Continuing besifovir dipivoxil maleate versus switching from tenofovir disoproxil fumarate for treatment of chronic hepatitis B: Results of 192-week phase 3 trial
Article information
Abstract
Background/Aims
Besifovir dipivoxil maleate (BSV), an acyclic nucleotide phosphonate, shows potent antiviral activity against hepatitis B virus. Our previous 48-week trial revealed that BSV has comparable antiviral efficacy to tenofovir disoproxil fumarate (TDF) and better safety profiles in terms of improved renal and bone safety. This extension study evaluated the prolonged efficacy and safety of BSV in treatment-naive chronic hepatitis B patients.
Methods
Patients continued to participate in an open-label BSV study after an initial 48-week double-blind comparison of BSV and TDF treatment. The antiviral efficacy and drug safety was evaluated up to 192 weeks in two groups: patients continuing BSV treatment (BSV-BSV) and patients switching from TDF to BSV after 48 weeks (TDF-BSV).
Results
Among 197 patients receiving randomized treatments, 170 (86%) entered the open-label phase and 152 (77%) entered the 192-week extension study. Virological response rates over 192 weeks were 92.50% and 93.06% in the BSV-BSV and TDF-BSV groups, respectively (P=0.90). Hepatitis B envelop antigen seroconversion and alanine aminotransferase normalization rates were similar between the groups (P=0.75 and P=0.36, respectively). There were no drug-resistant mutations to BSV. Bone mineral density and renal function were well preserved in the BSV-BSV group, whereas these initially worsened then recovered after switching therapy in the TDF-BSV group.
Conclusions
BSV maintained potent antiviral efficacy after 192 weeks and showed no evidence of drug resistance. BSV was safe, well tolerated, and effective in patients who switched from TDF to BSV. Trial Registration Number: NCT01937806 (date: 10 Sep 2013).
Graphical Abstract
INTRODUCTION
Hepatitis B is a major global health concern with 350 million people suffering from chronic hepatitis B (CHB) and 600,000 deaths per year due to related diseases [1]. Suppression of hepatitis B virus (HBV) replication by nucleos(t)ide analogs (NAs) leads to decreased liver-related events such as hepatocellular carcinoma (HCC) and decompensation [2]. However, functional cure by antiviral therapy (AVT), which is defined as sustained loss of hepatitis B surface antigen (HBsAg) is uncommon [3] and HBV relapse frequently occurs after cessation of AVT [4]. Therefore, most CHB patients are required to continue long-term AVT [5]. Because long-term AVT increases the risk of drug resistance, current guidelines recommend drugs with a high genetic resistance barrier as first-line treatment [6-8].
Tenofovir disoproxil fumarate (TDF) has potent antiviral effects and very high genetic barriers against resistance [9]. TDF monotherapy was shown to be effective in lamivudine-resistant and adefovir-resistant patients [10]. Thus, TDF is recommended as a first-line therapy as well as a rescue therapy for patients suffering from lamivudine and/or adefovir resistance [7]. However, long-term TDF therapy is associated with a potential risk of renal complications such as acute kidney injury or Fanconi syndrome as well as bone complications such as osteopenia or osteoporosis [11]. Hence, the European guidelines recommend NAs such as entecavir (ETV) and tenofovir alafenamide fumarate (TAF) rather than TDF for patients with bone or kidney diseases [6].
Besifovir dipivoxil maleate (BSV), an acyclic nucleotide phosphate, has potent antiviral efficacy and was approved for the treatment of CHB patients in Korea in May 2017 following the results of a 48-week randomized, controlled, phase 3 trial (NCT01937806). The results revealed that BSV and TDF showed similar antiviral efficacy at 48 weeks [12]. Furthermore, BSV treatment had a good safety profile, in addition to its potent antiviral effect, in terms of renal function and bone mineral density (BMD) until 144 weeks [13]. In the present study, subsequent extended studies were carried out to study the antiviral efficacy and safety of long-term BSV treatment over 192 weeks.
MATERIALS AND METHODS
Study design
This was a 192-week study, including 48 weeks of randomized controlled trial, with an extension period for the treatment of hepatitis B patients in Korea. The initial 48-week period comprised a double-blind, randomized, multi-center, non-inferiority, controlled trial comparing BSV (Ildong Pharmaceutical Co, Ltd., Seoul, Korea) with TDF (Gilead Sciences, Foster City, CA, USA), and the remaining 144 weeks comprised an open-label trial with BSV administration only. The present study was conducted in 22 institutions and obtained approval from each institution’s Institutional Review Board and the Human Research Ethics Committee. Further details are described elsewhere [12]. Signed consent was provided by all participants, and the study protocol followed the ethical guidelines of the Declaration of Helsinki.
Study participants
CHB patients were enrolled from November 2013 to February 2016 (NCT01937806). Details of the eligibility criteria are described in our previous study [12]. The main inclusion criteria were CHB patients aged ≥20 years and not having received AVT (treatment naive), such as interferon (including peg-interferons), for ≥12 weeks. Antiviral treatment was initiated in patients with HBV DNA levels >1.0×105 copies/mL (17,241 IU/mL) for hepatitis B envelop antigen (HBeAg)-positive patients and >1.0×104 copies/mL (1,724 IU/mL) for HBeAg-negative patients. Patients were also required to have serum alanine aminotransferase (ALT) levels of 1.2–10 times that of the upper limit of normal (ULN) (central laboratory cutoff of 33 U/L for females and 41 U/L for males). Patients with HCC, coinfected with hepatitis C virus, hepatitis D virus, or human immunodeficiency virus, and with decompensation were excluded. After the first 48 weeks, patients who agreed and gave written informed consent for the open-label phase participated in the extensional study.
