Comparison between obese and non-obese nonalcoholic fatty liver disease
Article information
Abstract
Nonalcoholic fatty liver disease (NAFLD) encompasses a spectrum of liver conditions that are characterized by excess accumulation of fat in the liver, and is diagnosed after exclusion of significant alcohol intake and other causes of chronic liver disease. In the majority of cases, NAFLD is associated with overnutrition and obesity, although it may be also found in lean or non-obese individuals. It has been estimated that 19.2% of NAFLD patients are lean and 40.8% are non-obese. The proportion of patients with more severe liver disease and the incidence of all-cause mortality, liver-related mortality, and cardiovascular mortality among non-obese and obese NAFLD patients varies across studies and may be confounded by selection bias, underestimation of alcohol intake, and unaccounted weight changes over time. Genetic factors may have a greater effect towards the development of NAFLD in lean or non-obese individuals, but the effect may be less pronounced in the presence of strong environmental factors, such as poor dietary choices and a sedentary lifestyle, as body mass index increases in the obese state. Overall, non-invasive tests, such as the Fibrosis-4 index, NAFLD fibrosis score, and liver stiffness measurement, perform better in lean or non-obese patients compared to obese patients. Lifestyle intervention works in non-obese patients, and less amount of weight loss may be required to achieve similar results compared to obese patients. Pharmacological therapy in non-obese NAFLD patients may require special consideration and a different approach compared to obese patients.
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) encompasses a spectrum of liver conditions that are characterized by excess accumulation of fat in the liver. The diagnosis is made following the exclusion of significant alcohol intake and other causes of chronic liver disease [1,2]. In the majority of cases, NAFLD is associated with overnutrition and obesity, although it may be also found in non-obese patients. The condition is closely associated with metabolic syndrome, which is a constellation of risk factors for cardiovascular disease [3]. The prevalence of NAFLD has been increasing, and it is recognized as the most common cause of chronic liver disease worldwide [4,5]. In 2020, an international panel of experts proposed a new term, “metabolic dysfunction-associated fatty liver disease (MAFLD),” which is diagnosed in persons with fatty liver in the presence of overweight or obesity, type 2 diabetes mellitus, or at least two metabolic risk abnormalities [6]. The present review primarily focuses on the comparison between obese and non-obese NAFLD, for which there is a richer body of literature, given that the term NAFLD has been in existence for a much longer period of time. However, the literature on MAFLD is rapidly expanding, and a similar review on MAFLD in due time would be of great interest. In general, a body mass index (BMI) cut-off of 25 and 30 kg/m2 is used for the definition of obesity for Asian and Caucasian populations, respectively. In studies using the term “lean NAFLD,” the nonlean patients included those who were overweight, defined by a BMI of ≥23 and ≥25 kg/m2 for Asian and Caucasian populations, respectively.
EPIDEMIOLOGY AND NATURAL HISTORY OF NON-OBESE NAFLD
Initial recognition and increasing interest
One of the earliest reports on non-obese NAFLD came from India. In a study on 1,911 subjects from the rural administrative unit of West Bengal that was published in 2013, Das and colleagues found the prevalence of NAFLD to be 8.7%. While this was relatively low compared to studies from other parts of India, the prevalence was considerably high, given that the majority of study subjects were young, physically active, less affluent, and non-obese. The term “third-world NAFLD” was used to describe this phenotype, where instead of overt obesity, subtle measures of increased adiposity predisposed to NAFLD [7]. The interest in non-obese NAFLD sky-rocketed after an abstract was presented at the Digestive Disease Week in the following year. In a study on 1,090 biopsy-proven NAFLD patients who were followed for 133 months, Dela Cruz and colleagues found that lean NAFLD patients had a significantly shorter survival compared to non-lean NAFLD patients [8]. Subsequently, a population-based study on 911 patients using proton-magnetic resonance spectroscopy and transient elastography in Hong Kong found non-obese patients to have less severe liver disease based on significantly lower serum cytokeratin-18 level and liver stiffness measurement [9]. Furthermore, in another study on 307 biopsy-proven NAFLD patients, non-obese NAFLD patients had significantly lower serum cytokeratin-18 level, liver stiffness measurement, and histological fibrosis stage. During follow-up, six patients died, two developed hepatocellular carcinoma, and one had liver failure, all of whom in the obese patients [10].
