Life-sustaining treatment and palliative care in patients with liver cirrhosis - legal, ethical, and practical issues
Article information
Abstract
With the enactment of the ‘Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life’ (Act No. 14013) in Korea, there is growing concern about the practicality of this law. In this review, we discuss definitions, ethics, and practical issues related to this law.
All hope abandon, ye who enter here.
Inferno, Divine Comedy
Dante (c. 1265 – 1321)
In many countries, elderly people make up an ever-growing proportion of the population. This population pattern has never occurred before in human history. Meanwhile, the prevalence of non-communicable diseases, such as heart disease, diabetes, dementia and cancer, is increasing rapidly. Combined, these changes place a heavy burden on healthcare systems [1].
Everyone hopes for a good death, or rather a good life until the very end, but little effort has been dedicated towards making that possible. Public engagement and policy intervention to improve quality of death (dying with dignity) through the provision of affordable access to end-of-life care has gained momentum in recent years [1].
ACTS ON LIFE-SUSTAINING TREATMENT AND PALLIATIVE CARE
In Korea, the ‘Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life’ was enacted in February 2016 (Act No. 14013). The act, which consists of 6 chapters and 43 articles, will be enforced on August 2017 (http://law.go.kr/lsEfInfoP.do?lsiSeq=180823#) [2]. However, the enforcement date of articles 9-20, 31, 33, 36, 37, 39, 40, and 43 was postponed to February 2018. This act will allow terminally ill patients to choose a life-sustaining treatment and will facilitate further development of palliative care in Korea. Interestingly, in articles 2 and 5, disease entities (cancer, AIDS, chronic obstructive pulmonary disease, ‘chronic’ liver cirrhosis, and other ordinance defining diseases) were specified in the act [2].
Since public perception of life-sustaining treatment and end-of-life care is strongly influenced by culture, the current status in other Asian countries will be briefly summarized.
In Taiwan, the “Natural Death Act” was passed in 2000. This act guarantees a patient’s right to request that medical staff do not resuscitate (DNR) them and gives the patient the right to reject other futile medical treatments at the end of their life. In 2015, Taiwan passed another law entitled the “Patient Autonomy Act”, which will be enforced in 2018. This law states that a patient may decline medical treatment according to his/her own will. This applies not only to terminally ill cancer patients but also to those who are irreversibly comatose, in a vegetative state, suffering from terminal dementia, or are experiencing intractable symptoms and suffering. Advance directives and advance care planning consultations are advised for every patient wishing to be covered under this law [3].
In 2002, the Hospital Authority of Hong Kong responded to Section 26 of “Care of the terminally ill” in the Professional Code and Conduct (November 2000) of the Medical Council of Hong Kong, delineating that the ethical principles and communication pathways in making decisions on withholding or withdrawing life-sustaining treatment, emphasizing the importance of a proper consensus-building process, and recommending approaches for handling disagreement [4].
In Japan, the “Cancer Control Act” was passed in 2007. Based on this law, the Japanese government developed the Basic Plan to Promote Cancer Control programs, which included promoting palliative care among its main focus areas. End-of-life care in Japan focused on patients with incurable cancer or acquired immunedeficiency syndrome (AIDS).
DEFINITION OF TERMS
Good death
A good death is ‘one that is free from avoidable suffering for patients, families and caregivers in general accordance with the patients’ and families’ wishes’. A good death, sometimes called ‘well dying’ in Korea, is defined using a measure assessing quality of life at the end of life [5].
Dying with dignity
Regarding the care of the terminally ill, it is important to allow patients to die with dignity. This may include (1) protecting the physical and psycho-spiritual integrity of the patient; (2) addressing the pain and suffering of the patient; (3) respecting the choices of the patient; and (4) treasuring the patient’s terminal phase of life. What constitutes ‘worthiness’ may vary among different individual. It may be affected by one’s values, past experiences, and cultural, social and religious background [4].