Treatment
Participants were randomly assigned to two groups in a 1:1 ratio and received either BSV (150 mg) plus L-carnitine (660 mg) or TDF (300 mg) alone for initial 48 weeks. In this period, to ensure double-blinding, participants in the BSV plus L-carnitine group also received placebo TDF, whereas those in the TDF group received placebo BSV plus placebo L-carnitine supplements. Thereafter, in the extension study, participants who had received BSV plus L-carnitine in the initial phase were administered the same regimen and those who had received TDF were switched to BSV plus L-carnitine, and the treatment was continued until week 192.
Endpoints
The primary endpoint was virological response (VR), defined as HBV DNA <69 IU/mL at week 192. Other efficacy endpoints were HBV DNA <20 IU/mL, HBsAg or HBeAg seroconversion, ALT normalization, and drug resistance. Safety evaluation included monitoring of adverse events (AEs), glomerular filtration rate (GFR), BMD, and carnitine concentration.
Laboratory measurements
All laboratory tests, including hematological analysis, serum chemistry tests, lipid parameters, and renal function measurements, were performed at a central laboratory (GC laboratory, Yongin, Korea) at 12-week intervals. HBV DNA quantification was performed using the COBAS AmpliPrep/TaqMan test (Roche Diagnostics, Indianapolis, IN, USA), with 20 IU/mL as the lower level detection limit. Other laboratory tests were performed as previously described [12].
BMD and GFR
BMD measurements of the lumbar spine (L1–4) and the total hip were performed using dual-energy X-ray absorptiometry scan and conducted at each institution. GFR was calculated using the Modification of Diet in Renal Disease (MDRD) method using the formula: 175 × serum creatinine (mg/dL) – 1.154 × age (years) – 0.203 (× 0.742 for females). BMD and GFR measurements were performed at baseline and weeks 48, 96, 144, and 192.
Resistance surveillance
Population sequencing was performed in all participants at baseline and at weeks 48, 96, 144, and 192 in participants with HBV DNA levels >1,724 IU/mL. DNA sequencing was performed at the investigator’s discretion to confirm drug adherence if virological breakthrough (increase of >1 log10 IU/mL from HBV DNA nadir) developed. An in vitro drug susceptibility assay was performed at the central laboratory (Department of Pharmacology and Center for Cancer Research and Diagnostic Medicine, IBST, School of Medicine, Konkuk University, Seoul, Korea) when virological breakthrough was observed from two continuous visits and when changes were detected in the reverse transcriptase sequence [14,15].
Construction of HBV RT mutant replicons
HBV DNA was extracted from the sera of the patients using a QiAamp MinElute Virus Spin Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocol. To characterize the HBV RT gene, the RT gene was amplified by PCR and cloned into the HBV1.2mer replicon using the pGEM-4Z vector (Promega, Madison, WI, USA) and sequenced, as described previously [15]. To identify the mutation(s), the sequences were compared with a wildtype genotype C HBV genome (NCBI GenBank accession no. GQ872210) isolated from the serum of an HBeAg-positive asymptomatic CHB patient (Supplementary Table 1).
In vitro drug susceptibility assay
In vitro drug susceptibility assay was performed as reported previously [15]. Briefly, Huh7 cells maintained in Dulbecco’s modified Eagle’s medium (Welgene, Gyeongsan, Korea) and supplemented with 10% fetal bovine serum were seeded into six-well plates and transfected with 2 μg of each replicon. After 4 hours, this medium was replaced with a fresh medium containing different concentrations (0, 5, 10, 20, 50 μg) of BSV. After drug treatment for 4 days, the supernatants and cells were harvested for HBeAg ELISA and Southern blot analysis, respectively. In vitro drug susceptibility data are representative of at least three independent experiments.
Statistical analyses
The primary efficacy endpoints, study designs, and sample size estimates were performed as described previously [12]. Briefly, for the primary efficacy analysis, the proportion of patients with HBV DNA <69 IU/mL was performed using the full analysis set (FAS) and per protocol set (PPS). Differences in baseline characteristics and endpoints between the treatment groups were analyzed using independent two-sample t test or Wilcoxon’s rank-sum test for continuous variables and a chi-squared test or Fisher’s exact test for categorical variables. P-value of <0.05 was defined as statistically significant. All analyses were performed using Statistical Analysis System 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Study population
Among 197 participants (86%) who enrolled in the initial randomized study, 170 participated in the BSV monotherapy extension study. Of these patients, 152 participated in the extended treatment period III (144–192 weeks, 4 years) and two (1.32%) dropped out owing to non-adherence (one in BSV-BSV and one in TDF-BSV group) (Fig. 1). A total of 152 participants (80 in the BSV-BSV group and 72 in the TDF-BSV group) were included in the FAS. Among these, 144 (77 in the BSV-BSV group and 67 in the TDF-BSV group) were included in the PPS, excluding eight cases of dropout or impaired compliance, for the 192-week analysis.
