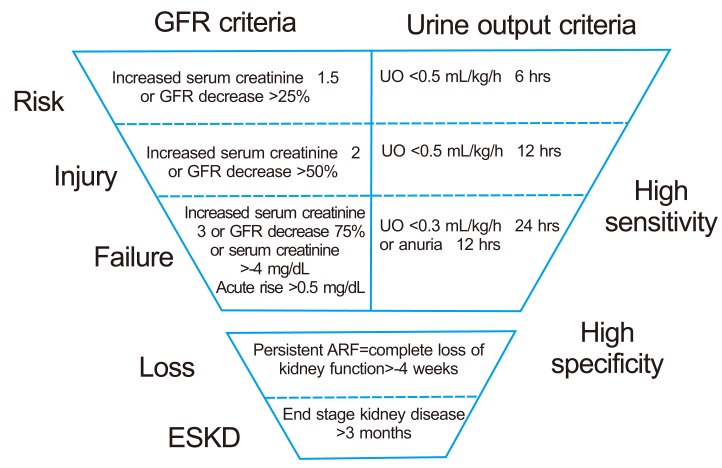
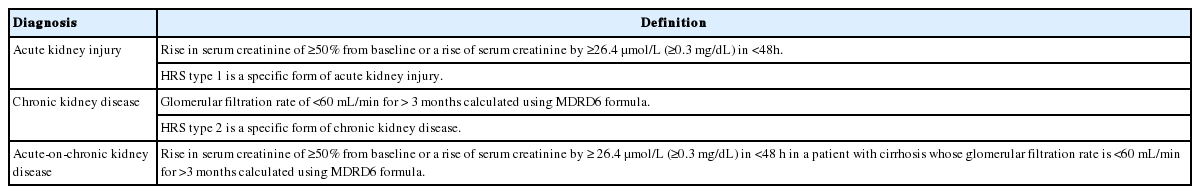
In 2004 the acute dialysis quality initiative (ADQI) Working Group developed a consensus definition and classification for AKI known as the RIFLE criteria (R: renal risk, I: injury, F: failure, L: loss of kidney function, E: endstage renal disease) which stratified acute renal dysfunction into grades of increasing severity based on changes in serum creatinine and/or urine output (Fig. 1).13 The RIFLE criteria have been validated in over 500,000 patients with AKI14,15 and have been shown to predict clinical outcomes of a progressive increase in mortality with worsening RIFLE class.16 The Acute Kidney Injury Network (AKIN), an independent collaborative network consisting of experts from ADQI and several nephrology and intensive care medicine societies, broadened the definition of AKI to include an absolute increase in serum creatinine of ≥26 mmol/l (≥0.3 mg/dL) when documented to occur within 48 h (Table 1),17 since smaller increases in serum creatinine than those considered in the RIFLE classification have been shown to be associated with an adverse outcome.18
Although serum creatinine reflects renal function in patients with compensated cirrhosis fairly accurately, patients with decompensated cirrhosis often have low serum creatinine levels relative to their glomerular filtration rate (GFR) owing to reduced production of creatinine from creatine in the liver and significant muscle wasting.19 Recognizing the inadequacy of serum creatinine as an index of renal function in cirrhosis, patients with milder degrees of renal dysfunction may not be diagnosed until advanced renal failure sets in. Thus, serum creatinine in patients with decompensated cirrhosis can still be within the normal range despite significant renal dysfunction.20
In year 2011, a revised classification system of renal dysfunction in patients with cirrhosis was proposed by the acute dialysis quality initiative (ADQI) and the international ascites club (IAC) Working Group (Table 2).21 It is a proposal to broaden the diagnosis of renal dysfunction in cirrhosis to include cases of acute and chronic renal failure not meeting the diagnostic criteria of hepatorenal syndrome types 1 and 2, respectively. The recognition of cases of renal dysfunction outside the traditional definition of hepatorenal syndrome will allow patients with lesser degrees of renal dysfunction to receive treatment. This potentially could have a positive impact on patient outcome, as patients will be treated earlier and better in the natural history of renal dysfunction. These diagnostic criteria will need to be validated in large cohorts of patients and may need to modified depending on the outcome of these studies. For the first step, we aimed to evaluate the prevalence of renal dysfunction of hospitalized patients with cirrhosis according to this proposal.