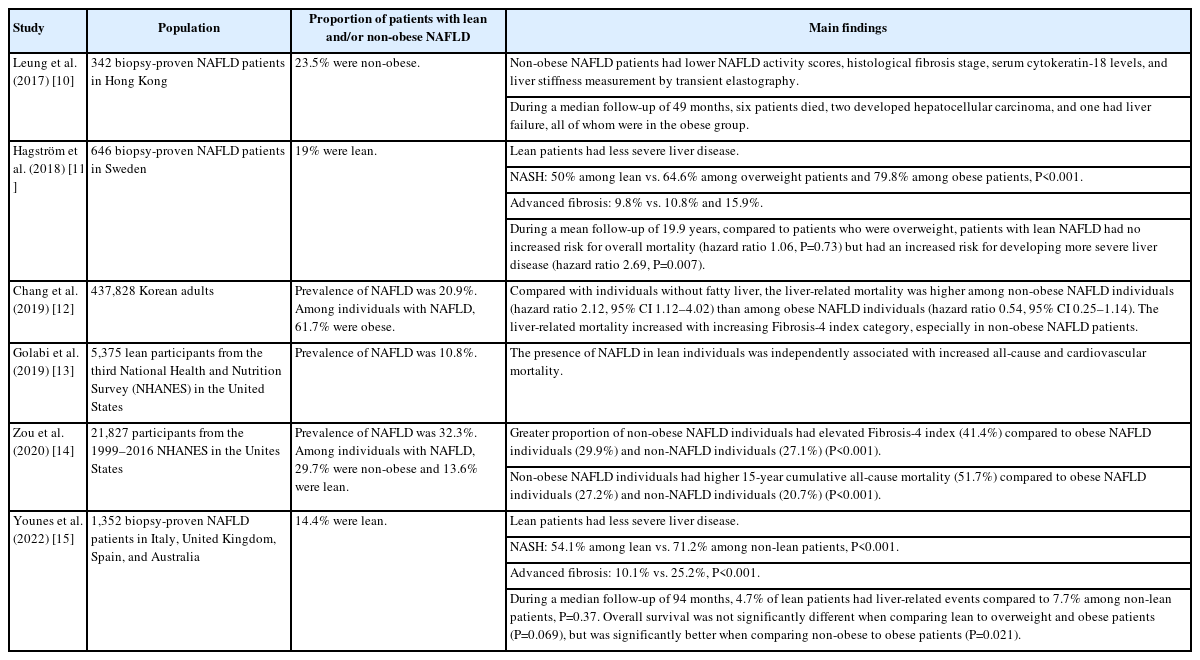
Possible reasons for disparities in data
Several other longitudinal studies have shown conflicting results (Table 1) [11-15]. A study in Sweden found that patients with lean NAFLD were paradoxically more likely to develop develop severe liver disease, despite having less severe liver disease at baseline, compared to non-lean patients [11]. Further studies are warranted to understand the reasons behind these inconsistent findings. One possible explanation is that the lean NAFLD patients in the study had more severe liver disease than expected compared to the general population, which could be expected given that the patients were seen in a secondary or tertiary care setting and underwent liver biopsy. This was evident from the high proportion of lean patients with nonalcoholic steatohepatitis (NASH) and advanced liver fibrosis at 50% and 9.8%, respectively. Furthermore, important confounding factors, such as changes in alcohol intake and body weight over time, were not taken into account. Alcohol intake is an important confounding factor and may not be adequately captured due to under-reporting. In a study on 184 patients, repeated moderate to excessive alcohol intake was detected in 28.6% of patients with presumed NAFLD, and patients with repeated moderate to excessive alcohol intake had significantly lower BMI [16]. This may partly contribute to the high proportion of lean or non-obese NAFLD patients with more severe liver disease. Assessment of alcohol intake by ethylglucuronide in hair had an area under curve of 0.93 for the detection of repeated moderate to excessive alcohol consumption [16], which may be useful to more accurately classify patients with fatty liver as NAFLD or not.