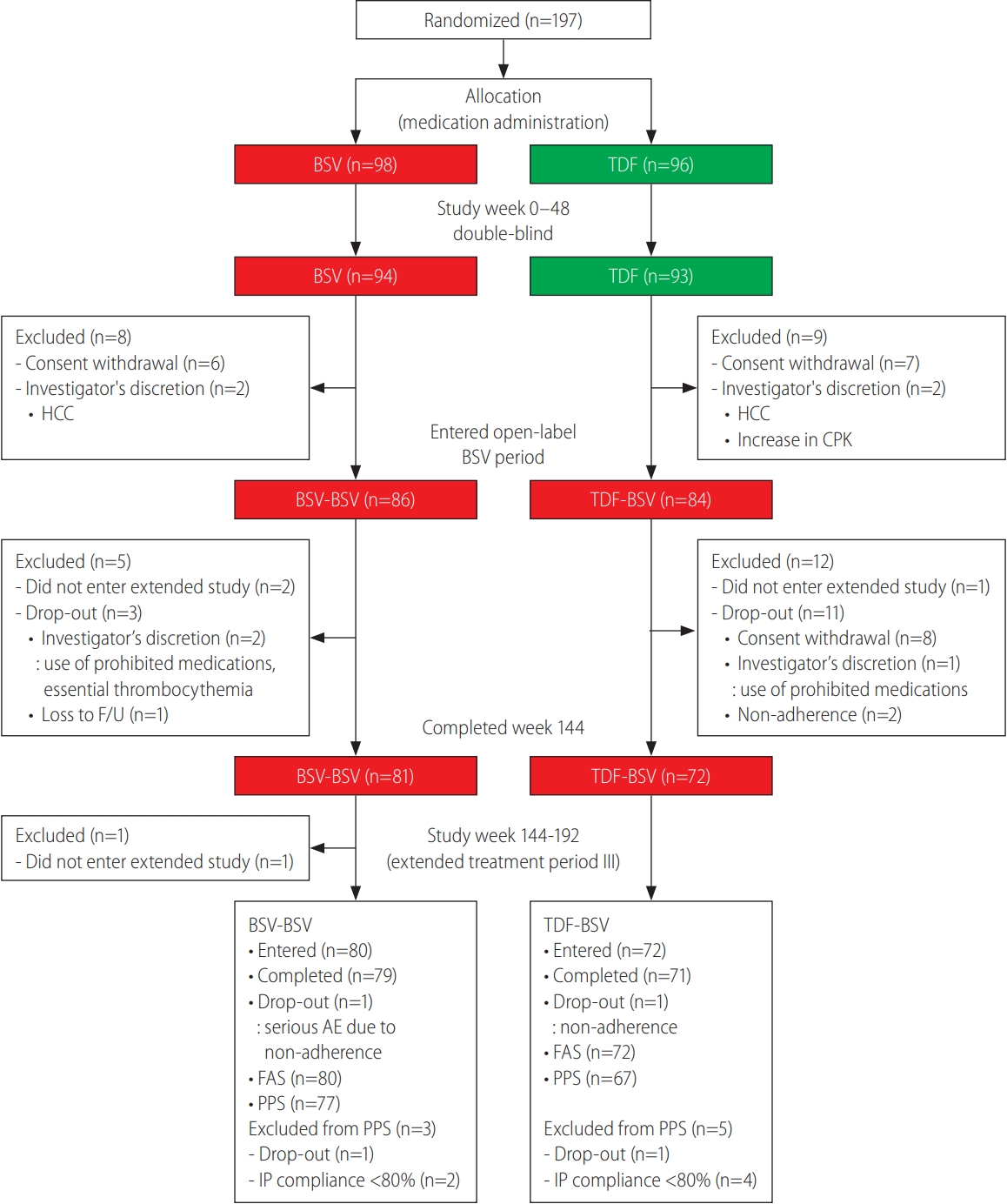
Patient disposition. BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate; HCC, hepatocellular carcinoma; CPK, creatinine phosphokinase; F/U, follow up; FAS, full analysis set; PPS, per protocol set; IP, investigational product.
Among the total study population, 65.1% (99/152) were male, and the rate of HBeAg-positive patients was 62.5% in the BSV–BSV group and 55.6% in the TDF-BSV group. The most common HBV genotype was type C (98.0%). The baseline characteristics were similar between the two groups, with an average HBV DNA of 6.31 log10 IU/mL and 6.55 log10 IU/mL in the BSV-BSV and TDF-BSV groups, respectively (Table 1).
