INTRODUCTION
Caroli's disease belongs to a group of hepatic fibropolycystic diseases. It is characterized by multifocal congenital dilatations of the intrahepatic bile ducts, which may be diffuse or limited, presenting in a sack form that produces cystic structures, which communicate with the biliary tree. Two types have been described: a pure form or Caroli's disease (type 1) and a complex form associated with congenital hepatic fibrosis or Caroli's syndrome (type 2).12 Clinical symptoms of Caroli's disease include right upper quadrant abdominal pain, jaundice, and recurrent cholangitis.34 Bacterial cholangitis occurs frequently and may be complicated by hepatic abscess formation and sepsis. Recurrent cholangitis dominates the clinical course and is the principal cause of morbidity and mortality. Caroli's disease limited to 1 liver segment is extremely rare, and there have been only a few cases of segmentectomy for Caroli's disease in Korea. In this report, we present a case of Caroli's disease that was misdiagnosed as an intraductal papillary neoplasm of the bile duct (IPNB) and was treated with segmentectomy.
CASES
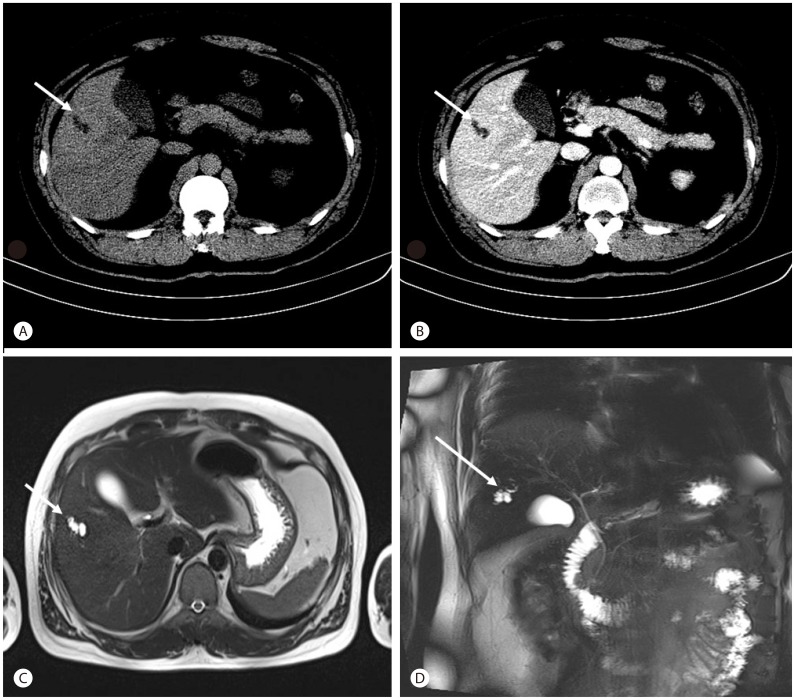
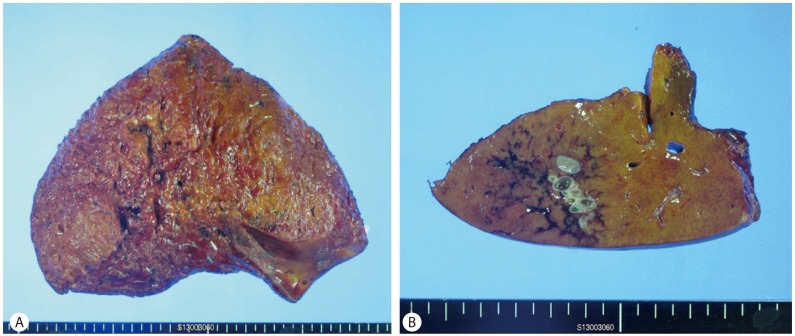
A 30-year-old man with no underlying diseases visited our hospital for further evaluation and treatment of a liver mass discovered on abdominal computed tomography (CT) scan at another hospital. This patient was asymptomatic on transfer to our hospital. The physical examination showed no abnormality, and the initial vital signs were as follows: body temperature, 36.9Ōäā; pulse rate, 70 beats/min; respiratory rate, 20 breaths/min; and blood pressure, 120/70 mmHg. His height and body weight were 179 cm and 93.4 kg, respectively. He consumed 120-180 g of alcohol per week, and his medical history and familial history were unremarkable. Laboratory examinations showed a white blood cell count of 5,800/┬ĄL, hemoglobin level of 15.9 g/L, and platelet count of 272,000/┬ĄL. The only abnormal finding on the liver function test was mildly elevated alanine transaminase levels, and the results were as follows: serum aspartate transaminase, 42 IU/L; alanine transaminase, 76 IU/L; alkaline phosphatase, 58 IU/L; gamma-glutamyl transferase, 82 IU/L; total bilirubin, 0.69 mg/dL; albumin, 5.3 g/dL; and international normalized ratio, 0.98. CA 19-9 and ╬▒-fetoprotein for malignancy work-up was carried out; 5.7 IU/mL and 3.6 ng/mL, respectively. Results for viral markers including hepatitis B surface antigen and anti-hepatitis C virus were negative. Abdominal CT (Fig. 1A, B) performed at the other hospital and abdominal magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) (Fig. 1C, D) performed at our hospital revealed a localized bile duct dilatation measuring 2.0├Ś0.8 cm in liver segment 5 without a demonstrable intraductal mass lesion and underlying steatosis of the liver. Although an obstructing lesion was not found on the images, we considered the duct obstructed with a mass or parasite proximal to the dilated ductal area because size of the dilated ductal site was very limited and could not find any evidence of other bile duct disease. Assuming that the lesion of the localized bile duct dilatation in liver segment 5 was due to an IPNB, we decided to perform surgery after consultation with the general surgery department because the possibility of malignancy with IPNB could not be excluded. He was transferred to the general surgery department and underwent segmentectomy of liver segment 5. Although the 16├Ś7├Ś16 cm resected liver specimen showed grossly unremarkable findings on the surface or inner surface (Fig. 2A), a diffuse parenchymal hemorrhagic soft dilated lesion was noted in the 4.5├Ś3.5 cm cut surface, 0.5 cm from the resection margins in a serial section of the specimen (Fig. 2B). Histopathologic findings showed congenital dilatation of the intrahepatic bile ducts (Caroli's disease) with approximately 50% centrilobular macrovesicular type fatty change (Fig. 3). This patient is seen regularly at the outpatient department and has no complications 5 months after surgery.
