Development and surveillance of hepatocellular carcinoma in patients with sustained virologic response after antiviral therapy for chronic hepatitis C
Article information
Abstract
Hepatitis C virus (HCV) infection is a major risk factor for liver cirrhosis and hepatocellular carcinoma (HCC), and is a leading cause of liver-related deaths worldwide. Recently available direct-acting antiviral agent is very safe and highly effective (>95% sustained virologic response, SVR) against all genotypes of HCV. Achievement of SVR has been associated with a significant reduction of hepatic decompensation, development of HCC, and liver-related mortality. However, HCC risk is not eliminated even after SVR. The annual incidences of HCC in advanced fibrosis or cirrhosis have been estimated to be up to 2.5–4.5% even in patients with SVR. Therefore, surveillance for HCC is recommended in this high-risk patients. In this review, we will describe the clinical outcomes and the risk of HCC in patients with SVR and suggest who should receive surveillance for HCC.
INTRODUCTION
Hepatitis C virus (HCV) infection is a major risk factor for liver cirrhosis and hepatocellular carcinoma (HCC), and is a leading cause of liver-related deaths worldwide. It is estimated that approximately 130–170 million individuals (2.3% of the world population) are chronically infected with HCV. If the patients were not treated, 10–20% of whom will progress to liver cirrhosis over 20-30 years of infection and HCC develops in 1–5% of patients with liver cirrhosis each year [1].
In patients with chronic hepatitis C (CHC), achievement of a sustained virologic response (SVR) by interferon (IFN) treatment has been associated with a significant reduction of hepatic decompensation, development of HCC, and liver-related mortality [2,3]. Previous studies have shown that hepatic decompensation rarely occurred in patients with SVR (annual incidence <0.1%). In patients with advanced liver fibrosis or cirrhosis, however, even after achieving SVR after IFN treatment, the annual incidence of HCC is reported to be as high as 2.5–4.5% [4,5].
Recently available direct-acting antiviral agent (DAA) is very safe and highly effective (>95% SVR) against all genotypes of HCV. They are applicable to all patients with HCV, including old age, those with decompensated liver disease and end stage renal disease who are unfit to IFN therapy [6-10]. In the era of highly effective and safe DAA for the treatment of CHC patients, identifying high-risk groups of HCC and monitoring them continuously is an important clinical issue.
In this review, we will describe the clinical outcomes and the risk of HCC in patients with SVR and suggest who should receive surveillance for HCC.
OUTCOMES OF PATIENTS WITH SVR AFTER IFN-BASED THERAPY
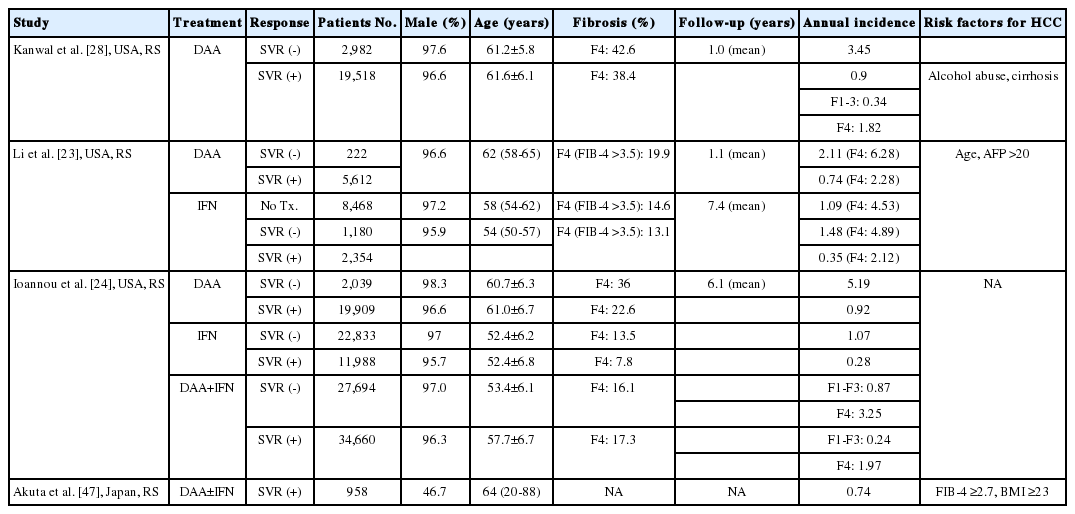