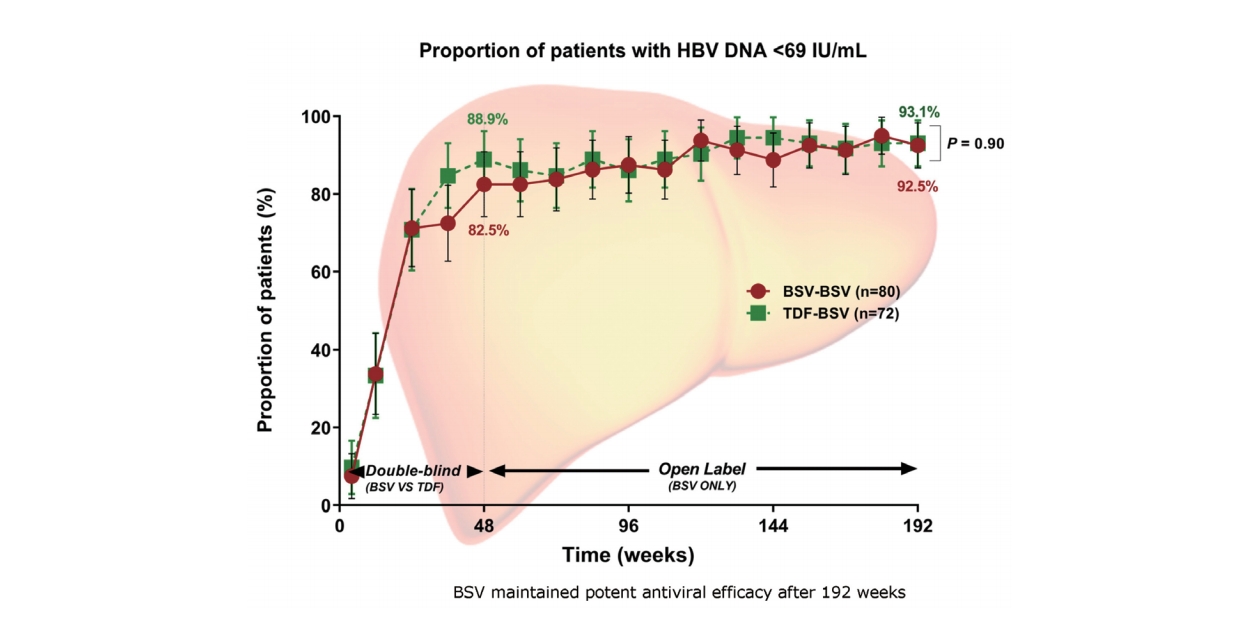
Virological response
At week 192, the cumulative incidence rates of HBV DNA <69 IU/mL and <20 IU/mL were 92.5% and 87.5% in the BSVBSV group and 93.1% and 87.5% in the TDF-BSV group, respectively, and there was no significant difference between the two groups in terms of VR in the FAS (P=0.90 for HBV DNA <69 IU/mL and P=1.00 for HBV DNA <20 IU/mL). The PPS analysis result was similar to the FAS result, and revealed that the HBV DNA <69 IU/mL and <20 IU/mL rates were 94.8% and 89.6% in the BSV-BSV group and 94.0% and 88.1% in the TDF-BSV group (Table 2), respectively. The antiviral responses during the follow-up period of 192 weeks were similar between the two groups (Fig. 2), and there were no significant differences in antiviral response between the two groups regardless of cirrhosis (Supplementary Table 2). In both the BSV and the TDF groups, the mean HBV DNA levels decreased rapidly by week 24, and HBV DNA suppression was maintained throughout the 192 weeks, even if TDF was converted to BSV (Supplementary Fig. 1A). Changes in HBV DNA levels at week 192 did not significantly differ between the groups (-4.88±1.71 log10 IU/mL in the BSV-BSV group and -5.14±1.43 log10 IU/mL in the TDF-BSV group, P=0.32) (Supplementary Fig. 1B).
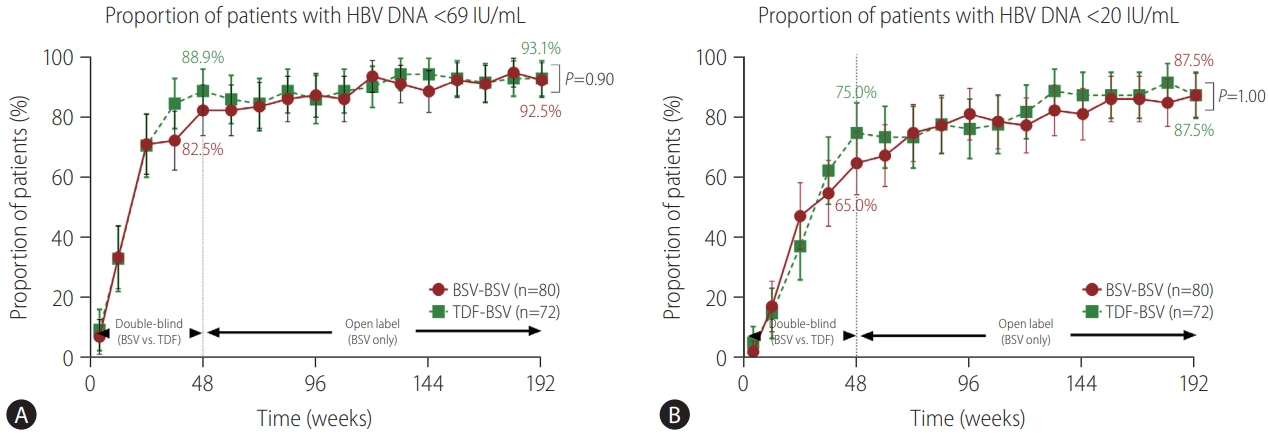
Viral suppression by study visit. (A) Proportions of patients with HBV DNA <69 IU/mL as determined by FAS. (B) Proportions of patients with HBV DNA <20 IU/mL as determined by FAS. Bars represent 95% confidence intervals. HBV, hepatitis B virus; BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate; FAS, full analysis set.
Serological and biochemical responses
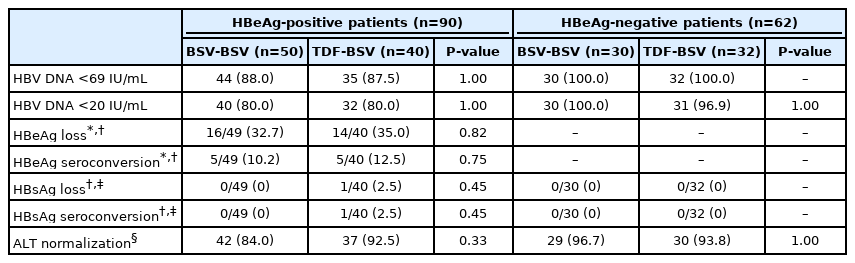
At week 192, the rates of HBeAg loss and HBeAg seroconversion were 32.7% and 10.2%, respectively, in the BSV-BSV group and 35.0% and 12.5%, respectively, in the TDF-BSV group. These rates did not differ statistically between the two groups (P=0.82 and P=0.75).
