Clinical implications of advances in liver regeneration
Article information
Abstract
Remarkable advances have been made recently in the area of liver regeneration. Even though liver regeneration after liver resection has been widely researched, new clinical applications have provided a better understanding of the process. Hepatic damage induces a process of regeneration that rarely occurs in normal undamaged liver. Many studies have concentrated on the mechanism of hepatocyte regeneration following liver damage. High mortality is usual in patients with terminal liver failure. Patients die when the regenerative process is unable to balance loss due to liver damage. During disease progression, cellular adaptations take place and the organ microenvironment changes. Portal vein embolization and the associating liver partition and portal vein ligation for staged hepatectomy are relatively recent techniques exploiting the remarkable progress in understanding liver regeneration. Living donor liver transplantation is one of the most significant clinical outcomes of research on liver regeneration. Another major clinical field involving liver regeneration is cell therapy using adult stem cells. The aim of this article is to provide an outline of the clinical approaches being undertaken to examine regeneration in liver diseases.
INTRODUCTION
The liver possesses the specific competence to return to a constant size within a short period after injury.1,2 We can observe this clinically in the form of regeneration after liver resection or liver transplantation, and after toxic liver injury. Liver regeneration involves hyperplasia of all the cell types of the liver. In humans, hapatocyte replication generally starts within a day of major hepatectomy, and replication of non-parenchymal cells, such as endothelial cells, Kupffer cells, and biliary cells begins somewhat later.3 Intensive research on liver regeneration has been carried out for several years (Table 1). But the molecular signals responsible for maintaining an original liver volume are unclear. However it stands to reason that the liver keeps up a delicate balance between cell loss and excess growth.4 Remarkable advancements that are directly relevant to clinical problems have been made in our understanding of liver regeneration. Moreover new experimental approaches have provided us much more information of hepatic failure and liver regeneration.5 The aim of this review is to survey recent progress in understanding liver regeneration. Greater understanding will lead to safer operations on living donors and on patients with huge or multiple liver masses. Furthermore it should provide to the development of new treatment strategies and diagnostic procedures for various liver diseases.
MECHANISM OF LIVER REGENERATION
After liver resection, the residual liver responds by undergoing hyperplasia (Fig. 1).1 Upon partial hepatectomy, non-diving mature hepatocytes quickly reenter the cell cycle. Throughout proliferation, liver recover its own volume. There are two main proposals concerning the physiological triggers for liver regeneration.6 One is that the increased energy demand per unit liver volume after partial hepatectomy generates an early stress signal.7 The other is that liver regeneration is triggered by altered hemodynamic factors. Although there is a definite correlation between blood flow and liver regeneration, the definite role of blood flow in liver regeneration remain unclear.6 Similar liver regeneration can be initiated after several different hepatic injuries including viral and toxic hepatitis.

Ki-67 immunostating for regenerating rat liver following 2/3 liver resection. Ki-67 positive hepatocytes indicating hepatoctyes are proliferating after hepatectomy. Most of hepatocytes are stained with Ki-67.
