Changes in the seroprevalence of IgG anti-hepatitis A virus between 2001 and 2013: experience at a single center in Korea
Article information
Abstract
Background/Aims
The incidence of symptomatic hepatitis A reportedly increased among 20- to 40-year-old Korean during the late 2000s. Vaccination against hepatitis A was commenced in the late 1990s and was extended to children aged <10 years. In the present study we analyzed the changes in the seroprevalence of IgG anti-hepatitis A virus (HAV) over the past 13 years.
Methods
Overall, 4903 subjects who visited our hospital between January 2001 and December 2013 were studied. The seroprevalence of IgG anti-HAV was analyzed according to age and sex. In addition, the seroprevalence of IgG anti-HAV was compared among 12 age groups and among the following time periods: early 2000s (2001-2003), mid-to-late 2000s (2006-2008), and early 2010s (2011-2013). The chi-square test for trend was used for statistical analysis.
Results
The seroprevalence of IgG anti-HAV did not differ significantly between the sexes. Furthermore, compared to the seroprevalence of IgG anti-HAV in the early 2000s and mid-to-late 2000s, that in the early 2010s was markedly increased among individuals aged 1-14 years and decreased among those aged 25-44 years (P<0.01). We also found that the seroprevalence of IgG anti-HAV in individuals aged 25-44 years in the early 2010s was lower than that in the early 2000s and mid-to-late 2000s.
Conclusions
The number of symptomatic HAV infection cases in Korea is decreasing, but the seroprevalence of IgG anti-HAV is low in the active population.
INTRODUCTION
Hepatitis A is an infectious disease caused by the hepatitis A virus (HAV), which is transmitted by the fecal-to-oral route. Common vehicles of transmission are polluted water and contaminated foods, which mostly occur under conditions of poor hygiene. In both developing and developed countries, most cases of HAV infection are asymptomatic and occur during adolescence or infancy. In the event that symptoms occur, the most likely one is mild jaundice. In developed countries, high prevalence of HAV infection is seen in adults and it usually manifests with severe symptoms like jaundice.1
In the late 2000s, several studies showed a rise in symptomatic hepatitis A cases among 20-40-year-old individuals in Korea.2,3 HAV infection was not included among the nationally notifiable communicable diseases in Korea before 2000, owing to which the exact prevalence of HAV infection was difficult to estimate. After 2000, the Korea Centers for Disease Control and Prevention (KCDC) designated HAV infection a contagious disease,4,5 and in 2011, as a Class I nationally notifiable communicable disease.6
Pediatric immunization is a well-established measure and was introduced in 1997; however, research on adult immunization, which was established only in 2012, are lacking. Several recent studies show that individuals aged 20-40 years had a low seroprevalence of IgG anti-HAV.5,7,8 Considering the recent national prevalence and epidemiology of HAV infection, the Korean Society of Infectious Diseases published recommendations for vaccination against HAV, which comprised information on the vaccine's indication and target.
The indication for the HAV vaccine differs according to patient age. Patients aged under 30 years should be vaccinated without serologic testing even if they are not at high risk, and those aged above 30 years should be vaccinated despite negative serologic tests.9
In this study, we aimed to determine the seroprevalence of IgG anti-HAV in the early 2010s, as vaccination was implemented after the symptomatic HAV surge in 2009, and compare it to those in the early 2000s and mid to late 2000s.
MATERIALS AND METHODS
Patients
We studied 4903 patients (age range: 1-54 years) who visited Hanyang Guri Hospital from January 2001 to December 2013. To study the trend of IgG anti-HAV seroprevalence according to age, the patients were stratified into the following 12 age groups based on 5-year intervals: <1, 1-4, 5-9, 10-14, 15-19, 20-24, 25-29, 30-34, 35-39, 40-44, 45-49, and 50-54 years. We excluded patients who had undergone transfusion in the past 6 months or showed evidence of HAV infection at the time of examination. The Hanyang University Guri Hospital Institutional Review Board (No 2014-03-003) approved this study.
Methods
The serum IgG anti-HAV levels were measured using an electrochemiluminescence immune analyzer (Modular E170, Roche) and compared according to age and sex for a 13-year period classified into 3 time periods: early 2000s (2001-2003), mid to late 2000s (2006-2008), and early 2010s (2011-2013).
Statistical analyses
All statistical analyses were performed using SPSS 18.0. The data obtained were analyzed for age, sex, and the 3 time periods. The Chi-square test and Chi-square test for trend were used for analyzing data according to sex and the 3 time periods, respectively. Statistical significance was set at P<0.05.
RESULTS
Comparison of IgG Anti-HAV prevalence by age and sex
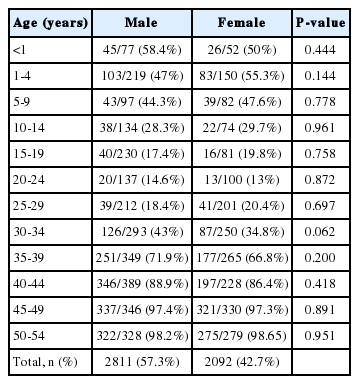
Of the 4903 patients in our study, 2811 (57.3%) were male and 2092 (42.7%) were female (Table 1). The IgG anti-HAV seroprevalence data were obtained and analyzed according to age and sex. No significant difference was found according to age or sex (Table 1 and Fig. 1).
