1. Wong MCS, Huang JLW, George J, Huang J, Leung C, Eslam M, et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat Rev Gastroenterol Hepatol 2019;16:57-73.


3. Lee SG, Moon DB, Hwang S, Ahn CS, Kim KH, Song GW, et al. Liver transplantation in Korea: past, present, and future. Transplant Proc 2015;47:705-708.


4. Lee JG, Lee KW, Kwon CHD, Chu CW, Kim BW, Choi DL, et al. Donor safety in living donor liver transplantation: the Korean organ transplantation registry study. Liver Transpl 2017;23:999-1006.


5. Park GC, Song GW, Moon DB, Lee SG. A review of current status of living donor liver transplantation. Hepatobiliary Surg Nutr 2016;5:107-117.


6. Korean Network for Organ Sharing (KONOS). Organ transplantation statistics; 2019;KONOS web site, <
http://konos.go.kr>. Accessed 26 Nov 2020.
7. Moreno R, Berenguer M. Post-liver transplantation medical complications. Ann Hepatol 2006;5:77-85.


8. Adam R, Karam V, Delvart V, OŌĆÖGrady J, Mirza D, Klempnauer J, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol 2012;57:675-688.


9. Bachir NM, Larson AM. Adult liver transplantation in the United States. Am J Med Sci 2012;343:462-469.


10. Durand F. How to improve long-term outcome after liver transplantation? Liver Int 2018;38 Suppl 1:134-138.


11. Durand F, Levitsky J, Cauchy F, Gilgenkrantz H, Soubrane O, Francoz C. Age and liver transplantation. J Hepatol 2019;70:745-758.


16. Humar A, Ganesh S, Jorgensen D, Tevar A, Ganoza A, Molinari M, et al. Adult living donor versus deceased donor liver transplant (LDLT versus DDLT) at a single center: time to change our paradigm for liver transplant. Ann Surg 2019;270:444-451.


17. Azzam A. Risk factors of hepatic graft failure, morbidity and mortality after living donor liver transplantation (LDLT): review article. Clin Res Trials 2018;4:1-11.

18. Zhu B, Wang J, Li H, Chen X, Zeng Y. Living or deceased organ donors in liver transplantation for hepatocellular carcinoma: a systematic review and meta-analysis. HPB (Oxford) 2019;21:133-147.


20. Yoon YI, Lee SG. Living donor liver transplantation for hepatocellular carcinoma: an Asian perspective. Dig Dis Sci 2019;64:993-1000.


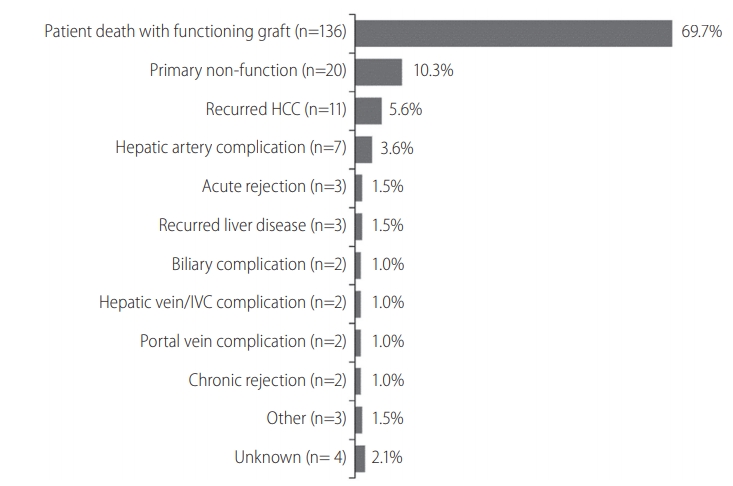
21. B├żckman L, Gibbs J, Levy M, McMillan R, Holman M, Husberg B, et al. Causes of late graft loss after liver transplantation. Transplantation 1993;55:1078-1082.


23. Gwiasda J, Schrem H, Klempnauer J, Kaltenborn A. Identifying independent risk factors for graft loss after primary liver transplantation. Langenbecks Arch Surg 2017;402:757-766.


24. Sharma R, Kashyap R, Jain A, Safadjou S, Graham M, Dwivedi AK, et al. Surgical complications following liver transplantation in patients with portal vein thrombosis--a single-center perspective. J Gastrointest Surg 2010;14:520-527.


25. Sandhu L, Sandroussi C, Guba M, Selzner M, Ghanekar A, Cattral MS, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: comparable survival and recurrence. Liver Transpl 2012;18:315-322.


26. Park HW, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. De novo malignancies after liver transplantation: incidence comparison with the Korean cancer registry. Transplant Proc 2012;44:802-805.


28. Lee S, Ahn C, Ha T, Moon D, Choi K, Song G, et al. Liver transplantation for hepatocellular carcinoma: Korean experience. J Hepatobiliary Pancreat Sci 2010;17:539-547.


29. Bahirwani R, Reddy KR. Outcomes after liver transplantation: chronic kidney disease. Liver Transpl 2009;15 Suppl 2:S70-S74.


31. Kim SG, Kim HJ, Lee JP, Lee SG, Kim YS, Ahn C, et al. Incidence and risk factors of renal dysfunction after liver transplantation in Korea. Transplant Proc 2004;36:2318-2320.


32. Lee SK, Park JB, Kim SJ, Choi GS, Kim DJ, Kwon CH, et al. Early postoperative renal dysfunction in the adult living donor liver transplantation. Transplant Proc 2007;39:1517-1519.


34. Cabezuelo JB, Ram├Łrez P, R├Łos A, Acosta F, Torres D, Sansano T, et al. Risk factors of acute renal failure after liver transplantation. Kidney Int 2006;69:1073-1080.


35. Barreto AG, Daher EF, Silva Junior GB, Garcia JH, Magalh├Żes CB, Lima JM, et al. Risk factors for acute kidney injury and 30-day mortality after liver transplantation. Ann Hepatol 2015;14:688-694.


36. Machicao VI, Srinivas TR, Hemming AW, Soldevila-Pico C, Firpi RJ, Reed AI, et al. Impact of implementation of the MELD scoring system on the prevalence and incidence of chronic renal disease following liver transplantation. Liver Transpl 2006;12:754-761.


37. Gonwa TA, Mai ML, Melton LB, Hays SR, Goldstein RM, Levy MF, et al. Renal replacement therapy and orthotopic liver transplantation: the role of continuous veno-venous hemodialysis. Transplantation 2001;71:1424-1428.


39. Heisel O, Heisel R, Balshaw R, Keown P. New onset diabetes mellitus in patients receiving calcineurin inhibitors: a systematic review and meta-analysis. Am J Transplant 2004;4:583-595.


41. Bodzin AS, Baker TB. Liver transplantation today: where we are now and where we are going. Liver Transpl 2018;24:1470-1475.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Supplement1
Supplement1 Print
Print