PATIENTS AND METHODS
We retrospectively reviewed medical records of cirrhotic patients aged >18 years who admitted at Konkuk university hospital from year 2006 to 2010. Six hundred and forty three patients were enrolled. The data at first admission were collected for this study. The criteria for exclusion included age younger than 18 years, liver transplantation status, and other serious diseases effect on the mortality (ie, heart failure or coronary artery disease). In addition, patients were excluded if they were diagnosed with primary (ie, hepatocellular carcinoma or cholangiocarcinoma) or metastatic malignancies, and patients who had incomplete data were also excluded (Fig. 2). This study was approved by the institutional review board of our hospital.
Definitions
Definitions of acute kidney injury (AKI), chronic kidney disease (CKD) and acute-on-chronic kidney disease (AKI on CKD) were made by proposed diagnostic criteria of kidney dysfunction in cirrhosis (Table 2). Hepatorenal syndrome type 1 (HRS type 1) and hepatorenal syndrome type 2 (HRS type 2) were defined according to the International Ascites Club (IAC).22 HRS type 1 included rapidly progressive renal failure and a doubling in serum creatinine concentrations to a level greater than 2.5 mg/dL in less than 2 weeks. Serum creatinine also did not improve (decreased to a level≤1.5 mg/dL), despite at least 2 days of diuretic cessation and optimization of intravascular blood volume with albumin and/or saline. Diagnostic criteria of HRS type 2 was same as for HRS type 1; however, HRS type 2 was defined by moderate rather than rapidly progressive renal failure with serum creatinine concentrations typically between 1.5 and 2.5 mg/dL.
Baseline creatinine was defined as the patient's creatinine value for a consistent 3months before the current hospital admission. The etiology of CKD was extracted from previous nephrology service notes and records.
Prerenal azotemia was defined using clinical and laboratory parameters. Urinary markers necessary for diagnosis included a urine specific gravity greater than 1.020 as well as a fractional excretion of sodium less than 0.01 (1%) in oliguric patients not treated with diuretics. Supporting clinical factors included tachycardia (heart rate, >90 beats per minute), hypotension (systolic blood pressure, <90 mmHg), orthostatic blood pressure changes, dry mucous membranes, other signs of decreased effective arterial blood volume in the setting of documented vomiting, prolonged diarrhea, excessive diuresis, acute hemorrhage, decreased oral intake, infection, or decreased cardiac output. In all cases, the diagnosis was dependent upon a decrease in serum creatinine with volume replacement, treatment of infection, or correction of volume status in those with clinical evidence of congestive heart failure.
Intrinsic renal dysfunction required a documented history of parenchymal renal disease in hospital records or serum creatinine values that did not improve after volume expansion and the exclusion of other etiologies of renal disease. Diagnosis of acute tubular necrosis required the presence of granular casts (epithelial cell casts) in urinary sediment, fractional excretion of sodium greater than 2%, or a urinary sodium concentration greater than 40 mmol/L, in the clinical setting of prolonged hypotension, tachycardia, sepsis, or bleeding. Nephrotic syndrome was defined by proteinuria greater than 3.5 g/d, hypoalbuminemia, hyperlipidemia, and the presence of peripheral edema. Diagnosis of acute interstitial nephritis (AIN) required clinical exposure to a known nephrotoxin and either a diagnosis of AIN in the medical record or the presence of leukocytes, leukocyte casts, and eosinophils in uninfected urine.
Postrenal renal dysfunction was confirmed by imaging demonstrating hydronephrosis in the setting of oliguria or anuria.
Clinical cirrhosis was defined as radiologic features of cirrhosis with thrombocytopenia, esophageal varices, ascites, or encephalopathy. The ascites was assessed by physical examination or radiologic examination. The etiology of cirrhosis was determined according to the following criteria. Hepatitis B cirrhosis was defined by the presence of cirrhosis in patients with hepatitis B surface antigen, hepatitis C cirrhosis was defined by the presence of cirrhosis in a person with hepatitis C virus (HCV) RNA, alcoholic cirrhosis was determined from the provider's note in the presence of a history of alcohol abuse or dependence and the absence of other potential causes of liver disease, and other causes of cirrhosis were determined by using standard diagnostic criteria (ie, serologies, histology, iron studies).