Of the studies that included patients with all stages of fibrosis (Table 1), many studies reported in Japan, Yoshida et al. [11] reported a retrospective analysis of 2,890 patients (2,400 received IFN and 490 untreated) with biopsy-proven CHC. During a mean follow-up of 4.3 years, HCC developed in 89 IFN-treated patients (including 10 patients in SVR) and in 59 untreated patients. The annual incidence of HCC increased with the degree of liver fibrosis in untreated, non SVR and SVR patients (0.45 vs. 0.07 vs. 0.11% in ≤F1, 1.99 vs. 0.78 vs. 0.1% in F2 and 5.34 vs. 2.2 vs.1.29% in F3 and 7.88 vs. 5.32 vs. 0.49% in F4, respectively). In Taiwan, a total of 1,619 patients with biopsy-proven CHC, including 1,057 patients receiving IFN-based therapy and 562 untreated controls were enrolled in retrospective-prospective cohort study and followed for 5.18 years after treatment [5]. The cumulative incidence of HCC was significantly lower in patients with SVR (3.0%) than in those without SVR (36.0%, P=0.007) and untreated patients (35.2%) (P<0.0001). The annual incidence of HCC after SVR was higher in cirrhotic patients compared with non-cirrhotic patients (2.7% vs. 0.09%) [5]. In a prospective study of 642 SVR patients [4], conducted in Taiwan, 33 of the 642 (5.1%) patients developed HCC during median follow-up of 53 months. The annual incidences of HCC were higher in patients with liver cirrhosis compared with non-cirrhotic patients (4.54% vs. 0.14–2.80% depending on additional risk factors). The above results were confirmed in Western countries [12,13]. In a recent large-scale study [13] conducted in Canada, 8,147 patients (cirrhotics in 5%) who received IFN-based therapy were followed for a median of 5.6 years (range: 0.5–12.9). The annual incidences for HCC were 0.11% and 0.72% in patient with SVR and non-SVR, respectively. Among the patients with SVR, cirrhosis, age ≥50 years and male were associated with a higher HCC risk.

Summary of studies reporting annual incidence of hepatocellular carcinoma in all stages of fibrosis patients receiving interferon-based therapy
In a study [14] that included 530 patients with biopsy-proven advanced fibrosis or cirrhosis (Table 2) in Europe and Canada who were treated with IFN-based regimen, HCC developed in 3.6% (7/192) in SVR patients, 22.5% (76/338) in the non-SVR group. Ten-year cumulative incidence rate of HCC was lower in patients with SVR compared without SVR (5.1%; vs. 21.8%; P<0.001). In patients with SVR, the annual incidence of HCC was lower than in those without SVR (0.55%, 95% confidence interval [CI], 0.14–0.96 vs. 2.63%, 95% CI, 1.83–2.89, P<0.001). SVR was associated with reduced risk of all-cause mortality (hazard ratio [HR], 0.26; 95% CI, 0.14–0.49; P<0.001) and reduced risk of liver-related mortality or transplantation (HR, 0.06; 95% CI, 0.02–0.19; P<0.001). van deer Meer et al. [15] also reported the result of pooled data from Western CHC cohort (n=1,000) with bridging fibrosis or cirrhosis who attained SVR. During median follow-up of 5.7 (2.9–8.0) years, HCC and clinical disease progression, defined as liver failure, HCC or death were developed in 51 patients (5.1%) and 101 (10.1%) patients, respectively. The annual incidence of HCC was 0.9% (95% CI, 0.67–1.18). Old age (≥45), low platelet count (<10×109/L) and diabetes mellitus were independently associated with development of HCC.
