A case of ruptured hepatic angiomyolipoma in a young male
Article information
Abstract
A 31-year-old male visited a local hospital due to sudden-onset severe abdominal pain. Abdominal computed tomography revealed a solid cystic mass with a size of approximately 12 cm and exhibiting both hemorrhage and fluid collection in the pelvic cavity. Emergency angiography and embolization were performed, and a large hepatic tumor was subsequently surgically resected. The tumor cells stained positive for human melanoma black-45 and smooth-muscle actin, and the pathologic diagnosis was hepatic angiomyolipoma. This case report also discusses the spontaneous rupture of a hepatic angiomyolipoma.
INTRODUCTION
Angiomyolipoma (AML) is an unusual mesenchymal tumor, composed of a varying heterogeneous mixture of three tissue components: blood vessels, smooth muscle, and adipose cells [1]. AML occurs most commonly in the kidneys, and the liver represents the second most frequent site of involvement [2]. Tuberous sclerosis may be associated in some cases of AML [3,4], but sporadic cases are also frequent.
With the increased use of imaging studies, most cases of AMLs are now discovered incidentally [5]. However, in renal AML, hemorrhage can be a presenting symptom, and micro-aneurysms are frequently reported [5]. There is a risk of spontaneous rupture and life threatening hemorrhage in renal AML, especially for lesions ≥4 cm or intralesional aneurysm >5 mm [4,5] These lesions are recommended for consideration of nephrectomy or selective arterial embolization, although surveillance with reimaging is also an option [5].
In contrast, there is limited information on the risks of rupture and hemorrhage in hepatic AML. Although there are many cases of hepatic AML reported in English literatures, most cases were focused on differential diagnosis of incidentally detected hepatic solid lesions [6]. As hepatic AML contains an inconstant proportion of fat, smooth muscle and blood vessels, sporadic hepatic AML have a varied appearance, making confident imaging diagnosis difficult in many cases [6]. Recently, we experienced a case of spontaneous rupture of hepatic AML in a young man, where pre-operative diagnosis was difficult. Herein we report this case with a literature review.
CASE REPORT
A 31-year-old male was referred to our hospital for a spontaneously ruptured hepatic tumor. Fifteen days earlier, he had presented to the local emergency room due to sudden onset severe abdominal pain localized in the right upper quadrant area. His blood pressure was 130/80 mmHg, heart rate 82 beats/min, body temperature 36.3°C and respiratory rate 16 breaths/min. Initial hemoglobin level was 7.1 mg/dL, prothrombin time 76.9%, albumin 4.1 g/dL, aspartate aminotransferase 20 U/L, and alanine aminotransferase 23 U/L. He complained of severe abdominal discomfort and tenderness on physical exam. The abdominal computed tomography revealed an approximately 12 cm sized mass in the right hepatic lobe, which showed a thin peripheral enhancing solid portion with an internal cystic component, and accompanying hemorrhage was noted (Fig. 1). Magnetic resonance imaging showed multiloculated cystic lesions with internal hemorrhage. There was no fat component in the enhancing solid portion, and diffusion restriction was also observed (Fig. 2). Emergent angiography with embolization was done, and he was referred to our hospital. He had no history of diabetes, hypertension or previous surgery. He was not taking any regular medication including anabolic steroid. His blood pressure was 146/70 mmHg, heart rate 73 beats/min, body temperature 36.8°C, and respiratory rate 20 breaths/min. Hemoglobin level was 11.3 mg/dL, prothrombin time 85%, albumin 3.8 g/dL, aspart aminotransferase 14 U/L, and alanine aminotransferase 16 U/L. Hepatitis B surface antigen was negative, anti-hepatitis B surface antibody was positive, and antihepatitis C antibody was negative. Alpha fetoprotein level was 1.3 ng/ml and the PIVKA-II test result was 44 mAU/mL. The patient underwent hepatic resection. Pathologically, a huge multilocular cystic mass, measuring 12.5×11.0×9.8, was noted (Fig. 3A). Microspically extensive necrosis of the tumor (about 60%) with a hemorrhage component was observed, without any fat component (Fig. 3B). Immunohistochemical staining showed diffuse positive staining for human melanoma black (HMB)-45 and multifocal positive staining for smooth muscle actin (Fig. 3C). Finally, the tumor was diagnosed as angiomyolipom, of the myomatous type. The patient recovered without complications after surgical resection.