Epidemiology and clinical characteristics
A systematic review and meta-analysis estimated the prevalence of lean NAFLD and non-obese NAFLD in the general population to be 5.1% (95% confidence interval [CI] 3.7–7.0%) and 12.1% (95% CI 9.3–15.6%), respectively. Among NAFLD patients, an estimated 19.2% (95% CI 15.9–23.0%) were lean and 40.8% (95% CI 36.6–45.1%) were non-obese. Among patients with non-obese or lean NAFLD, 39.0% (95% CI 24.1–56.3%) had NASH, 29.2% (95% CI 21.9–37.9%) had significant fibrosis, and 3.2% (95% CI 1.5–5.7%) had cirrhosis. The corresponding rates among obese NAFLD were 52.9% (95% CI 38.3–67.0%), 38.3% (95% CI 30.6–46.6%), and 2.0% (95% CI 0.4–5.7%). In the largest multicenter biopsy-proven NAFLD registry in Asia to date consisting of 1,812 patients, 21.6% of patients were non-obese. The proportion of patients with NASH and advanced liver fibrosis among non-obese NAFLD patients were 50.5% and 14%, respectively, while the corresponding rates among obese NAFLD patients were 56.5% and 18.7%, respectively [17].
Natural history and prognosis
The incidence rates of all-cause mortality, liver-related mortality, and cardiovascular-related mortality among patients with lean or non-obese NAFLD were found to be 12.1 (95% CI 0.5–38.8), 4.1 (95% CI 1.9–7.1), and 4.0 (95% CI 0.1–14.9) per 1,000 person-years, respectively. The corresponding rates among obese NAFLD patients were 7.5 (95% CI 0–33.6), 2.4 (95% CI 1.0–4.4), and 2.4 (95% 0–13.3) per 1,000 person-years, respectively (Fig. 1) [18]. Although it appeared that lean or non-obese NAFLD patients have higher all-cause mortality, liver-related mortality, and cardiovascular mortality, the results should be interpreted with caution due to the small number of related studies. The authors have also cautioned that further research is needed before any conclusions are made on this due to the scarcity of data for obese and non-obese populations [18]. The results on all-cause mortality, liver-related mortality, and cardiovascular mortality were based on only three studies. Furthermore, only one study provided all-cause mortality, cardiovascular mortality, and liver-related mortality for lean and non-lean NAFLD patients [11]; another study provided all-cause mortality and cardiovascular mortality for obese and non-obese NAFLD patients [12]; a third study provided all-cause mortality and cardiovascular mortality only for non-obese NAFLD patients [13].