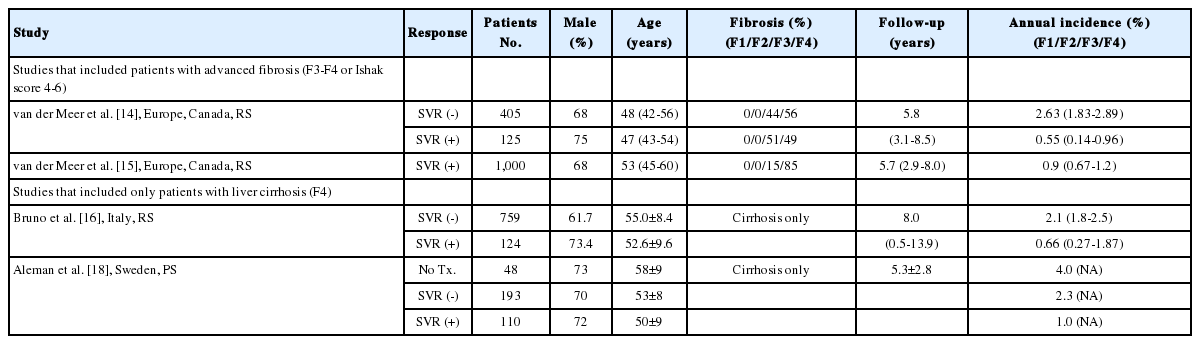
Summary of studies reporting annual incidence of hepatocellular carcinoma in advanced fibrosis or cirrhosis patients receiving interferon-based therapy
In a study [16] that included patients with liver cirrhosis (Table 2), IFN therapy was performed in 1,214 HCV patients. During a mean 8 years of follow up period, HCC developed in 5.6% (7/124) in SVR patients, 16.1% (122/759) in the non-SVR group. Liver-related complications (ascites, upper gastrointestinal bleeding, and hepatic encephalopathy) did not occur in patients with SVR, but in 14.1% (107/759) in non-SVR group. The incidence rates of liver-related complications per 100 person-years of follow-up was 0 in SVR patients and 1.88 (95% CI, 1.54–2.27) in non-SVR patients. The annual incidence rates of liver-related mortality were 0.19 (95% CI, 0.02–0.71) in SVR and 1.44 (95% CI, 0.14–1.78) in non-SVR patients. The clinical benefits of SVR in patient with HCV-related cirrhosis were validated by the prospective studies [17,18]. Shiratori et al. prospectively followed for mean 6.8 years for 271 patients who received IFN treatment with HCV-related cirrhosis [17]. In that cohort, the rates of HCC and liver-related death were lower in SVR patients than in those without SVR (17.2% vs. 35.3%, and 0% vs. 15%, P<0.001). Aleman et al. [18] also conducted a prospective study to evaluate long-term effect of SVR in 351 patients (110 patients with SVR, 193 patients without SVR and 48 patients without treatment) with HCV-related liver cirrhosis. During follow-up for 5.3±2.8 years, HCC developed in six patients after achieving SVR. The annual incidence of HCC was 1.0%. The annual incidence of HCC was significantly higher in non-SVR and untreated patients with 2.3 and 4.0% (P=0.04 and P=0.03, respectively).
Many studies, including meta-analysis, have also demonstrated that the risk of liver-related mortality, and the development of HCC decreases after SVR is attained with IFN-based regimens. A meta-analysis of 26 studies [2], enrolled 15,611 patients, showed that annual incidences of liver-related mortality, HCC and hepatic decompensation were 0.81% (95% CI, 0.55–1.07), 1.84% (95% CI, 1.36–2.32) and 0.54% (95% CI, 0.11–0.97) in patients without SVR in any stage of fibrosis, respectively. Among the non-SVR patients in advanced fibrosis, rates of liver-related mortality (2.73%/year; 95% CI, 1.38–4.08), HCC (3.22%/year, 95% CI, 2.02–4.42), and hepatic decompensation (2.92%/year; 95% CI, 1.61–4.22) were substantial. In another meta-analysis of 12 studies [3], encompassing 25,497 patients, HCC developed in 1.5% (145/9,185) of SVR patients and 6.2% (990/16,312) in non-SVR patients in patient with any stage of fibrosis. The annual incidence of HCC was 0.33% (95% CI, 0.22–0.50) among patients with SVR compared with 1.67% (95% CI, 1.15–2.42) in those without SVR. SVR was associated with reduced risk of HCC of 0.24 (95% CI, 0.18–0.31). In a further meta-analysis of 6 studies including 2,649 patients with advanced fibrosis [3], HCC developed in 4.2% (32/756) and 17.8% (337/1,893) in patients with SVR and without SVR, respectively. The annual incidences of HCC were 1.05% (95% CI, 0.73–1.50) and 3.3% (95% CI, 2.61–4.16) in patients with SVR and without SVR, respectively.