Statistical analysis
Demographics, and clinical and laboratory characteristics of the patients were summarized using descriptive statistics. Child-Pugh score was calculated. Continuous variables were summarized by mean and standard deviation. Categorical variables were compared using Chi-square test. Two-sided null hypotheses of no difference were rejected if p-values were less than .05. SPSS Version 17.0 (SPSS, Inc, an IBM Company, Chicago, Illinois, USA) was used for statistical analysis.
RESULTS
Of the 882 patients with cirrhosis and ascites, 239 were excluded (malignancy in 81, liver transplantation status in 19, coronary artery disease and heart failure in 1, liver abscess in 1, incomplete data in 134). Thus, 643 patients were included in the present study (Fig. 2).
Six hundred and forty three patients were enrolled from year 2006 to 2010. Demographic and clinical characteristics are shown in Table 3. Most of the patients were male (n=478, 74.3%) and mean age was 57.4±11.3 years. The most common etiology of cirrhosis was alcohol (n=320, 49.8%), followed by HBV infection (n=202, 31.4%). Mean albumin was 3.1±0.7 (g/dL) and mean total bilirubin was 4.8±7.2 (mg/dL). Mean creatinine and mean eGFR was 1.3±1.0 (mg/dL) and 65.6±25.1 (ml/min/1.73 m2). Mean prothrombin time (PT) was 1.5±0.6 (INR).
Child-Pugh class A, B and C was 190 (29.5%), 273 (42.5%) and 180 (28.0%) (Table 4). Renal dysfunction that occurred in each group was 10 (5.3%), 41 (15.3%), and 57 (31.7%). In the cirrhotic patients with higher severity of cirrhosis, renal dysfunction was developed much more (P<0.001).
Rate of renal dysfunction classified by cirrhosis severity according to the Child-Pugh classification
The type and cause of renal dysfunction from year 2006 to 2010 are presented in Table 5. The most common type of renal dysfunction was AKI, present in 83 patients (12.9%). Dehydration was the most common cause of AKI, present in 30 patients (36.1%). 3 patients (3.6%) were diagnosed with hepatorenal syndrome type 1 and 26 patients (31.3%) were pre-renal type AKI caused by volume deficiency after variceal bleeding. Eight patients (9.6%) were diagnosed with AKI induced by septic shock.
On the other hand, CKD was found in 22 patients (3.4%). One of these patients (4.5%) had already preexisting end stage renal disease (ESRD) induced by IgA nephropathy and 13 patients (59.1%) had underlying diabetes or hypertension. Two patients (9.0%) were diagnosed with HBV associated glomerulonephritis. Five patients (22.7%) had unknown cause of chronic renal insufficiency. One patient (4.5%) was diagnosed with HRS type 2. AKI on CKD was found in 3 patients (0.5%).
Overall hospital mortality rate in patients with cirrhosis and renal insufficiency was 22.3%. Mortality rates by type of renal insufficiency are presented in Table 6. The highest mortality rate was seen in patients with AKI on CKD (66.7%). Mortality for those with AKI was 22.1%, and mortality for those with CKD was 17.4%. Among these patients, 8 (32%) died of varix bleeding, 4 (16%) died of hepatic encephalopathy, 4 (16%) died of hepatorenal syndrome (4 patients were diagnosed with HRS type 1 and they all died during hospitalization.), and 5 (20%) died of profound hepatic failure. Four patients died of other than liver disease (pneumonia, sepsis, acute respiratory distress syndrome were included.)
DISCUSSION
Prevalence of renal dysfunction in cirrhosis is not infrequent (16.8%). In this study, the most common type of renal dysfunction was AKI, which accounted for 12.9% of cases and was usually the result of prerenal azotemia (67.4%), consistent with previous studies.4,5,6,7,8,23,24 In turn, the most common cause of prerenal azotemia was dehydration (36.1%), followed by varix bleeding (31.3%). Dehydration was developed secondary to diuretics, lactulose-induced diarrhea and poor oral intake. Postrenal causes of AKI in cirrhosis are rare and represent less than 1% of the cases in other study,23 there was no patients with postrenal cause of AKI in our cohort.