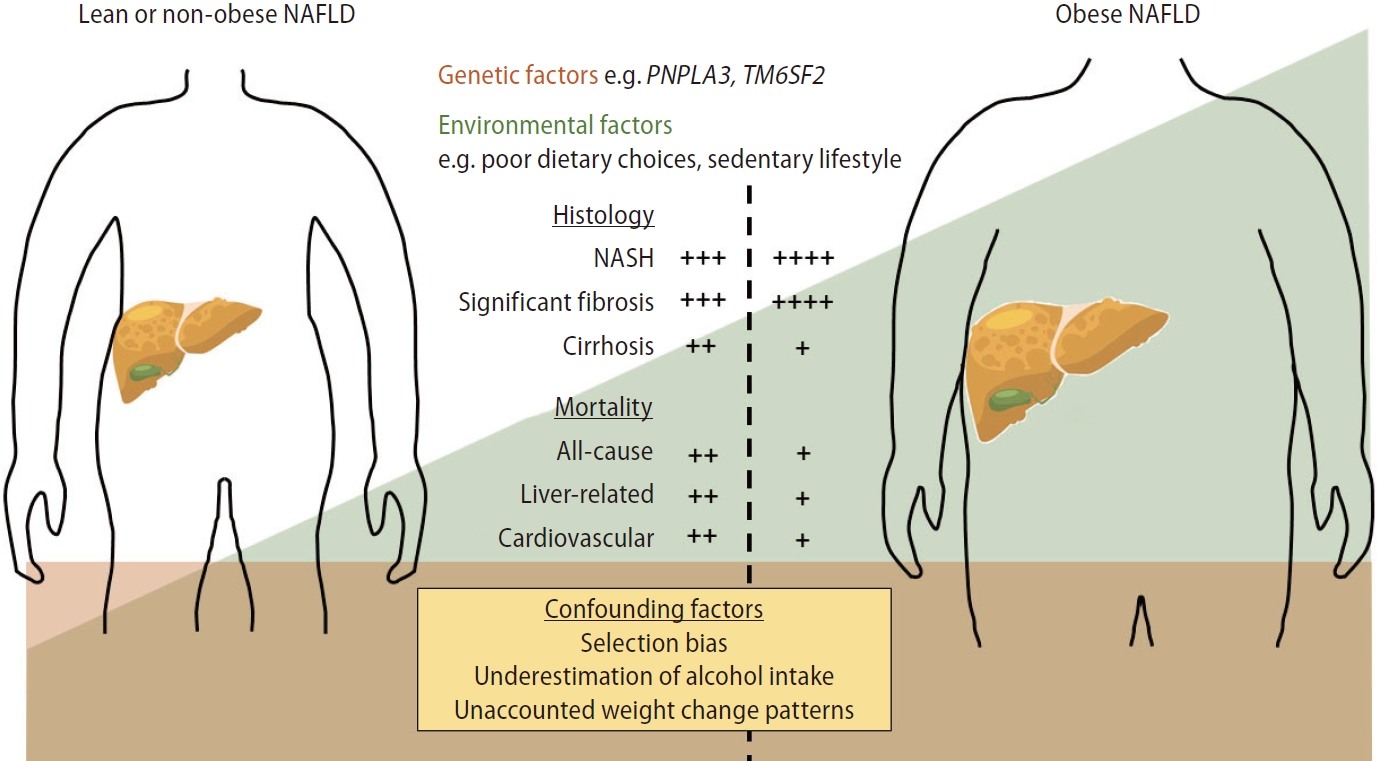
The effect of genetic, environmental, and confounding factors in the severity of liver disease and outcomes of lean or non-obese patients compared with obese NAFLD patients. Genetic factors may have a more pronounced effect towards the development of NAFLD in lean or non-obese individuals, but the effect may appear less pronounced in the presence of strong environmental factors, such as poor dietary choices and a sedentary lifestyle, in the obese state. Selection bias, underestimation of alcohol intake, and unaccounted weight loss over time from poorly controlled diabetes mellitus and/or loss of muscle mass from advanced liver disease are important confounding factors for varying severity of liver disease and outcomes in lean or non-obese NAFLD patients compared to obese NAFLD patients, although genetic factors may play a role. NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; PNPLA3, patatin-like phospholipase domaincontaining- 3; TM6SF2, transmembrane 6 superfamily member 2. +: Relative frequency of the corresponding variable when comparing between lean or non-obese NAFLD and obese NAFLD.