Standard liver regeneration
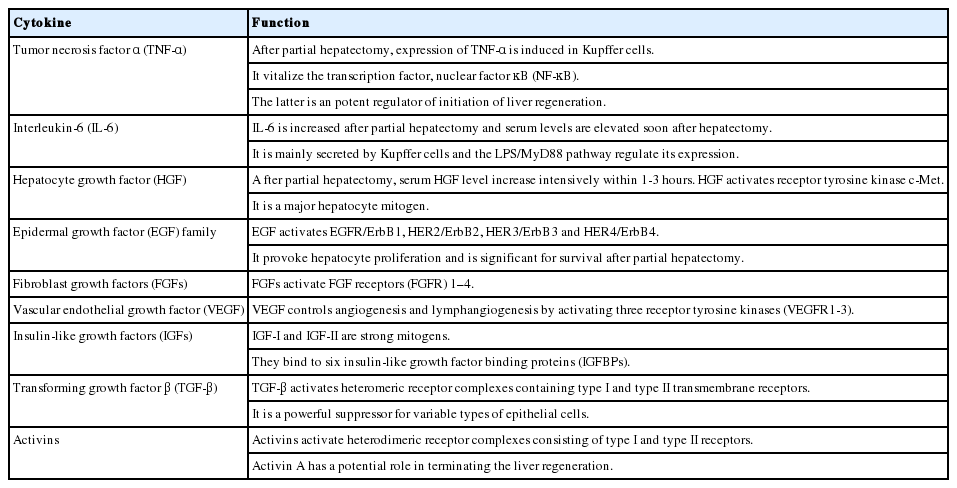
Usually hepatocytes are non-dividing (G0 phase) in the normal liver. After liver injury, they enter the G1 phase. Tumor necrosis factor α (TNF-α) and interleukin-6 (IL-6) are released from Kupffer cells, and these contribute to the initiation of the cell cycle (G0 to G1) by binding to their receptors.8,9 Several factors for instance hepatocyte growth factor (HGF), epidermal growth factor (EGF), and transforming growth factor α (TGF-α) are thought to initiate the G1 to S transition.10 These factors stimulate DNA replication and mitosis by binding to their corresponding receptors.11 TGF-β1 is a noted inhibitor of hepatocyte proliferation.12 In the normal liver, growth factors and TGF-β have agonistic effects. At the begining of regeneration, the HGF signal is more powerful than that of TGF-β, whereas at the termination of regeneration, the original balance is restored.13 Activin is an inhibitor of liver regeneration that selectively suppress hepatocyte proliferation. When the liver volume returns to its own size, activin A, apoptosis and other factors may terminate the regeneration process.14 Table 2 summarizes the properties of various cytokines and growth factors engaged in liver regeneration.15 Shear stress is the powerful stimuli for liver regeneration. After liver resection, the increased portal vein flow past hepatocytes or sinusoidal endothelial cells initiates regeneration and regulates the size of the liver. Shear stress on the endothelial cells is the powerful impetus for regeneration, liver volume regulation, and growth, as well as atrophy.16 Hemodynamic factors increase the shear stress in the liver, and nitric oxide (NO) is secreted. NO then initiates the liver regeneration cascade.17
Oval cell-mediated liver regeneration
Oval cells are detected after partial hepatectomy when hepatocyte proliferation is suppressed in the rat or mouse models. It is very difficult to find oval cell mediated liver regeneration in the chronic liver disease patients. Their origin is unclear, but there is considerable evidence that they derive from the biliary component.18 Unlike in standard liver regeneration, in oval cell-medicated regeneration there is no hepatocyte proliferation. When hepatocyte proliferation is constrained, bile duct cells reproduce and expand into many oval cells. Gene expression in these cells has characteristics of both biliary cells and hepatocytes. The oval cells transform into a hepatocyte phenotype.19
CLINICAL APPLICATIONS OF LIVER REGENERATION
Recent research for liver regeneration is focused on human liver disease treatment especially for various hepatectomy for chronic liver disease and hepatic tumors. For these innovative researches on liver regeneration, hepatectomy outcomes have markedly improved over recent decades.20 However post-hepatectomy liver failure (PHLF) remains one of the most dangerous and life-threatening complications of hepatectomy, and takes place in up to 10% of cases.21 A number of different criteria are used for PHLF. One of the most frequently used in clinical practice is the 50-50 criterion that combines a PT index <50% and serum total bilirubin >50 µmol/L (>2.9 mg/dL) on post-operative day (POD) 5.22 In 2011, the International Study Group of Liver Surgery (ISGLS) described the three grades of PHLF.23 This kind of criteria could be established because of marked increase of understanding of clinical aspect of liver regeneration potential in chronic liver disease patients.