Life-sustaining treatment
This refers to all treatments that have the potential to postpone the patient’s death. The Korean ‘Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life’ specifies 4 life-sustaining treatments - cardiopulmonary resuscitation, artificial ventilation, hemodialysis, and anticancer chemotherapy. In other countries, blood products, pacemakers, vasopressors, and antibiotics have been considered life-sustaining treatments, along with artificial nutrition and hydration (BMA 1999, Section 3.2) [4].
End-of-life
End-of-life is defined as a condition in which a patient is unlikely to recover from a worsening condition despite aggressive treatment, ultimately leading to the patient’s death within months. (Korean Act No. 14013, Article 2) However, clinical outcomes of patients at the end-of-life are quite variable. Occasionally it is difficult to pinpoint a specific time as the end-of-life.
Because of modern technical and medical developments and the belief in the potential for success due to treatment, treatments persist that focus on cures and life-prolonging interventions until the last stages of life, even when they are no longer warranted or beneficial in hospital settings [6].
Although the terms ‘palliative care’ and ‘end-of-life care’ are sometimes used interchangeably, the latter is often taken to mean care delivered only during the final stages of a terminal illness [1].
Last days of life (final days of life)
Last days of life refers to any situation in which a patient has a condition with no possibility of recovery despite aggressive treatment, where the symptoms are worsening rapidly and death is imminent (Korean Act No. 14013, Article 2).
Terminally Ill
Terminally ill patients suffer from advanced, progressive, and irreversible diseases and fail to respond to curative therapy, yielding a short life expectancy ranging from days or weeks to a few months [4].
Palliative care
Palliative care is an approach that improves the quality of life for patients and families that are dealing with life-threatening illness through the prevention and relief of suffering by means of early identification and treatment of pain and other physical, psychosocial and spiritual problems. The goal is neither to hasten or postpone death but to affirm one’s life and to be able to regard dying as one of the natural processes of life (Fig. 1) [7].
Hospice
Hospice care is end-of-life care provided by health professionals and volunteers. They provide medical, psychological and spiritual support to the patient. The goal of hospice care is to help people who are dying to have peace, comfort and dignity. Caregivers attempt to control pain and other symptoms so that a person may remain as alert and comfortable as possible (Fig. 1) [7.8].
Advance care planning
Advance care planning is a process for patients at all stages of life that want to be able to plan their future health care. Advance care plans provide direction for healthcare professionals when a patient is not in a position to either make and/or communicate their own healthcare choices. The main components of advance care planning include the nomination of a substitute decision maker (proxy designation) and the completion of documents such as advance directives, physician orders for life-sustaining treatment (POLST), or other similar documents [9].
Advance directives
Advance directives are prospective decisions about treatment made by patients who may be unable to participate directly in future medical decision-making. Periodic reviews of directives are required to ensure that the patients’ current wishes and circumstances are accurately reflected [10-12].
Advance directives may go by other names in different states (e.g. living will, health care power of attorney); however, regardless of the term used, it is a ‘legal document’ that provides guidance about what types of treatments a patient may want to receive in case of potential future medical emergencies; this document is also where patients designate a surrogate (proxy). All adults are able to have advance directives (Table 1) [13-15].
Physician Orders for Life-Sustaining Treatment (POLST)
This may also go by other names in different states; however, regardless of the term, the POLST is a ‘medical order’ for specific medical treatments the patient may want based on his/her diagnosis, prognosis and goals of care. A POLST is only recommended for individuals with a serious illness or frailty near the end-of-life [13,15]. A DNR order is a part of POLST.
Health care professionals should ask patients for a copy of their advance directives prior to completing a POLST form in order to complete a review of the documents to ensure that the advanced directives complement the potential POLST in order to avoid future confusion. While a POLST is meant to complement the advance directives, it does not replace the advance directives (Table 1) [13,15].