PATHOPHYSIOLOGY OF NON-OBESE NAFLD
The role of obesity and lipotoxicity in the development of NAFLD and NASH has been well described [19]. Briefly, obesity and insulin resistance lead to excess free fatty acids and increased de novo lipogenesis in the liver. Free fatty acids are either stored as triglyceride, exported from the liver, or undergo oxidation. The excess in free fatty acids causes oxidative stress, liver cell injury and death, inflammation, and eventually fibrosis. On the other hand, the pathophysiology of lean or non-obese NAFLD is not completely understood. Despite having a normal or lower BMI, lean or non-obese NAFLD patients have excess visceral adiposity. Lean or non-obese NAFLD patients share common altered metabolic and cardiovascular profile as their non-lean or obese counterparts, although the alterations are generally less severe [20]. While it is reasonable to think that lean or non-obese NAFLD is the early phase of NAFLD or the less severe end of the NAFLD spectrum, evidence suggests that there may be more to it.
Ethnic differences in body fat distribution and genetic factors
It is well-known that different ethnic groups have different tendency to accumulate visceral and liver fat and to develop metabolic syndrome. Ethnic difference in the prevalence of hepatic steatosis was first pointed out in the landmark paper by Browning and colleagues in 2004, where Hispanics were found to have the highest prevalence of hepatic steatosis, while the prevalence was significantly lower among Blacks despite an equally high prevalence of obesity and insulin resistance [21]. In a subsequent multi-ethnic cohort study on 1,794 subjects of African, European, Japanese, Latino, or Native Hawaiian ancestry in the United States, the mean visceral and liver fat were greatest among the Japanese Americans, which jointly accounted for a statistically significant fraction of the difference in metabolic syndrome prevalence compared to other ethnic groups independently of total fat mass [22]. Studies on multi-ethnic Malaysians have also consistently found the prevalence of NAFLD to be higher among the Indians and Malays compared to the Chinese [23,24], with the ethnic predilection seen as early as young adulthood [25]. Consistent with this is the greater prevalence of metabolic syndrome among the Indians and Malays compared with the Chinese [26]. The difference in tendency for visceral adiposity, NAFLD, and metabolic syndrome between the different ethnic groups may be explained by genetic differences. A single nucleotide polymorphism in the patatin-like phospholipase domain-containing-3 (PNPLA3) gene, the rs738409 C>G variant, which results in substitution of isoleucine by methionine at position 148 (I148M), was found to be associated with increased liver fat in a genome-wide association study, and the risk allele was found to be the highest among Hispanics and the lowest among Blacks [27], providing an explanation to the initial observation by Browning and colleagues. Genetic polymorphisms in the PNPLA3 gene have subsequently been recognized as a major genetic determinant of NAFLD and its severity [28]. The PNPLA3 protein has lipase activity in hepatocytes and I148M leads to loss of function that promotes accumulation of triglycerides in liver cells [29]. Interestingly, a population-based study in Hong Kong found that the PNPLA3 gene polymorphism had a greater effect on liver fat in lean individuals compared to overweight and obese individuals. Furthermore, lean individuals were significantly more likely to carry the risk allele compared with overweight and obese individuals [30]. Therefore, genetic factors may have a greater effect towards the development of NAFLD in lean or non-obese individuals, but the effect may be less pronounced in the presence of strong environmental factors, such as poor dietary choices and a sedentary lifestyle, with increasing BMI and in the obese state (Fig. 1). The findings were somewhat different in a study in the Western population, which found that the effect of the risk allele was amplified by increasing adiposity [31]. The inconsistent findings may be due to other genetic determinants at play, environmental factors such as diet, or differences in the metabolic profile of the study populations. A difference in the effect of genetic polymorphisms in the PNPLA3 gene on NAFLD has been observed among different ethnic groups, with the effect lowest among the Chinese compared to the Indians and Malays [32]. In a subsequent study, the HSD17B13 rs72613567 and rs6834314 variants were found to be associated with a lower risk of NASH and adverse liver-related outcomes among the Chinese but not the Indians and Malays, supporting the role of polygenic determinants in the disease phenotype [33]. The transmembrane 6 superfamily member 2 (TM6SF2) encodes a membrane protein required for normal very low density lipoprotein secretion. The rs58542926 C>T variant, which results in substitution of glutamate by lysine at position 167 (E167K), was found to be associated with higher circulating levels of serum alanine aminotransferase, a marker of liver injury, but lower level of serum low density lipoprotein cholesterol and triglycerides [34]. In a retrospective cohort study on 669 consecutive patients with biopsy-proven NAFLD in Italy, a significantly greater proportion of patients with lean NAFLD had E167K compared to their non-lean counterparts. In the same study, I148M was the only independent factor found to be associated with NASH and significant fibrosis among lean patients [35]. Additionally, lean NAFLD may be also driven by other rare genetic disorder, such as familial hypobetalipoproteinemia and cholesteryl ester storage disease [36,37].