None of the participants in the BSV-BSV group showed HBsAg loss and/or seroconversion until week 192, whereas one participant in the TDF-BSV group showed HBsAg loss at week 48 and seroconversion at week 144 (Table 2).
At week 192, 88.8% of participants in the BSV-BSV group and 93.1% of participants in the TDF-BSV group showed serum ALT normalization (P=0.36) (Table 2, Supplementary Fig. 2). ALT normalization rates were similar between the two groups regardless of cirrhosis (Supplementary Table 2).
Resistance surveillance and virological breakthrough
It was previously shown that resistance to BSV did not develop until 144 weeks [13]. One patient, who was not adherent to medication and finally dropped out, experienced virological breakthrough between weeks 144 and 168. In this patient (#136=S07-09), a BSV susceptibility test was performed (Supplementary Fig. 3A). As a result, although some mutations (reverse transcriptase region mutations 55, 134, 267, 269, and 305) were found in HBV DNAs cloned in the patient (Supplementary Table 1), the sequence changes were present at baseline and the patient’s HBV DNAs were phenotypically sensitive to inhibition by BSV in vitro (Supplementary Fig. 3B). Therefore, we believed that the virological breakthrough in this patient was caused by non-adherence and finally concluded that resistance to BSV was not developed until 192 weeks.
Subgroup analyses
The virological, serological, and biochemical responses were further evaluated according to HBeAg status (Table 3). At 192 weeks, all HBeAg-negative patients achieved HBV DNA <69 IU/mL, and only one patient in the TDF-BSV group failed to achieve HBV DNA <20 IU/mL. In HBeAg-positive patients, 88.0% (44/50) of the BSV-BSV group and 87.5% (35/40) of the TDF-BSV group achieved HBV DNA <69 IU/mL (P=1.00), (Supplementary Fig. 4), and the rates for those achieving HBV DNA <20 IU/mL were 80.0% (40/50) and 80.0% (32/40) in the BSV-BSV and TDF-BSV groups, respectively (P=1.00) (Supplementary Fig. 5). HBsAg loss or seroconversion to HBsAb developed in only one HBeAg-positive patient in the TDF-BSV group and there was no significant difference between the BSV-BSV and TDF-BSV groups (P=0.45). The BSV-BSV and TDF-BSV groups showed similar ALT normalization rates among both the HBeAg-positive and HBeAg-negative subgroups (P=0.33 and P=1.00, respectively) (Table 3). PPS analysis of both subgroups showed similar results to the FAS analysis (Supplementary Table 3).
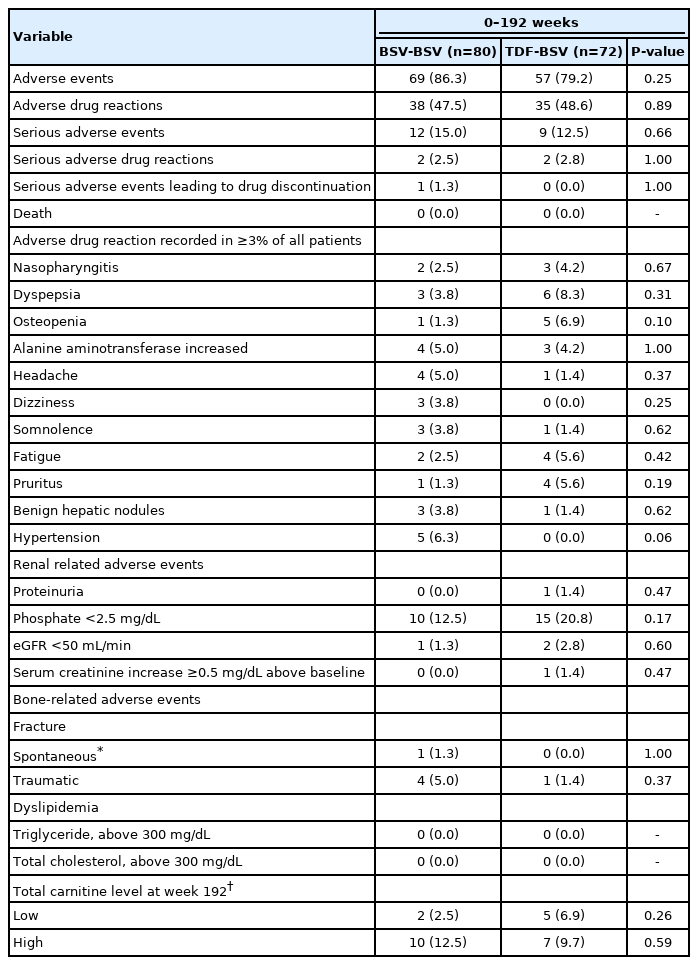
Safety
During 192 weeks, 69/80 (86.3%) AEs were reported in the BSV-BSV group and 57/72 (79.2%) were reported in the TDF-BSV group. During this period, there were 12/80 (15.0%) SAEs reported in the BSV-BSV group and 9/72 (12.5%) in the TDF-BSV group (Table 4, Supplementary Table 4).