DISCUSSION
Caroli's disease, a congenital cystic dilatation of the hepatic ducts, has been reported steadily wordwide since the first report in 1958 by Caroli et al.5 The incidence worldwide is 1 case per million, and most patients are diagnosed before the age of 30 years.6 It is clinically complicated with recurrent cholangitis, intrahepatic cholelithiasis, or liver abscess; cancer also can be found in 7-24% of cases.78 Caroli's disease can be divided into the diffuse type, which involves both lobes, and the localized type, which occurs in a single lobe. Most cases are the diffuse type in which the intrahepatic bile ducts are dilated in both lobes. Liver fibrosis is found more frequently in the diffuse type than in the localized type, and such fibrosis is accompanied by portal hypertension, which is known as Caroli's syndrome. Caroli's syndrome is mostly comorbid with cystic kidney diseases such as polycystic kidney disease and medullary cystic kidney disease.91011 The primary treatment of Caroli's disease is surgery such as segmentectomy, lobectomy, or hepaticojejunostomy, determined by the range of cystic formation. Because the diffuse type is mostly inoperable, these patients are usually treated conservatively with antimicrobial and ursodeoxycholic acid administration and stone removal or bile duct drainage with endoscopic retrograde cholangiopancreatography if there is intrahepatic cholelithiasis.12 In contrast, in localized Caroli's disease, cure is possible with lobectomy; therefore, many domestic and foreign reports exist.1314
To our knowledge, there are 6 cases of localized Caroli's disease, including our case in Korea (Table 1),1415161718 and among them, this is the second case that was treated with segmentectomy. In addition, considering the location, 5 cases including our case involved the right lobe and only 1 of 6 total cases of localized Caroli's disease reported in Korea involved the left lobe. The foreign case reports of localized Caroli's disease differ. In one study, the disease affected the left lobe in 75-89% of cases,19 and another study presented similar rates between right and left lobes.20 However, most cases in domestic studies involved the right lobe.
In this case, segmentectomy alone was effective treatment because the lesion size of the bile duct dilatation was small. Although abdominal CT and abdominal MRI were performed before resection, Caroli's disease was not suspected because the lesion of the localized bile duct dilatation was smaller than the lesions in other reported cases, and the incidence of localized Caroli's disease is low. Irregular tubular structure and presence of tiny dots with strong contrast enhancement within the dilated intrahepatic bile ducts (the "central dot" sign) shown in CT scan or localized tubular cystic lesion seen in brightly high signal intensity in MRI T2-weighted image accompanied with communication between biliary tree in MRCP is considered very suggestive finding of Caroli's disease. However, in present case we could not find those evidences of Caroli's disease. Although mass lesion suggesting IPNB or obstruction of bile duct with stone or parasite was not found, surgery was performed because it was possible that malignancy could not be visualized between image cuts. We incidentally diagnosed Caroli's disease by a histopathological examination performed after resection for suspected IPNB or parasite infestation and thus, treated the asymptomatic Caroli's disease. Optimal management of patients with Caroli's disease is debatable,12 especially in the localized pure form of Caroli's disease, as in the present case. Some may argue that if localized Caroli's disease was suspected, the surgery should not have been performed, as our patient was asymptomatic and had no complications such as hepatic fibrosis, biliary lithiasis, cholangitis, or liver abscesses. However, considering that IPNB, which is potentially malignant, cannot be ruled out with imaging studies, and liver biopsy was unnecessary since only focal dilatation of the bile duct with no mass lesion was noted, liver segmentectomy was considered the best choice in our situation.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




