A case of obstructive jaundice caused by tuberculous lymphadenitis: A literature review
Article information
Abstract
Obstructive jaundice caused by tuberculous lymphadenitis is a rare manifestation of tuberculosis (TB), with 15 cases having been reported in Korea. We experienced a case of obstructive jaundice caused by pericholedochal tuberculous lymphadenitis in a 30-year-old man. The patient's initial serum total bilirubin level was 21.1 mg/dL. Abdominal computed tomography revealed narrowing of the bile duct by a conglomerated soft-tissue mass involving the main portal vein. Abrupt obstruction of the common bile duct was observed on cholangiography. Pathologic analysis of a ultrasonography-guided biopsy sample revealed chronic granulomatous inflammation, and an endoscopic examination revealed esophageal varices and active duodenal ulceration, the pathology of which was chronic noncaseating granulomatous inflammation. Hepaticojejunostomy was performed and pathologic analysis of the conglomerated soft-tissue mass revealed chronic granulomatous inflammation with caseation of the lymph nodes. Tuberculous lymphadenitis should be considered in patients presenting with obstructive jaundice in an endemic area.
INTRODUCTION
Tuberculosis (TB) is an infectious disease that is prevalent worldwide, but obstructive jaundice secondary to abdominal TB remains rare.1 Patients with bile duct involvement of TB causing obstructive jaundice have protracted symptoms such as malaise, jaundice, and weight loss, which are indistinguishable from those of cholangiocarcinoma.2 Obstructive jaundice can be caused by tuberculous enlargement of the head of the pancreas, tuberculous lymphadenitis, tuberculous stricture of the biliary tree, or a tuberculous mass of the retroperitoneum.1 Fifteen cases of pericholedocal tuberculous lymphadenitis were reported in Korea.3,4,5,6,7,8,9,10,11,12,13,14,15,16,17 There were two cases of pericholedocal tuberculous lymphadenitis with duodenal TB10,14 and two cases of pericholedocal tuberculous lymphadenitis with portal hypertension.11,13 This is the first case report of pericholedocal tuberculous lymphadenitis with portal hypertension concomitant with duodenal TB in Korea. Here we report a case of obstructive jaundice with portal hypertension caused by pericholedochal tuberculous lymphadenitis with duodenal TB in addition to a review of tuberculous lymphadenitis in Korea.
CASE
A 30-year-old man admitted our hospital due to jaundice. One year ago, he had been diagnosed with pulmonary TB that he had completed a six-month regimen of anti-TB medication (isoniazid, rifampicin, etambutol and pyrazinamide for 2 months, then continuing with isoniazid, rifampicin and ethambutol for the remaining 4 months) at local clinic. After treatment, he had no other problems until the development of jaundice. Abdominal ultrasonography performed at a local clinic which showed bile duct dilatation. The patient was referred to our hospital for evaluation of the biliary obstruction.
On physical examination, the patient's sclera was icteric. There was no hepatomegaly, splenomegaly or ascites. Hemoglobin was 10.7 g/dL, platelets were 227,000/µL, and white blood cell count was 9300/µL. The serum total bilirubin was 21.1 mg/dL and direct bilirubin was 12.4 mg/dL. AST was 160 IU/L and ALT was 147 IU/L. Serum BUN, creatinine, amylase and lipase levels were within normal range. Viral marker assays were negative for hepatitis B surface antigen, IgM anti-hepatitis A and anti-hepatitis C virus. Dynamic computed tomography (CT) showed both intrahepatic duct and extrahepatic bile duct dilation with abrupt narrowing of the proximal common bile duct (CBD). The proximal CBD was encased by a soft tissue mass (Fig. 1A, 1B). This lesion spread from the hepatic hilum to the hepatoduodenal ligament and pancreatic head. Central calcification was observed in the lesion and the main portal vein was encased by soft tissue mass. The patient's chest X-ray showed patchy and fibrotic opacities in both upper lungs with volume decrease. High-resolution chest CT showed multiple nodules with calcification and fibrotic bands in both upper lobes and the superior segment of both lower lobes considered stable TB (Fig. 1C). The cholangiogram from percutaneous transhepatic biliary drainage (PTBD) showed abrupt proximal CBD obstruction with dilated intrahepatic ducts (Fig. 1D). The guide wire and catheter were not passed through the narrowed segment.