Among the reported SAEs, serious adverse drug reactions (SADRs) included one case each of muscle spasm and biochemical breakthrough due to non-adherence in the BSV-BSV group and one case each of sudden hearing loss and arthralgia in the TDF-BSV group. All patients who had experienced SADR recovered, but the one with biochemical breakthrough finally dropped out (Table 4, Supplementary Table 4).
Hip and spine BMD decreased during the 48 weeks in the TDF group (mean percent change: -0.62 vs. 0.28, P=0.01 in hip and -1.12 vs. 0.39, P=0.07 in spine), whereas there was no change in the BSV group. However, in the TDF group, hip and spine BMD improved after switching to BSV at 48 weeks, and there was no significant difference from the BSV-BSV group after at 96 weeks. Furthermore, hip and spine BMD was maintained in both groups until 192 weeks and showed no significant difference in mean percent change compared with baseline (0.69 vs. -0.62, P=0.46 in hip BMD and -0.39 vs. -1.02, P=0.82 in spine BMD) (Fig. 3).
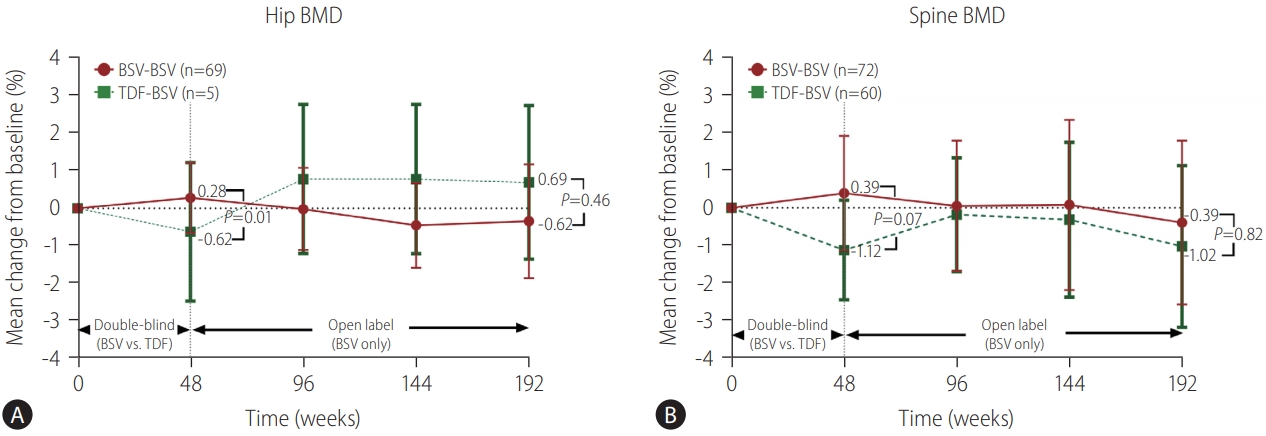
Changes in BMD. (A) Mean percentage changes in the hip at week 48, 96, 144, and 192 of treatment. Bars represent 95% confidence intervals. (B) Mean percentage changes in the spine at week 48, 96, 144, and 192 of treatment. Bars represent 95% confidence intervals. BMD, bone mineral density; BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate.
The median changes in GFR at 192 weeks were 6.0 mL/min (interquartile range [IQR]: -1.60, 12.90) and 0 (IQR: -2.30, 15.25) in the BSV-BSV and TDF-BSV groups, respectively (P=0.59) (Fig. 4). Reduction in GFR to <50 mL/min at week 192 was not observed in the BSV-BSV group and was seen in one patient (1.4%) in the TDF-BSV group during the extension study III period (144–192 weeks). This patient had underlying diabetes mellitus, which led to a reduction in renal function, and the GFR decreased to <50 mL/min from week 96 and continued to week 192. Another patient in the TDF-BSV group had proteinuria at week 192, but reduced GFR or other AEs related to renal function were not observed in this patient.
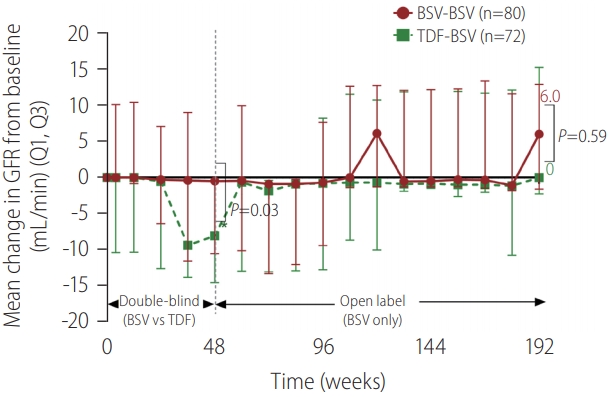
Median changes from baseline in eGFR (MDRD) by study week. Data are presented as median (Q1, Q3) values (mL/min). BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate; eGFR, estimated glomerular filtration rate; MDRD, modification of diet in renal disease.
A decrease in L-carnitine levels was observed in seven patients (two patients in the BSV-BSV group and five patients in the TDF-BSV group) at week 192 without any clinical symptoms associated with carnitine deficiency. During the next visit, we will check the safety in patients with decreased levels of L-carnitine using follow-up laboratory tests.