We found that CKD was diagnosed in 3.4% of hospitalized patients with cirrhosis. In the cirrhotic patients with higher severity of cirrhosis, renal dysfunction including AKI, CKD and AKI on CKD was developed much more.
HRS type 1 has been studied extensively and is widely accepted as associated with a very poor outcome.9,25 Approximately 3.6% of patients with AKI in our study had HRS type 1. This is in contrast to previously published work, in which HRS type 1 has been shown to account for approximately 11% of AKI.26 This discrepancy may be a result of imprecision in definitions of HRS type 1 or inherent differences between previous and current diagnostic criteria.22,27
Diagnosis of HRS type 2 was still difficult and diagnosis of AKI on CKD needs long term follow up evaluation of renal function in cirrhotic patients. We had known that HRS was a unique potentially reversible form of ARF secondary to renal vasoconstriction that results from extreme vasodilatation.28,29 But, it is possible that HRS type 2, as currently defined, is not a unique functional kidney disorder. This syndrome may simply be a reflection of previously undiagnosed intrinsic renal pathology30 or simply because of prerenal AKI. The most recent diagnostic criteria for HRS clearly delineated which patients should be regarded as having HRS and therefore receive specific treatment. However, the rigid cut-off value of a serum creatinine level of 133 mmol/l (1.5 mg/dl) may limit treatment to patients with the most severe degree of renal dysfunction. The changes that predispose to the development of HRS are not an 'all-or-none' phenomenon, but rather evolve progressively with the natural history of cirrhosis.21 It is unclear whether patients who have milder degrees of renal dysfunction will also experience adverse outcomes.21 If so, they should also be offered treatment early rather than waiting until the diagnostic criteria of HRS are reached.
Differentiation among the three main causes of AKI may be difficult in patients with cirrhosis because the clinical presentations do not match classical paradigms and, factors that lead to prerenal azotemia can precipitate HRS and can also precipitate ATN.9
Differentiation between prerenal azotemia and HRS also may be difficult. By definition, prerenal azotemia improves with volume expansion. However, assessment of exact intravascular volume deficit in a patient who is already total body sodium overloaded is difficult; the rate of fluid administration is unspecified, and thus the rate of response in serum creatinine is highly variable and often incomplete.9
It is important to recognize several limitations of this study. First, the retrospective nature of this study presents difficulties with the precise determination of the etiologies of renal dysfunction and, theoretically, could be a source of misclassification. To alleviate this potential limitation, we excluded patients that were unable to be adequately categorized according to predetermined definitions. Second, this study was conducted at a single center. Clinical settings have to be evaluated with a multi-center prospective study. Finally, data collection for this investigation ended at the time of the first admission, and hence, there was no long-term follow-up for determination of long-term patient outcomes. A prospective study capturing real-time laboratory and clinical characteristics may be beneficial and, in addition, might allow a better understanding of the natural history of renal dysfunction in cirrhosis.
In conclusion, both acute and chronic renal dysfunction are common in hospitalized patients with cirrhosis. The most common type of renal dysfunction was AKI (12.9%), and the most common cause of AKI was prerenal azotemia (67.4%), which was developed secondary to dehydration (36.1%) and varix bleeding (31.3%). Further and larger prospective studies are warranted to assess the ability of new criteria vs. the conventional criteria of renal dysfunction to predict clinical outcomes in patients with cirrhosis, as suggested by a recent Working Party.21 Additionally, future studies are clearly needed to better define diagnostic criteria of HRS type 2.
Notes
The authors have no conflicts to disclose.
Abbreviations
ADQI-IAC
acute dialysis quality initiative and the international ascites club
AIN
acute interstitial nephritis
AKI
acute kidney injury
ALT
alanine aminotransferase
AST
aspartate aminotransferase
BUN
blood urea nitrogen
CHB
chronic hepatitis B
CKD
chronic kidney disease
DM
diabetes mellitus
GFR
glomerular filtration rate
HBV
hepatitis B virus
HCV
hepatitis C virus
HRS
hepatorenal syndrome
HTN
hypertension
PT
prothrombin time
UTI
urinary tract infection