Comparison of IgG Anti-HAV prevalence by age and time periods
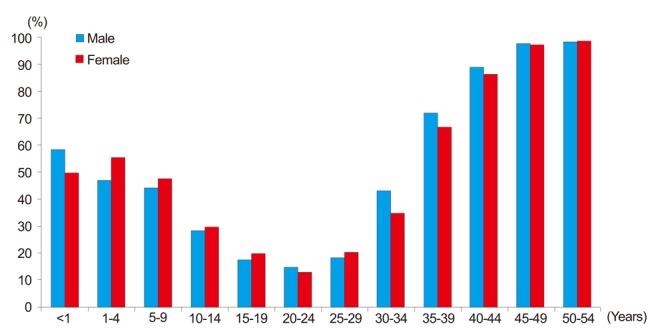
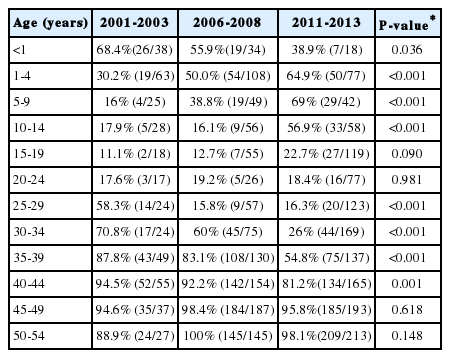
The IgG anti-HAV seroprevalence during the early 2000s is as follows: <1 year, 68.4%; 1-4 years, 30.2%; 5-9 years, 16%; 10-14 years, 17.9%; 15-19 years, 11.1%; 20-24 years, 17.6%; 25-29 years, 58.3%; 30-34 years, 70.8%; 35-39 years, 87.8%; 40-44 years, 94.5%; 45-49 years, 94.6%, and 50-54, 88.9%.
The IgG anti-HAV seroprevalence during the mid to late 2000s is as follows: <1 year, 55.9%; 1-4 years, 50%; 5-9 years, 38.8%; 10-14 years, 16.1%; 15-19 years, 12.7%; 20-24 years, 19.2%; 25-29 years, 15.8%; 30-34 years, 60%; 35-39 years, 83.1%; 40-44 years, 92.2%; 45-49 years, 98.4%, and 50-54 years, 100%.
The IgG anti-HAV seroprevalence during the early 2010s is as follows: <1 year, 38.9%; 1-4 years, 64.9%; 5-9 years, 69%; 10-14 years, 56.9%; 15-19 years, 22.7%; 20-24 years, 18.4%; 25-29 years, 16.3%; 30-34 years, 26%; 35-39 years, 54.8%; 40-44 years, 81.2%; 45-49 years, 95.8%, and 50-54 years, 98.1%.
Thus, we found that the seroprevalence of IgG anti-HAV in patients aged 1-14 years increased significantly, while in those aged 25-44 years decreased significantly (P<0.05, Table 2 and Fig. 2).
Comparison of IgG anti-HAV prevalence rates between the early 2000s, mid 2000s, and early 2010s according to age group
DISCUSSION
In this study, we analyzed the changes in IgG anti-HAV seroprevalence in patients who visited a single hospital. We divided the study into 3 time periods on the basis of the fact that the prevalence of HAV peaked in 2009.10,11 We compared data from the early 2000s and early 2010s, the periods before and after the prevalence of HAV peaked. We also analyzed data from 2006-2007, which was just before the prevalence of HAV peaked, that is, 2009. Thus, we focused on analyzing the IgG anti-HAV seroprevalence in the early 2010s, wherein patients aged 25-44 years showed a significant decrease in IgG anti-HAV seroprevalence compared to that in the early 2000s and mid to late 2000s. We also studied the IgG anti-HAV seroprevalence according to age groups based on 5-year intervals. Furthermore, we compared the pattern and age-specific trend of IgG anti-HAV seroprevalence (Table 2).
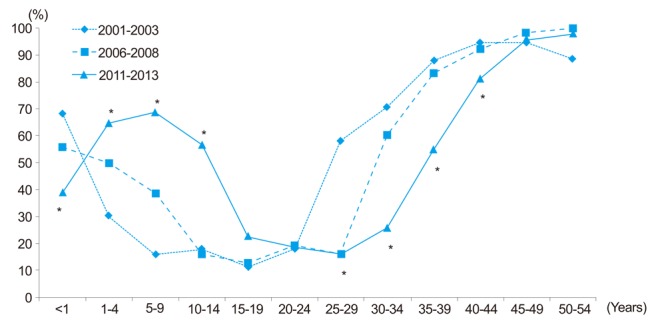
Recently, the KCDC investigated the number of hepatitis A cases since 2001: less than 400 cases were reported in 2001-2004, about 800 in 2005, about 2000 in 2006 and 2007, about 7,900 in 2008, and about 15,000 in 2009. Further, recent data show that the prevalence of HAV infection has decreased, from 10.91/100,000 cases in 2011 to 2.35/100,000 cases in 2012 (Fig. 3A).10 These data correspond with those obtained from our study that was conducted during the same period at our hospital, with similar annual prevalence rates (Fig. 3B), and demonstrate the rapid increase in the prevalence of HAV until 2009, which then decreased in 2010. Our hospital survey stated that its HAV prevalence pattern (Fig. 3B) was similar to that of the entire country (Fig. 3A): both figures show a similar pattern of hepatitis A occurrence. This confirms that the number of patients with IgG anti-HAV seroprevalence has been decreasing since the peak in 2009.