More severe liver disease in some non-obese NAFLD patients
Even among lean or non-obese NAFLD patients, varying proportions of more severe liver disease have been observed. As elucidated earlier, this may be due to the under-reporting of alcohol intake, particularly in populations with high alcohol consumption, as well as genetic factors. For example, in a study on an outpatient population in the United States, ethic differences in the prevalence of cryptogenic cirrhosis mirrored the prevalence of hepatic steatosis and the frequency of I148M among the different ethnic groups [27]. Another point for consideration is the loss of weight from poorly controlled diabetes mellitus and the loss of muscle mass associated with more advanced chronic liver disease in patients with longstanding history of obesity, NAFLD, and diabetes mellitus. The inclusion of these patients as lean or non-obese NAFLD will paradoxically enrich the population with patients who are worse metabolically and have more severe liver disease with resultant poorer outcomes. The gut microbiome may play a role in the pathogenesis of NAFLD [38], but this remains unclear and deserves further studies, especially in non-obese NAFLD.
NON-INVASIVE TESTS IN NON-OBESE NAFLD
It is well-recognized that the fibrosis stage is the single most important predictor for overall and liver-related mortality in patients with NAFLD [39]. The same has been observed for the subpopulation of lean or non-obese NAFLD patients [11]. Due to the high prevalence of NAFLD in the general population and only a small yet significant proportion of patients having advanced liver fibrosis [40], a simple assessment and referral pathway is needed to identify the patients who are more likely to have more severe liver disease for specialist care and to limit unnecessary referrals [41]. Although liver biopsy is considered the reference standard for fibrosis assessment and required for the diagnosis of NASH, it is not routinely performed as it is invasive and associated with a small risk of serious complications. Since the initial description and following refinement and validation, sequential testing with simple fibrosis score followed by liver stiffness measurement has become the backbone for fibrosis assessment in patients with NAFLD [41-44]. In a multicenter study in France, Malaysia, and Hong Kong, all non-invasive tests that were tested, including the Fibrosis-4 index, NAFLD fibrosis score, and liver stiffness measurement, were performed equally well in non-obese compared with obese patients, and the same cut-offs can be used with similar or higher sensitivities and specificities. Furthermore, the negative predictive value of every noninvasive test was found to be higher due to the lower prevalence of advanced fibrosis among non-obese compared to obese patients [45]. A subsequent individual patient data meta-analysis evaluating non-invasive tests against liver histology using data from 5,705 patients (15.2% of patients had a BMI of <25 kg/m2) found that non-invasive tests, namely the Fibrosis-4 index, NAFLD fibrosis score, and liver stiffness measurement, performed better in patients with lower BMI [46]. The area under the curve of some of the most commonly used non-invasive tests among non-obese patients compared to obese patients are summarized in Table 2.