Artificial nutrition and hydration
Artificial nutrition and hydration refers specifically to techniques used for providing nutrition or hydration in order to bypass the swallowing process. These techniques include the use of nasogastric tubes, percutaneous endoscopic gastrostomy, intravenous or subcutaneous fluid, and parenteral nutrition (BMA 1999, Section 3.4). Artificial nutrition and hydration are different from offering oral nutrition and hydration. The latter is considered basic care and should never be withheld or withdrawn (BMA 1999, Section 3.5) [4].
Even if it is requested/supported by the family and there is consensus within the care team, the proposal to withhold or withdraw artificial nutrition and hydration requires a formal clinical review and should be reported to and reviewed by the hospital ethics committee to ensure that the appropriate procedures are being followed [4].
Futility
Futility occurs when clinical reasoning or experience suggests that a life-sustaining treatment is highly unlikely to achieve its purpose. As costs and benefits sometimes involve quality-of-life considerations and can be value-laden, the decision-making process for establishing futility is thus a consensus-building process between the health care team and the patient and family [4].
THE ETHICS OF RESUSCITATION AND END-OFLIFE DECISIONS
Ethical principles
- The principle of Respect for Autonomy: Respect the right of a mentally competent individual to consent or to refuse clinically indicated medical treatment including life-sustaining treatment. This choice should be based on adequate information, and the individual takes responsibility for such choice [4].
Informed decisions require that individuals receive and understand accurate information about their condition and prognosis, as well as the nature, risks, benefits, and alternatives of any proposed interventions [4,10,16,17].
- The principle of Beneficence: Duty of care and due regard for patients’ welfare and interests to preserve life, relieve suffering, and limit disability. Related professional terms and concepts include ‘patient’s best interests’ and ‘patient’s benefit’ [4,10].
- The principle of Non-Maleficence: “Do no harm” to avoid prolonging suffering by utilizing futile interventions and to adequately consider the risks and harms of interventions [4,10].
- The principle of Justice and Equity: Justice implies that health resources are distributed equally and fairly, regardless of the patient’s socioeconomic status, in the absence of discrimination, with the right of each individual to receive the current standard of care. ‘Equity’ is often considered a related concept. An individual should not be unfairly treated or discriminated based on disability, age, socioeconomic status, etc. On the other hand, an individual cannot claim unlimited rights (e.g. the right to be treated at all costs) without considering the impact on other persons or potential scarcity of resources [4,10].
Cultural context should be considered when interpreting the above principles. In Korean culture, the concept of the self may be different from the Western concept and has more to do with familial relations. The role of the family in decision-making may also be more important than it is in Western societies. Therefore, it acknowledges the importance of involvement of the family in the decision-making process, although the views of the family cannot override those of a mentally competent patient [4].
LIFE-SUSTAINING TREATMENT AND PALLIATIVE CARE IN GENERAL
The relationship between disease-modifying treatment and palliative care
The relationship between disease-modifying treatment and palliative care may vary in different countries and societies for a variety of reasons. However, it is consistently emphasized that palliative care should in no way act as a substitute for appropriate disease-modifying treatment (Fig. 1) [7].
In high-income countries, death is frequently medicalized, and disease-modifying treatment may be prioritized ahead of palliative care. Interestingly, a majority of deaths occur in hospitals in South Korea, and according to a previous study on international place of death, South Korea has one of the highest hospital death rates [18]. In certain cultures, death and dying are stigmatized, and commonly held perceptions and taboos need to be challenged before palliative care provision can even be addressed [7].
Palliative care, while still a relatively new component of modern healthcare, is increasingly recognized as an essential part of all healthcare systems. Since the early 1980s, the need for palliative care for cancer patients has been increasingly acknowledged worldwide. More recently, there has been increased awareness of the need for palliative care for other chronic diseases or conditions, such as HIV/AIDS, congestive heart failure, cerebrovascular disease, neurodegenerative disorders, chronic respiratory diseases, drug-resistant tuberculosis, and diseases of the elderly. However, there remains a need for palliative care for these chronic life-limiting health problems in most parts of the world [7].