(A) Prevalence of reported acute hepatitis A infection in Korea during 2001-2013. (B) Incidence of acute hepatitis A infection in our hospital during the same period.
Previously, hepatitis A was mostly found in children below 10 years of age.12,13 However, in recent years, the common age range for HAV infection was found to be 10-29 years.3,12,14,15 In our study as well, the group with the highest risk for HAV infection was the 10-29-year age group, and an increasing susceptibility was seen in active populations such as the 30-39-year and 40-49-years age groups.2,3,16
In the early 2000s (2001-2003), Korea's hepatitis A outbreak pattern was similar to that in developing countries, but in recent years, it was similar to those observed in developed countries. The age of onset, in particular, is 20-40 years.1,2,3 One study showed that the age of onset for symptomatic apparent hepatitis was 29 years.17
In Korea, vaccination against HAV began in 1997.2,12,16 Recent studies showed that about 40% of infants aged 1-10 months had received vaccination.1,18,19 A study conducted in the Busan area analyzed individuals aged 5-24 years from April 2012 to November 2012, and revealed that the seroprevalence of IgG anti-HAV was lower in individuals aged 15-24 years.20 It is possible that these individuals were not vaccinated during infancy. Several other studies showed that individuals aged 1-14 years had a significantly high IgG anti-HAV seroprevalence, which is similar to the results obtained in our study12,16,17,21 and possibly due to the increase in HAV vaccination. Compared to the early 2000s and mid to late 2000s, the seroprevalence of IgG anti-HAV in children below 1 year of age decreased in the early 2010s. This is probably because the seroprevalence of IgG anti-HAV is low in women of child-bearing age.22 We suggest that childbearing aged women may be vaccinated to reduce their susceptibility in case of a hepatitis A outbreak. Therefore, the tendency of periodic examinations, owing to vaccination and the age-cohort effect, caused the IgG anti-HAV seroprevalence pattern to change from a U to a sine pattern (Fig. 1).12
The cost-effectiveness analysis of different vaccination strategies in the United States revealed that screening for IgG anti-HAV was less costly than vaccination, without examining HAV serology, when the IgG anti-HAV prevalence exceeded 35% and the cost of serological testing was less than 25 USD (~26,000 won).23 To date, there is no study about the cost-effectiveness of vaccination in Korea. According to expert opinion, in Korea, because the cost of vaccination was about 10 times higher than that of the serum antibody test, the general population aged 10-20 years with an IgG anti-HAV seroprevalence below 10% should be vaccinated without antibody testing.17
Our results show that seroprevalence of IgG anti-HAV had significantly decreased to lower than 30% in individuals aged 30-34 years compared to that in the late 2000s.21,24 Therefore, seropositivity decreased as age increased, and we believe that this was the age-cohort effect: as the population grew older, they acquired a lower seroprevalence of IgG anti-HAV. We suggest that the current guidelines, which were established in 2012, be modified to accommodate a proper vaccination strategy that involves age expansion or catch-up schedules.
However, our study has some limitations. First, this is a single-hospital study conducted in the Gyeonggi region. Our results cannot be extrapolated to other institutions or regions. Second, this study did not take into account the socio-economic status or area of residence of the patients. This study was conducted in a small- and medium-sized city, in which the urban and rural communities coexisted. Further, our study did not involve socioeconomic or residential environment status analysis. Previous research showed that the areas between Seoul and Gyeonggi did not differ in terms of the seroprevalence of IgG anti-HAV.25 Third, our study was a retrospective study that could not include previous vaccinations and underlying diseases. However, the data obtained is reflective of current clinical practices associated with HAV infection. Despite these limitations, our results were found to be similar to those for the entire country using the sample monitoring system.
In summary, due to the vaccination and age-cohort effect, we found that the seroprevalence of IgG anti-HAV in individuals aged 25-44 years in the early 2010s was lower than that in the early 2000s and mid to late 2000s. However, the seroprevalence of IgG anti-HAV in those aged 1-14 years was found to be increased.
In conclusion, the number of symptomatic HAV infection cases in Korea is decreasing, but the seroprevalence of IgG anti-HAV is lower in the active population. This active population appears to have lower immunity and be more susceptible towards HAV. Low immunity to HAV makes people more infectious to HAV, especially in case of a severe outbreak. Thus, we suggest that future studies focus on age expansion, catch-up scheduled vaccination, or other treatment measures.
Notes
The authors have no conflicts to disclose.
Abbreviations
HAV
hepatitis A virus
IgG
immunoglobulin G
KCDC
Korea Centers for Disease Control and Prevention