LIFESTYLE INTERVENTION AND PHARMACOLOGICAL TREATMENT IN NON-OBESE NAFLD
Lifestyle intervention is the cornerstone for the management of NAFLD. A landmark study on comprehensive lifestyle programs for patients with biopsy-proven NASH has shown that weight loss of ≥10% can result in NASH resolution and fibrosis improvement in 90% and 45%, respectively [47]. In a randomized controlled trial of a 12-month lifestyle intervention program, a significantly greater proportion of patients in the intervention group achieved remission of NAFLD based on proton-magnetic resonance spectroscopy compared with the control group (64% vs. 20%, P<0.001) with 97% of patients with ≥10% weight loss achieving remission of NAFLD [48]. More importantly, a secondary analysis found similar beneficial effect of lifestyle intervention program regardless of the baseline BMI. The proportion of patients achieving remission of NALFD was 67% in the intervention group and 18% in the control group among non-obese patients. The corresponding proportions among obese patients were 61% and 21%, respectively. Furthermore, 50% of non-obese patients achieved remission of NAFLD with 3–5% weight loss, while the same could be also achieved with 7–10% weight loss among obese patients [49].
To date, there is no pharmacological therapy approved for NAFLD. However, multiple drugs targeting obesity and the metabolic syndrome have shown promising results. In a multicenter, randomized, double-blind, placebo-controlled trial on biopsy-proven NASH patients, liraglutide 1.8 mg daily for 48 weeks resulted in significantly greater resolution of definite NASH compared to placebo [50]. In another study, semaglutide at increasing dosages resulted in significantly greater NASH resolution without worsening fibrosis compared with placebo, but there was no significant difference in fibrosis improvement [51]. However, these studies enrolled only overweight patients with BMI ≥25 kg/m2 [50,51]. Whether glucagon-like peptide-1 receptor agonists will be beneficial over standard of care and have acceptable profiles of side effect in lean NAFLD patients is not clear. Another concern related to marked weight loss, although desirable for the underlying NAFLD, is whether it comes with an associated loss of muscle mass. Sarcopenia is a common and important complication of chronic liver disease, including NAFLD, and has been associated with poorer outcomes [52]. However, post-hoc analysis of the STEP 1 trial, which was a trial evaluating semaglutide 2.4 mg once-weekly for adult patients with BMI ≥27 kg/m2 with ≥1 weight-related comorbidity or BMI ≥30 kg/m2, without diabetes mellitus, found semaglutide to be associated with reduced total fat mass and regional visceral fat mass, and an increased proportion of lean body mass. Although the total lean body mass decreased from baseline (–9.7%), the proportion relative to total body mass increased by 3.0% with improvement in lean body mass to fat mass ratio [53]. Another study found that semaglutide resulted in significant declines in fat mass index and visceral adipose tissue, but not skeletal mass index, fat free mass index, and muscle strength [54]. However, further studies are needed on the use of these emerging novel therapies in lean or non-obese NAFLD patients [55].
CONCLUSION
Lean or non-obese NAFLD is a common entity and may be more than just the early phase or the less severe end of the NAFLD spectrum. While confounding factors, such as alcohol intake and weight loss following disease progression, could explain more severe liver disease and a worse outcome in some patients with lean or non-obese NAFLD, genetic factors are increasingly recognized to play an important role. Further studies to understand these genetic determinants in lean or non-obese NAFLD patients may open the door to better diagnostics and therapeutics that may have the potential to be expanded to obese NAFLD patients. Overall, non-invasive tests perform better in lean or non-obese NAFLD patients than in their obese counterparts. Lifestyle intervention works for lean or non-obese NAFLD patients, and less amount of weight loss may be required to achieve similar results compared to obese NAFLD patients. The role of emerging therapeutics in lean or non-obese NAFLD patients is unclear, and further studies are warranted.
Notes
Conflicts of Interest
Wah-Kheong Chan has served as a consultant or advisory board member for Roche, Abbvie, Boehringer Ingelheim and Novo Nordisk; and a speaker for Viatris and Hisky Medical.
Abbreviations
NAFLD
nonalcoholic fatty liver disease
MAFLD
metabolic dysfunction-associated fatty liver disease
BMI
body mass index
NASH
nonalcoholic steatohepatitis
PNPLA3
patatin-like phospholipase domain-containing-3
TM6SF2
transmembrane 6 superfamily member 2
E167K
glutamate by lysine at position 167