WHO’s estimate of people in need of palliative care at the end-of-life worldwide
The estimated global number of adults in need of palliative care at the end-of-life is over 19 million. The majority of adults in need of palliative care were those who were diagnosed with cardiovascular diseases (38.5%) and cancer (34%), followed by chronic respiratory diseases (10.3%), HIV/AIDS (5.7%), and diabetes (4.5%) (Fig. 2) [7].
LIFE-SUSTAINING TREATMENT AND PALLIATIVE CARE IN PATIENTS WITH LIVER CIRRHOSIS
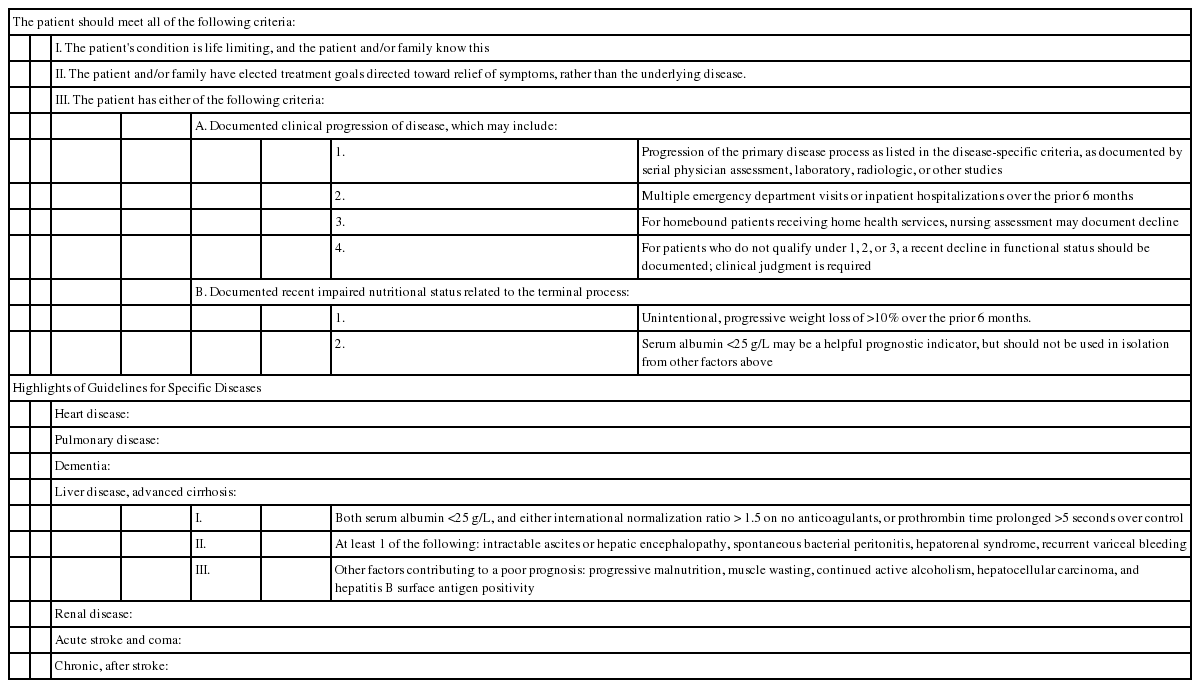
NHPCO Guidelines for hospice enrollment in patients with liver cirrhosis: Out of date
In 1996, in an effort to assist clinicians and regulators in determining which patients could be enrolled in hospice, the National Hospice and Palliative Care Organization (NHPCO) published medical guidelines for hospice enrollment in patients with non-cancer diagnoses (Table 2). The guidelines were cited as follows: Local Medical Review Policies (implemented by Medicare intermediaries in the Unites States of America) have modified these guidelines, particularly by mandating some of the optional elements. In addition, hospices have adjusted their own enrollment criteria in order to limit risks of denied payments or allegations of fraud. Currently hospices vary substantially in their interpretations of eligibility [19,20].
However, the NHPCO Guidelines do not reflect medical advances from the past 20 years and are far from optimal at present.