Portal vein embolization
Portal vein embolization (PVE) is the best example of how liver regeneration research has influenced clinical application. PHLF is associated with a small relative residual liver volume.24 Two-stage liver resection after portal vein occlusion (PVO) is one of the best strategies for volume manipulation.3 PVE was first described by Kinoshita in 1980s.25,26 In general, two approaches exist for portal vein occlusion: radiological PVE and surgical portal vein ligation (PVL). After liver injury, various activated growth factors are carried from the intestine to the liver. These factors run through the portal flow, not the hepatic artery, and induce a number of molecular and cellular changes.27 PVO induces apoptosis in the same side lobe, and proliferation of the opposite side lobe.28 PVE is indicated only if there is a high risk of a small relative residual liver volume after hepatectomy.29 There are no universal guidelines. Schindl et al. observed a relationship between liver dysfunction score and relative residual liver volume, and they identified a critical minimum relative residual liver volume of 26.6% that was needed to avoid serious hepatic dysfunction.24 In normal livers, if the size of the liver remnant is likely to exceed 30% of the original volume, hepatectomy can be performed safely. In cirrhotic livers, the threshold is 50% based on our current practice and available data.3
Living donor liver transplantation
Living donor liver transplantation is state of the art of liver regeneration research. Even though wonderful clinical outcomes from Asian large volume centers, there are still obstacles to be overcome. In 2008, Ghobrial et al. examined donor morbidity following living donor liver transplantation. Overall complications were 38% (148 donors had a total of 220 complications). According to the Clavien grading system, there were 48% grade 1 complications, 47% grade 2, <4% grade 3 and 1.4% grade 4 (leading to death).30 For donor safety, it is necessary to minimize the size of the graft. However, graft size is positively related to recipient prognosis, and a balance between the two must be maintained. In terms of donor safety and recipient prognosis, research on liver regeneration is essential for improving clinical outcomes.
Small-for-size graft syndrome
Understanding about liver regeneration has been made some progress for treating small-for size graft syndrome following living donor liver transplantation. Small-for-size graft syndrome is defined as long-lasting cholestasis and refractory ascites.31 Long-lasting cholestasis is defined as total bilirubin >10 mg/dL on POD 14, and refractory ascites is defined as an amount of ascites of >1 L/day on POD 14 or >500 mL/day on POD 28.32
In 2008, Ikegami et al. summarized the reason of small-for-size syndrome and outlined potential solutions. The former involved graft size, quality, and flow as graft-related factors, and portal hypertension and the severity of the liver disease as recipient-related factors. Right lobe grafts, auxiliary transplants, and dual graft transplants were described as strategies for overcoming insufficient graft size. For poor graft quality, use of younger donors and donor diet programs for steatosis were possible strategies. Various shunt and graft operations were considered for excessive inflow and insufficient outflow drainage. Larger grafts and appropriate flow were considered ways of dealing with poor general recipient condition.33
Associating liver partition and portal vein ligation for staged hepatectomy
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) refers to in situ splitting and iatrogenic portal vein obliteration aimed at inducing rapid liver hypertrophy; it was first introduced by Hans Schlitt in 2007.34 Schnitzbauer et al. performed PVL with in situ splitting in 2012. This approach induced median hypertrophy of 74%, and yielded results superior to PVL or PVE alone.35 Knoefel et al. demonstrated that ALPPS offered an chance for curative hepatectomy even after PVE had failed and had resulted in insufficient growth of the liver remnant (Fig. 2).36
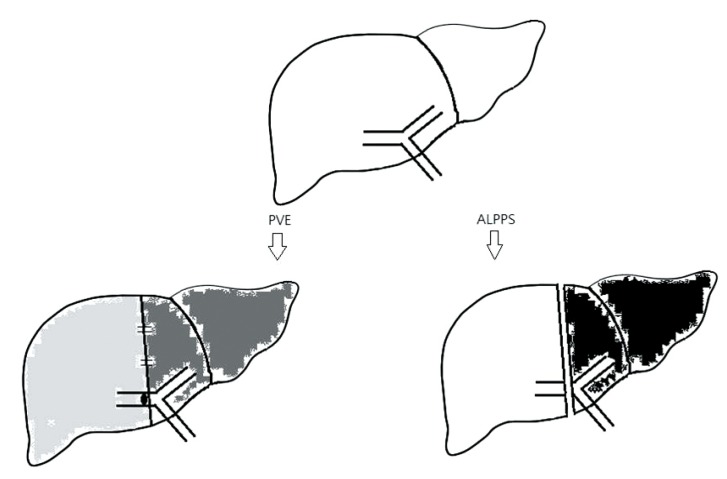
Portal vein embolization (PVE) versus associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). PVE is radiological method, and so less invasive. However a shunt is opened in the liver. ALPPS is more invasive than PVE, because surgery is needed, but complete isolation is achieved.