In a recently published prospective study [19], 1,323 patients with biopsy- proven HCV-related liver cirrhosis were followed for median 53 months after IFN-based treatment. SVR was associated with a decreased incidence of HCC (HR, 0.29; 95% CI, 0.19–0.43; P<0.001) and hepatic decompensation (HR, 0.26; 95% CI, 0.17–0.39; P<0.001) compared with patients without an SVR. SVR decreased the overall mortality (HR, 0.27; 95% CI, 018–0.42; P<0.001) compared with patients without SVR and death from liver-related and non-liver-related causes.
OUTCOMES OF PATIENTS WITH SVR AFTER DAA-BASED THERAPY
DAA are very safe and highly effective (>95% SVR) against all genotypes of HCV [8-10]. They are applicable to all patients with HCV, including those with decompensated liver disease and end stage renal disease who are unfit to IFN therapy [6,7]. The introduction of DAA into hepatitis C treatment is expected to increase the clinical benefit in terms of prevention of progression of chronic liver disease and the development of HCC. However, a few recent studies have raised concerns that DAA might increase the risk of HCC in some patients [20-22]. However, recent retrospective studies [23-25] and meta-analyses [26,27] concluded that there is no evidence that HCC occurrence or recurrence after treatment for HCC is different between patients receiving DAA or IFN therapy in patients with SVR treated with DAA or IFN.
Table 3 summarized the outcome of SVR patients who received DAA therapy. In a large retrospective cohort study of HCV patients (n=22,500) treated with DAA using Veterans health administration data, SVR was associated with a 76% reduction in risk of HCC compared with those who did not achieve SVR [28]. Patients with SVR had a significantly reduced risk of HCC compared with patients without SVR (annual incidence 0.90% vs. 3.45%; HR, 0.28, 95% CI, 0.22–0.36). The annual HCC incidences were 0.34% (95% CI, 0.24–0.45) and 1.82% (95% CI, 1.52–2.12) in non-cirrhotic patients and cirrhotic SVR patients, respectively. Even though the follow-up duration was short, the preventive effect of SVR increased over time. Li et al. [23] retrospectively analyzed 17,836 patients treated with IFN or DAA. Among all treated patients, risk of HCC was not higher in the DAA group compared to the IFN group. Among cirrhotic patients (defined by FIB-4 >3.5) with SVR, annual incidence of HCC was not different in the DAA group compared to the IFN group (2.12% vs. 2.28%). In cirrhotic patients with SVR, old age, use of proton-pump inhibitor, and AFP (>20) were independent risk factors for HCC. Ioannou et al. [24] analyzed 62,354 who were treated with IFN only (n=35,871), DAA+IFN (n=4,535) and DAA only (n=21,948). In all regimen, the annual incidences of HCC was 0.43% and 1.14% in SVR and non-SVR patients, respectively. They are not different among three treatment regimen. In cirrhotic patients, the annual incidence was lower in SVR patients compared to those without SVR (1.97% vs. 3.25%). In non-cirrhotic patients, the annual incidence was lower in SVR patients compared to those without SVR (0.24% vs. 0.87%). In patients with DAA, HCC incidence was 0.92% in the SVR group and 5.19% in the non-SVR group.
RISK FACTORS FOR HCC IN CHC PATIENT WITH SVR AFTER ANTIVI RAL THERAPY
Table 4 summarizes the risk factors for HCC in patients with CHC who achieved SVR after antiviral treatment. Among them, old age and ≥F3/F4 fibrosis were most important risk factors for HCC in most studies. Other risk factors for HCC include male, diabetes mellitus, alcohol abuse, high gamma-glutamyltransferase (GGT) and AFP.