DISCUSSION
The present study reports the four-year outcome of a study scheduled for eight years in HBeAg-positive and HBeAg-negative CHB patients. Long-term BSV treatment showed a stable and potent virological, biochemical, and serologic response. In addition, no viral resistance against BSV was found during the 4 years. BSV therapy was tolerable, none of the patients discontinued its use due to AEs, and the risk of BSV-induced renal and bone complications were low.
Our previous study revealed that BSV has antiviral effects comparable to those of TDF during 48 weeks. Furthermore, the antiviral effect was maintained for up to 144 weeks when TDF was switched to BSV [12,13]. The present study showed that BSV treatment increased the VR rate (HBV DNA <69 IU/mL and 20 IU/mL) to approximately 90% at 192 weeks. Previous studies on the long-term effects of TDF or ETV have shown that around 90% of patients had HBV DNA suppression for four years [16,17]. Therefore, although BSV treatment was not directly compared with ETV or TDF at 4 years, BSV is also considered to have potent antiviral efficacy similar to TDF and ETV, which have been shown to have long-term antiviral effects. In addition, the biochemical response rate was also maintained until 192 weeks. Since HBV DNA and ALT levels are risk factors for liver-related events [18], efficacious HBV DNA suppression and ALT normalization by BSV is expected to prevent progress to decompensated cirrhosis and reduce the development of HCC.
In this study, HBeAg loss and seroconversion rate were lower than those in other studies for patients receiving NA [19,20]. In HBeAg-positive patients, low viral load and high serum ALT levels are the pre-treatment predictive factors of HBeAg seroconversion [21,22]. Most guidelines recommend AVT in HBeAg-positive CHB patients with ALT ≥2×ULN [6,7,23]. However, this study included CHB patients with ALT levels of 1.2–10 times that of the ULN, and ALT levels was lower than those observed in other studies. Therefore, lower ALT levels may lead to lower HBeAg loss and seroconversion rate in this study.
Emergence of resistance to NAs is related to reduced antiviral efficacy, hepatitis flares, disease progression, and poor outcomes [24,25]. Therefore, it is recommended that NAs with high resistance barrier are used as the first-line therapy [6-8]. The present study showed that the VR was maintained without resistance up to 4 years (192 weeks) during BSV administration. Therefore, BSV may also be regarded as a high genetic barrier drug and can be considered for first-line treatment as well as ETV and TDF. Due to the high genetic barrier, TDF monotherapy is also used as rescue therapy in CHB patients with resistance to other NAs, such as lamivudine or adefovir, even with multidrug resistance [26]. A study on the antiviral efficacy of BSV in patients with NAs resistance is currently underway (NCT02792088).
Despite its potent antiviral efficacy and low resistance, reduction in BMD due to long-term use of TDF is an important problem. A previous study revealed that the incidence rates of osteoporosis and osteopenia were 8.2% and 31.6%, respectively, after 96 weeks of TDF [27], and TDF was also shown to be an independent predictor of low BMD [28]. In the present study, use of TDF for 48 weeks decreased BMD, whereas there was no change in BMD in the BSV group. Interestingly, switching from TDF to BSV improved hip and spine BMD to a similar degree to that observed in the BSV-BSV group, and BMD was maintained up to 192 weeks without showing a significant change. In addition, although bone fracture events seemed to be more frequent in the BSV-BSV group, most fractures (four in the BSV-BSV and one in the TDF-BSV) occurred by either trauma or accident, and only one fracture event in the BSV-BSV group occurred in a patient with osteoporosis. Furthermore, there were no significant differences in BMD changes between those with fractures and those without fractures (P=0.34, data not shown). Therefore, BSV can be used without concern about BMD reduction in individuals at high risk of osteoporosis, such as patients with osteopenia, elderly patients, or menopausal women.
TDF has potential nephrotoxic effects such as decreased GFR or tubular injury [29,30]. In the present study, the TDF group showed a significant decline in GFR during the 48 weeks, whereas there was little change in the BSV group. After switching from TDF to BSV, the GFR recovered to the same level as that of the BSV-BSV group, and there was no difference until 192 weeks. One patient in the TDF-BSV group was observed to have and estimated GFR (eGFR) <50 mL/min; however, this patient had diabetes, which is a risk factor for renal disease, as an underlying disease. In addition, another patient had intermittent proteinuria since the beginning of the study, and no abnormal findings were observed by the nephrology or urology consultants. Therefore, BSV was not associated with renal complication in the present study, and BSV can be safely used in patients with reduced renal function without impairing renal function.
Carnitine deficiency is the most common side effect of BSV [31,32]. Therefore, L-carnitine (660 mg/day) was supplemented during BSV treatment. A reduction in serum carnitine levels was observed in two patients in the BSV-BSV group and five patients in the TDF-BSV group at week 192. Serum carnitine levels were close to the lower normal limit, and there were no clinical symptoms associated with carnitine deficiency, such as hypoglycemia, hypoketosis, or encephalopathy, in these patients. However, the effects of a slight reduction in serum carnitine concentration by BSV require long-term follow-up.
TAF, which is an orally bioavailable prodrug of tenofovir, has been developed to reduce AEs of TDF, such as renal or bone complications. In a TDF-TAF switching study, changes in GFR and BMD showed a similar pattern to those seen with switching from TDF to BSV [33]. Recent studies have reported that TAF may worsen lipid profiles, with a 1–4% of grade 3–4 hypercholesterolemia [34-38]. In contrast, there was only a small change in total cholesterol level at week 48 and 192 with BSV compared with baseline (+3.74 mg/dL, P=0.222 and -2.47 mg/dL, P=0.420, respectively), and there was no severe dyslipidemia at 192 weeks. Moreover, only small changes in serum triglyceride levels were observed at weeks 48 and 192 (7.13 mg/dL, P=0.222 and 3.24 mg/dL, P=0.196, respectively), suggesting that BSV is a safe for use in patients with dyslipidemia.