Stem cells and liver regeneration
In 2007, Takahashi et al. generated pluripotent stem cells from adult human fibroblasts.37 This approach could lead, in the foreseeable future, to a remarkable change of therapeutic strategy in the area of cell-based therapies for life-threatening liver diseases. Recently there have been clinical trials of transplantation of mature hepatocytes, but the long-term effect is uncertain. If we can get over these problems, we will use variable stem cells, such as autologous induced pluripotent stem cells, mesenchymal stem cells, and endogenous hepatic stem/progenitor cells, as possible materials for transplantation.38
RECENT TRENDS AND FUTURE PERSPECTIVES
Tissue engineering can be a useful therapeutic option that combines cells, biological scaffolds and active molecules.39 Three-dimensional (3-D) scaffolds play a critical role in tissue engineering by regulating cell functions and inducing the formation of new tissues and organs. They supply adequate space for the transplanted cells, as well as physical and biological signals that promote adhesion, migration, proliferation and differentiation, and they also gather the cells that have proliferated, and released matrices, into functional tissues and organs.40 In 2010, Ott et al. created an artificial biological lung from decellularized lungs. They made these lungs by detergent perfusion and succeeded in generating scaffolds that contained vasculature, airways and alveoli without cell. Thereafter they were able to successfully transplant the regenerated artificial lungs into the orthotopic position.41 In 2010, Uygun et al. demonstrated the architecture of a decellularized 3-D liver, as well as its functional vasculature and the original matrix composition. Furthermore, they achieved recellularization of the graft in vitro. This artificial liver was viable on its own.42 In 2013, Takebe et al. constructed a functional human organ from pluripotent stem cells. They generate functional human liver with vasculature from human induced pluripotent stem cells by transplantation of liver buds created in vitro.43 3-D printing refers to a variety of processes for making three-dimensional objects from a 3D models or other electronic data sources primarily through an additive process in which successive layers of material are laid down under computer control. In the near future, we should be able to generate bio-printed livers using 3D printing technology.
CONCLUSIONS
Liver regeneration has been well known for centuries, and in recent decades we have begun to understand its mechanism. Recent researches have focused on understanding liver regeneration after liver resection and liver transplantation. The use of innovative approaches could change strategies for treating liver dysfunctions such as PHLF and small-for-size graft syndrome. Liver regeneration has numerous applications. The use of PVO should permit the removal of large volumes of liver tissue with a diminished risk of liver failure. Hepatocyte transplantation could repopulate the liver of patients with inborn error metabolism. Moreover, regenerative therapy could provide innovative support for living donor transplantation. In the near future, we will be able to make artificial livers constructed from an individual's own cells. This would be the perfect way to support liver transplantation without the need for immunosuppressant drugs. In conclusion, the research of liver regeneration provides new strategies for the detection and treatment of a variety of liver diseases.
Notes
Conflicts of Interest: The authors have no conflicts to disclose.
Abbreviations
ALPPS
associating liver partition and portal vein ligation for staged hepatectomy
EGF
epidermal growth factor
HGF
hepatocyte growth factor
IL-6
interleukin-6
ISGLS
international study group of liver surgery
PHLF
post-hepatectomy liver failure
POD
post-operative day
PVE
portal vein embolization
PVO
portal vein occlusion
TGF-β
transforming growth factor beta
TNF-α
tumor necrosis factor alpha