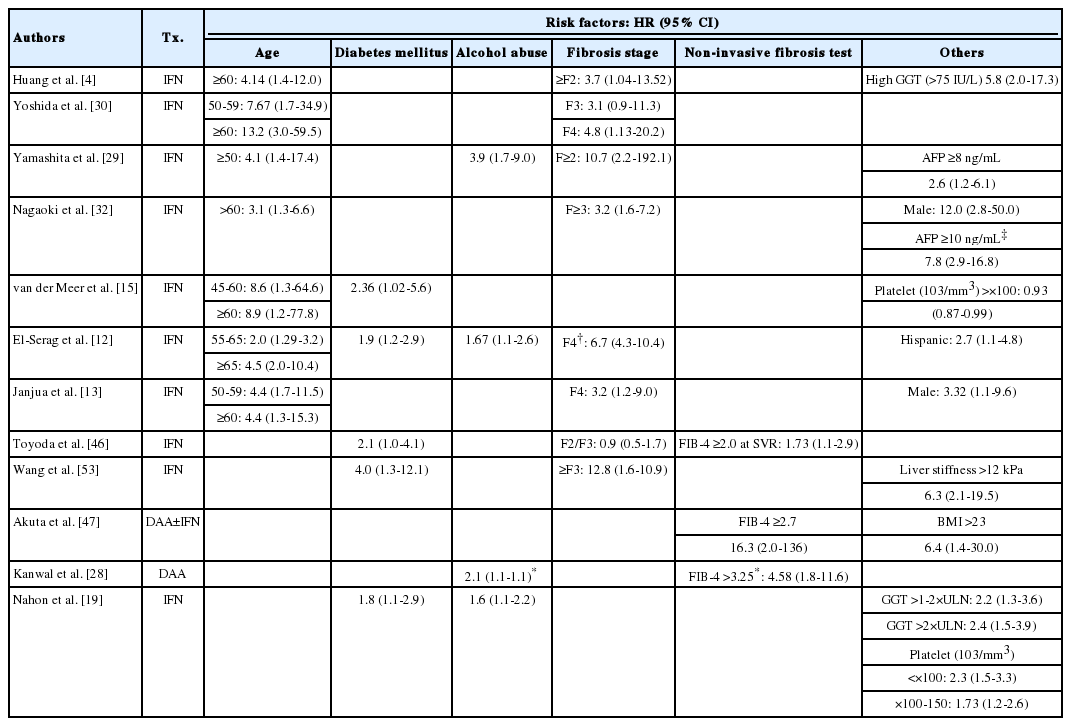
Hazard ratio of risk factors for hepatocellular carcinoma in patients with sustained virologic response (SVR)
The annual incidence of HCC increased up to 2.5–4.5% even in patient with SVR in advanced fibrosis or liver cirrhosis [4,5]. In some studies, the risk of HCC after SVR was also increased in patients with F2 fibrosis [4,29]. In contrast, the annual risk of HCC in patients with SVR in ≤F2 fibrosis might be less than 0.5% (Table 1) [11,29-32]. Therefore, based on the current evidences, routine surveillance for HCC in patients with F0-F2 fibrosis is not recommended [33-35].
However, Japanese studies have reported that HCC developed in several number of patients with F1/F2 fibrosis even after SVR. In a study by Yamashita et al. [29], 562 SVR patients were followed for median 4.8 years after IFN-based treatment. HCC developed in 31 patients (5.5%) after completion of IFN therapy. Among them, 35.5% (11/31) patients had pretreatment fibrosis F1 or F2. In their study, ≥F2 fibrosis was an independent risk factor for HCC. Ikeda et al. [31] reported that 12 of 706 (1.7%) of patients with F1/F2 fibrosis developed HCC with an annual incidence of 0.27% and 0.47% in F1 and F2, respectively. In another Japanese study [32], HCC developed in 3% (36/1,094) in patients with SVR after IFN therapy during median follow-up of 37 months (17–141 months). The cumulative rates of HCC according to fibrosis stage (F0/1, F2, F3, and F4) were 2%, 7%, 17%, and 22% at 10 years, respectively. Furthermore, the cumulative rates of HCC by fibrosis stage in males were 5%, 10%, 16%, and 20% at 10 years for F0/1, F2, F3, and F4, respectively (P=0.009).
There have been studies [4,11,30] that the annual incidence of HCC is higher than that of F2 fibrosis alone when the risk factors of other HCC are added in SVR patients with F2 fibrosis. Yoshida et al. [30] reported that the annual incidences of HCC was 0.1% in patients with F2 fibrosis, however, the annual incidence increased to 1.18% in men aged 60 years or older with F2 fibrosis. Huang et al. [4] reported that age ≥60, high GGT and F ≥2 fibrosis were independent risk factors for HCC in non-cirrhotic patients [4]. In non-cirrhotic patients with 1 risk factor (age ≥60 or high GGT), the annual incidence of HCC was 1.22%. In non-cirrhotic patients with 2 risk factors, the annual incidence of HCC increased to 2.8%. In patients with SVR without HCV-related cirrhosis, the annual incidence of HCC was 1.22% in patients older than 60 years of age and 0.14% in patients less than 60 years of age [4].