The present study has several limitations. First, the sample size was relatively small and only Asian patients were enrolled. Therefore, further studies with large sample sizes and race diversity are required. Second, although 4-year BSV treatment was effective and tolerable, further studies are required to confirm its long-term antiviral efficacy and safety. Third, although renal AE was not observed after BSV treatment, the present study did not measure biomarkers for renal function, such as urinary albumin, fractional excretion of uric acid, and urinary beta-2 microglobulin. Similarly, markers for bone turnover to detect bone formation or resorption were not evaluated. Fourth, while levels of total cholesterol and triglyceride were measured every 48 weeks, other lipid profiles, such as low-density lipoprotein cholesterol or high-density lipoprotein cholesterol, were not evaluated. Finally, only qualitative HBsAg was measured; therefore, the present study could not assess the reducing effect of antiviral medication on HBsAg titers, which might represent their impact on intrahepatic covalently closed circular HBV DNA. Despite these limitations, to the best of our knowledge, this is the first study to report on the safety profiles of renal function and bone density in long-term BSV therapy.
In conclusion, BSV treatment for 192 weeks showed potent viral reduction without the development of drug resistance. BSV treatment also demonstrated favorable safety profiles without reducing BMD and eGFR. As the safety profile is a major consideration in the selection of medication, BSV is a potentially novel treatment for CHB, especially in patients at high risk of developing renal and bone-related diseases.
Notes
Authors’ contribution
D.S.S. wrote the manuscript and performed the formal analysis and critical revision. S.H.U. was involved in the study conception, design, and supervision. All the other authors contributed to data acquisition and revision of the manuscript.
Conflicts of Interest: The authors have no conflicts of interest to declare regarding the content of this manuscript. The sponsor paid for the laboratory analyses and clinical research coordinator expenses and supplied the investigational products. Dr. Um received grants for clinical trials sponsored by Ildong Pharmaceutical Co. outside of the submitted work.
Acknowledgements
This study was financially supported by Ildong Pharmaceutical Co. Ltd., Korea.
Abbreviations
AE
adverse event
ALT
alanine aminotransferase
AVT
antiviral therapy
BMD
bone mineral density
BSV
besifovir dipivoxil maleate
CHB
chronic hepatitis B
eGFR
estimated glomerular filtration rate
ETV
entecavir
FAS
full analysis set
GFR
glomerular filtration rate
HBeAg
hepatitis B envelop antigen
HBsAg
hepatitis B surface antigen
HBV
hepatitis B virus
HCC
hepatocellular carcinoma
IQR
interquartile range
NA
nucleos(t)ide analog
PPS
per protocol set
SADRs
serious adverse drug reactions
TAF
tenofovir alafenamide fumarate
TDF
tenofovir disoproxil fumarate
ULN
upper limit of normal
VR
virological response
SUPPLEMENTAL MATERIAL
Supplementary material is available at Clinical and Molecular Hepatology website (http://www.e-cmh.org).
HBV RT mutations identified in a besifovir-treated patient
Virological, biochemical response according to the presence of cirrhosis (FAS)
Virological, serological, and biochemical responses by baseline HBeAg status (PPS)
Serious adverse events
(A) Mean HBV DNA level (log IU/mL). (B) HBV DNA change from baseline (log IU/mL). BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate; HBV, hepatitis B virus; ANOVA, analysis of variance.
ALT normalization at 192 weeks. ALT, alanine aminotransferase; BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate.
In vitro besifovir susceptibility and determination of IC50 of patient-derived RT mutants using Southern blot. (A) The besifovir susceptibility assay. Each panel shows representative autoradiograms from at least three independent experiments. The levels of secreted HBeAg were determined by ELISA to assess the transfection yield. (B) Determination of IC50 values by Southern blot. The level of HBV replication without drug treatment was set at 100%. The IC50 values were obtained by interpolation of the data from at least three independent experiments. WT, wild type; BSV, besifovir dipivoxil maleate; RT, reverse transcriptase; HBeAg, hepatitis B envelope antigen; ELISA, Enzyme-linked immunosorbent assay; HBV, hepatitis B virus.
Proportion of patients with HBV DNA <69 IU/mL at 192 weeks by FAS in (A) HBeAg-positive patients and (B) HBeAg-negative patients. Bars represent 95% confidence intervals. HBeAg, hepatitis B envelope antigen; HBV, hepatitis B virus; BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate; FAS, full analysis set.
Proportion of patients with HBV DNA <20 IU/mL at 192 weeks by FAS in (A) HBeAg-positive patients and (B) HBeAg-negative patients. Bars represent 95% confidence intervals. HBeAg, hepatitis B envelope antigen; HBV, hepatitis B virus; BSV, besifovir dipivoxil maleate; TDF, tenofovir disoproxil fumarate; FAS, full analysis set.
References
Article information Continued
Notes
Study Highlights
• BSV maintained prolonged potent antiviral efficacy without drug resistance in HBeAg-positive and HBeAg-negative patients throughout 192 weeks of treatment.
• Approximately 93% of patients had HBV DNA <69 IU/mL after 192-week BSV treatment.
• Long-term BSV treatment is tolerable and safe in terms of renal function and BMD.