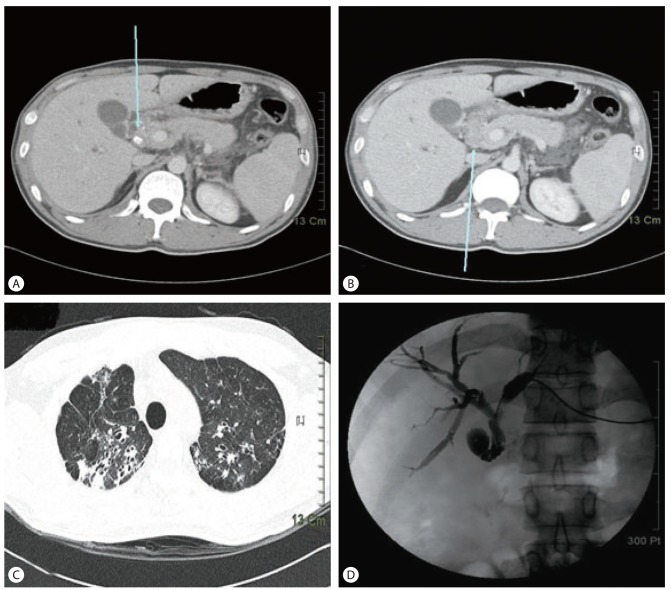
Liver and chest computed tomography (CT) images and cholangiogram via percutaneous transhepatic biliary drainage catheter. (A, B) Liver dynamic CT showing the main portal vein encased by a soft-tissue mass (arrow), which had spread from the hepatic hilum (A) to the pancreatic head (B). Calcifications were observed within the soft-tissue mass (arrow in A). (C) High-resolution chest CT showing multiple nodules in both upper lobes with calcification and fibrotic bands. Traction bronchiectasis is also seen. (D) Cholangiogram showing abrupt common bile duct (CBD) obstruction with a dilated intrahepatic duct.
Upper gastrointestinal endoscopy revealed grade 1 esophageal varices (Fig. 2A) and active duodenal ulceration was noted at the bulb (Fig. 2B). Pathologic examination of the duodenal ulceration showed chronic non-caseating granulomatous inflammation (Fig. 2C, 2D). TB polymerase chain reaction (TB-PCR) and acid fast bacillus (AFB) stain were all negative.
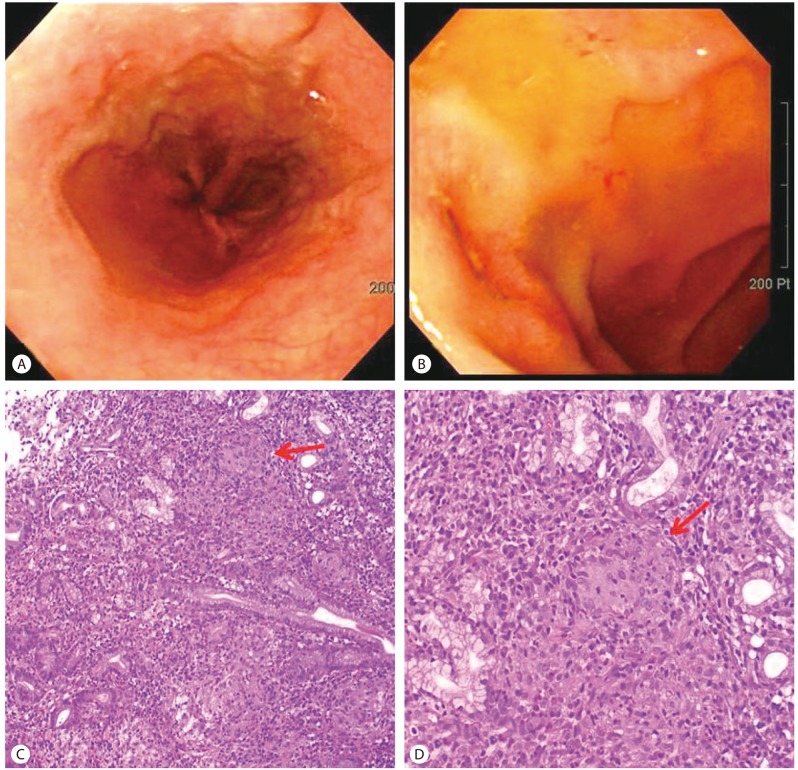
Upper gastrointestinal endoscopic findings and pathology of the duodenal ulcer. (A, B) Endoscopic examination showing esophageal varices (A) and a duodenal ulcer at the bulb (B). (C, D) Pathologic examination of the duodenal ulcer showing noncaseating granulomatous inflammation with a multinucleated giant cell [arrow; hematoxylin and eosin (H&E) stain; C, ×100; D, ×200].