The 5-year cumulative risk of HCC was higher in SVR patients with metabolic features (body mass index of 25 kg/m2 or greater and/or diabetes and/or dyslipidemia) than in those without any metabolic features (30% vs. 8.8%; P=0.042) [19]. Whereas, HCC risk was similar in non-SVR patients with and without metabolic features (13.9% vs. 20.6%; P=0.91). These findings suggest that HCC surveillance tests might be needed in some patients with ≤F2 fibrosis with other risk factors for HCC.
The problem is that most of the studies reported so far are based on studies in CHC patients with biopsy-proven liver fibrosis, and it is practically impossible to perform biopsy to all patients before antiviral therapy in clinical practice. Recent guideline [33] recommends non-invasive fibrosis tests, such as liver stiffness measurement (LSM), aspartate aminotransferase-to-platelet ratio index (APRI), fibrosis-4 (FIB-4) index and commercial assays, instead of liver biopsy to assess liver disease severity in CHC patients prior to therapy. LSM is the most accurate non-invasive method for detecting cirrhosis in patients with viral hepatitis [36]. In low- and middle-income countries, as well as in settings where treatment expands outside of specialty clinics, if LSM was not available, APRI and FIB-4 are recommended [33] because they are generally available, simple and cheap, and the result is reliable [37-43]. The cut-off values of LSM, APRI and FIB-4 which predict the advanced fibrosis (≥F3), are 9.5 kPa, 1.5 and 3.25 [33,39,43-45].
Non-invasive fibrosis tests have been reported to predict the risk of HCC in patients with SVR (Table 5) [28,46-48]. Correlation between non-invasive fibrosis test and development of HCC is summarized in Table 4. Kobayashi et al. [48] retrospectively analyzed 605 patients with SVR after treatment with DAA (n=77) or IFN (n=528). The cumulative incidence of HCC in patients with FIB-4 >3.25 was not different between the DAA and IFN groups (9.66% vs. 8.37%). The cumulative incidence of HCC at 5 years in patients with FIB-4 ≤3.25 was 0% and 1.05% in DAA and IFN groups, respectively. According to Kanwal et al [28], alcohol abuse, diabetes, FIB-4 >3.25 were independent risk factors for HCC. Patients with FIB-4 >3.25 had an annual HCC incidence of 2.16% (95% CI, 1.78–2.54) compared with 0.45% (95% CI, 0.32–0.59) in patients with FIB-4 1.45 to 3.25, and 0.3% (95% CI, 0.14–0.46) in patients with FIB-4 ≤1.45.
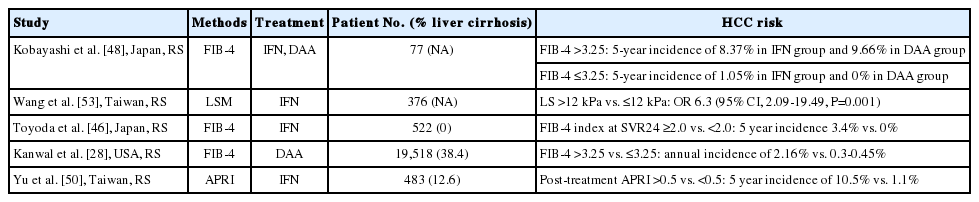
Noninvasive fibrosis tests predicting hepatocellular carcinoma (HCC) after sustained virologic response (SVR)
Some studies have shown that non-invasive liver fibrosis after treatment is more useful than before treatment [46,49,50]. Toyoda et al. [46] evaluated the usefulness of FIB-4 at the time of SVR as a risk factor for the HCC after median follow-up of 7.2 years in patients with SVR after IFN treatment. HCC developed in 3.5% (18/522) patients. The cumulative incidence of HCC was 1.2% at 5 years and 4.3% at 10 years. The presence of diabetes mellitus (risk ratio 2.08; P=0.045) and FIB-4 at the time of SVR, but not pretreatment liver fibrosis were associated with a higher risk of HCC. Yu et al. [50] evaluated the predictive value of APRI at 6 months after end of treatment (APRI-M6). Among the SVR group, the 5-year, and 10-year cumulative incidence of HCC was significantly higher in patients with APRI-M6 >0.5 compared to those with APRI-M6 <0.5 (10.5%, 25.7% vs. 1.1%, 1.1%; P<0.001).