(A) On arterial phase computed tomography (CT) images, a 12 cm sized mass is noted in the right hepatic lobe. The mass shows a thin peripheral enhancing solid portion (white arrow) with an internal cystic component. (B) On non-enhanced CT scan images, there is a high density (white asterisk) along the perihepatic space representing peritoneal hemorrhage by tumor bleeding.
(A, B) On T1 and T2 weighted magnetic resonance (MR) images, the mass has multiloculated cystic lesions with fluid-fluid levels representing internal hemorrhage (white asterisk). (C) On out-of-phase MR images, there is no fat component within the mass (white arrow). (D) On diffusion weighted images with b-value 800, the corresponding peripheral enhancing component shows high signal intensity indicating diffusion restriction (white arrow)

(A) On a cut section, there is a huge multilocular cystic mass (white arrow) measuring 12.5×11×9.9 cm, which is located at S5 and S6. (B) Spindle or epithelioid smooth muscle cells with eosinophilic cytoplasm and blood vessels (arrow) were seen on pathological findings (HE, ×200). But adipose tissue was rarely seen in this tumor. (C) Result of immunohistochemical staining , HMB-45 (HE, ×200).
DISCUSSION
Hepatic AML is a tumor capable of dual myomatous and lipomatous differentiation and melanogenesis, with HMB-45 positive myoid cells as the defining criterion [7,8]. Because of its protean morphologic appearance, various variant patterns have been recognized such as mixed, lipomatous, myomatous, and angiomatous types, including the epitheloid type with no or a minimal amount of fat [9]. Hence, a correct preoperative diagnosis of hepatic AML is demonstrated in only 20-52% of cases, especially in lipid poor AML [9].
The distinction of fat-deficient AML from other tumors, especially HCC, is very challenging. Jeon et al. suggested that the presence of early draining veins connected to prominent tumoral vessels and the absence of tumor capsules may help with the differentiation of fat-deficient AML in non-cirrhotic liver [10]. Kim et al. suggested homogeneous hypointensity in the hepatobiliary phase in gadoxetic acid-enhanced magnetic resonance imaging [9]. However, these findings were not observed in this case.
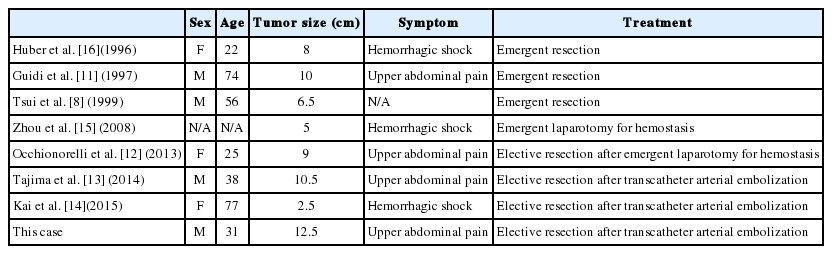
In differential diagnosis, demographic or clinical findings can be helpful. As malignant tumors such as hepatocellular carcinoma mostly develops in patients with risk factors (e.g., hepatitis B, hepatitis C or cirrhosis), identifying risk factors for hepatocellular carcinoma development is very important for differential diagnosis [7]. Age, sex and clinical behaviors also help with differential diagnosis. Hepatic adenoma can be suspected for women taking oral contraceptive therapy. Hemorrhage has been reported in 11-29% of hepatocellular adenoma cases, with nearly all instances of spontaneous rupture occurring in lesions ≥5 cm [7]. In cases of hepatic AML, ruptures are usually observed in middle aged women [8]. Spontaneous rupture and hemorrhage is uncommon, and to our best knowledge, there are only seven cases of hepatic AML presenting as a rupture (Table 1) [8,11-16]. The size of the tumors are usually large, and there are no gender or age preferences in the reported cases. In this case, the patient was a young man without risk factors for hepatocellular carcinoma and presented with a spontaneous rupture, fat-deficient case. Differential diagnosis was very challenging. The characteristic findings of hepatic AML are the presence of both fat and prominent vascularity in the same lesion. Conversely, less fatty and hypervascular hepatic mass accompanying hemorrhage radiologically suggested hepatocellular carcinoma or hepatic adenoma [7]. As he had no risk factors for hepatocellular carcinoma, the first differential diagnosis was hepatic adenoma in this case. The correct diagnosis could only be confirmed after resection of the tumor by immunohistochemical staining. In summary, we present a case of ruptured hepatic AML in a young male patient. This variant of hepatic AML should be included as a differential diagnosis of hepatic tumor presenting as a rupture.
Notes
Conflicts of Interest:The authors have no conflicts to disclose.
Abbreviations
AML
angiomyolipoma
HMB
human melanoma black