KASL’s official opinion on the definition of ‘end-of-life’ for patients with liver disease
Last year, KASL (Korean Association for the Study of the Liver) replied to the request of KAMS (Korean Academy of Medical Sciences) about the definition of ‘end-of-life’ for patients with liver disease and further explained as follows (Table 3) [21-24].
- Unlike NHPCO criteria, the prothrombin time and albumin, indicating synthetic function of the liver, cannot be used solely as criteria for determining the severity, prognosis, or irreversibility of liver disease. Moreover, the cut-off points for albumin and prothrombin time described in these criteria are unreasonable. It is reasonable to introduce the Child-Pugh classification, which is widely used to determine the progression of cirrhosis, as criteria for end-stage liver disease.
- Liver transplantation is considered a priority whenever possible. Liver transplantation could change the natural course of terminally ill patients with liver cirrhosis.
- Liver cirrhosis is no longer considered an irreversible disease. Recent studies have repeatedly shown the reversibility of advanced liver disease, including liver cirrhosis, with antiviral treatment, abstinence, and other appropriate medical treatments.
- Intractable ascites should be excluded from the criteria. Large volume paracentesis with albumin infusion is a recommended therapy, and many patients maintain a relatively stable state over a long period of time. Intractable ascites can also be improved by TIPS (transjugular intrahepatic portosystemic shunt).
- Spontaneous bacterial peritonitis should be excluded from the criteria. With broad-spectrum antibiotics, spontaneous bacterial peritonitis is reversible in most patients.
- ‘Hepatorenal syndrome’ should be changed to ‘hepatorenal syndrome that does not improve despite active treatment’. With standard treatment using vasoactive agents such as terlipressin and albumin, hepatorenal syndrome is reversible and can be treated in many patients.
- ‘Hepatic encephalopathy’ should be changed to ‘serious hepatic encephalopathy that does not improve despite active treatment’. It is reasonable to exclude minimal, subclinical, and mild hepatic encephalopathy.
- It is reasonable to limit variceal bleeding to ‘variceal bleeding which does not show improvement despite active treatment’. Even for recurrent variceal bleeding, there are several treatment options, such as BRTO (balloon occluded retrograde transvenous obliteration) and TIPS, with which many patients could expect long-term survival.
ARGUMENTS ABOUT THE KOREAN ACT (ACT NO. 14013)
Determination of life-sustaining treatment and supporting patients with palliative care are different from each other. By attempting to touch on two different subjects within the same Act, confusion and concern are inevitable. Without meticulous ordinances and regulations by the Ministry of Health and Welfare, enforcement of the Act would not be practical.
In Korean culture, relationships within a family are more important than in Western countries, where family members are not able to substitute a patient’s legal right without proxy designation. The discrepancy between Korean culture and American-style law may cause problems. For example, usual DNR orders and other POLST after discussion with family members will be illegal after February 4th, 2018.
As noted in the WHO report, cardiovascular diseases (38.5%) and cancer (34%), followed by chronic respiratory diseases (10.3%) and HIV/AIDS (5.7%), need palliative care. However, the Korean Act specifies 4 diseases (cancer, AIDS, chronic obstructive pulmonary disease, and ‘chronic’ liver cirrhosis) in its definition of ‘end-of-life’. Most patients diagnosed with end-stage liver disease with serious complications need special care from hepatologists rather that general palliative care. It is reasonable to exclude or limit the scope of patients with liver disease from ‘end-of-life’ patients covered by this law to ensure the proper management of patients.
Notes
Conflicts of Interest:The authors have no conflicts to disclose.
Abbreviations
BRTO
balloon occuluded retrograde transvenous obliteration
DNR
do not resuscitate
HIV/AIDS
human immunodeficiency virus/acquired immune deficiency syndrome
KAMS
Korean Academy of Medical Sciences
KASL
Korean Association for the Study of the Liver
NHPCO
National Hospice and Palliative Care Organization
POSLT
physician orders for life-sustaining treatment
TIPS
transjugular intrahepatic portosystemic shunt
WHO
World Health Organization