LSM might be a promising test to predict the risk of HCC during active viral replication [37,51,52]. In a study [53] from Taiwan of 278 patients with SVR during a median follow-up period of 7.6 years, HCC developed in 17.4% (4/23) in patients with ≥12 kPa and even in 4.9% (5/103) with liver stiffness <12 kPa, respectively. Another study [54] from Korea suggested that stiffness threshold to predict HCC development was ≥7.0 kPa. So far, therefore there is no reliable threshold level of liver stiffness to predict HCC development in patients with SVR.
In a recent study of 115 SVR patients who underwent serial liver biopsy, Tachi et al. demonstrated that APRI or FIB-4 after SVR reflected liver fibrosis in patients with SVR [55]. However, non-invasive blood fibrosis tests have demonstrated poor correlation with post-SVR liver biopsy findings in another study [56]. Therefore, non-invasive blood fibrosis tests after therapy are not recommended to assess the fibrosis stage after therapy, as they are unreliable in this setting [33].
SURVEILLANCE FOR HCC IN PATIENTS WITH CHC WHO HAVE A QUIRED SVR AFTER ANTIVIRAL THERAPY
To decide whether to enter a patient into a surveillance program, the clinician should consider not only the risk level of HCC, but also the age, overall health status, and medical cost [57]. Until now, a definite threshold level of annual incidence of HCC is not clear, but it was reported that surveillance is cost-effective if the annual incidence is ≥1.5–2% per year in patients with HCV-related liver cirrhosis [58,59]. However, Lin et al. reported that surveillance for HCC in patient with HCV-related liver cirrhosis was cost-effective regardless of annual incidence [60]. There is little information about cost-effective analysis in patients with non-cirrhotic CHC, especially those who achieve SVR after treatment. Therefore, it is more difficult to determine the criteria for surveillance in these groups [57]. Nonetheless, several guidelines recommend surveillance for HCC if the annual incidence is ≥1.5% or advanced fibrosis or cirrhosis before treatment even after SVR after antiviral therapy [33,34,61-63].
Combining the results reported so far and the recommendation of several guidelines, surveillance for HCC should be performed in the following patients with SVR after antiviral treatment until new evidence is available: 1) biopsy proven advanced fibrosis (F3) or liver cirrhosis (F4); 2) clinical evidences of liver cirrhosis, such as ascites, esophageal/gastric varices; 3) splenomegaly with thrombocytopenia; 4) noninvasive fibrosis test suggesting advanced fibrosis (FIB-4 ≥3.24, APRI ≥1.5, LSM 9.5 kPa et al.). So far, there is not enough evidence to date in patient with F2 fibrosis, surveillance would be considered if there are additional risk factors for HCC, such as old age (≥60 years), diabetes mellitus, and alcohol abuse et al.
CONCLUSION
Even though, SVR after antiviral therapy dramatically decreased the risk of hepatic decompensation, HCC and death, the risk of HCC is not eliminated. The annual incidence of HCC in patients with liver cirrhosis have been estimated to be up to 4.5% even in patients with SVR. DAAs are applicable to all patients with HCV, including old age and more advanced liver disease. The development of HCC might be increasing even in patients with SVR. Therefore, identifying the high-risk groups of HCC and monitoring them continuously is an important clinical issue.
Notes
Author contributions
SK Na and BC Song were responsible for conception or design of the work, data collection, data analysis and interpretation, drafting the article, critical revision of the article, and final approval of the version to be published.
Conflict of Interest
The authors don’t have any conflict of interest.
Acknowledgements
This work was supported by the 2019 education, research and student guidance grant funded by Jeju National University.
Abbreviations
CHC
chronic hepatitis C
DAA
direct-acting antiviral agent
HCC
hepatocellular carcinoma
HCV
hepatitis C virus
IFN
interferon
SVR
sustained virologic response