Percutaneous ultrasonography-guided biopsy of the soft tissue mass was performed and pathologic examination showed chronic granulomatous inflammation with fibrosis (Fig. 3A). TB-PCR was negative and AFB and periodic acid Schiff stains did not demonstrate acid-fast bacilli or fungal organisms. Bacteria and Mycobacterium tuberculosis (M. tuberculosis) were not identified in blood and bile fluid from PTBD. The soft tissue mass was considered to be conglomerated lymph nodes or a true mass lesion. Drug sensitivity test for M. tuberculosis could not be performed because of no growth of the organism.
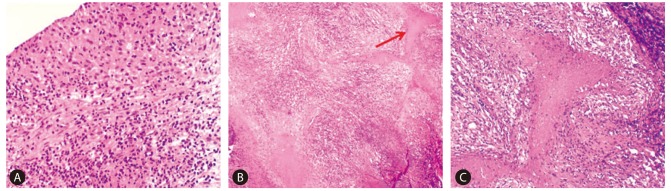
Pathology of a percutaneous ultrasonography-guided biopsy sample of the soft-tissue mass encasing the proximal CBD. Pathologic findings of a percutaneous ultrasonography-guided biopsy sample of a soft-tissue mass encasing the proximal CBD showing chronic granulomatous inflammation with fibrosis (H&E stain; A, ×200), and a caseating granuloma (arrow; H&E stain; B, ×40; C, ×200).
An explorative laparotomy was performed to relieve the biliary obstruction and to exclude malignancy. Several conglomerated lymph nodes encasing CBD and portal vein were observed during surgery. The pancreas and liver appeared grossly normal and the gallbladder was not distended. Examination of frozen sections of the conglomerated lymph nodes showed chronic ill-defined granulomatous inflammation and fibrosis. Cholecystectomy and a Roux-en-Y bypass hepaticojejunostomy were performed. Final pathologic examination showed chronic granulomatous inflammation of the lymph nodes with caseation (Fig. 3B, 3C). AFB staining did not identify acid-fast bacilli in the gallbladder, bile duct or lymph nodes. TB-PCR showed positive band in lymph nodes. After the operation, total bilirubin level decreased to 3.2 mg/dL. The patient was treated with anti-TB medication and bilirubin level had decreased to normal six weeks after surgery.
DISCUSSION
TB of the biliary system is rare and difficult to diagnose.2 Obstructive jaundice caused by tuberculous lymphadenitis is most often attributed to mechanical obstruction of the biliary tract by lymph nodes or mass lesions.1 Patients with tuberculous lymphadenitis usually present with obstructive jaundice, which may be confused with hepatobiliary malignancies.2 The annual incidence of hepatobiliary TB is reported as 1.05% of all TB infections.18
Hepatobiliary TB is caused by two mechanisms.19 The first mechanism is the direct spread of caseous materials from the portal tracts into the bile duct and the second is secondary inflammation related to tuberculous periportal adenitis.19
Table 1 lists pericholedocal tuberculous lymphadenitis reported in Korea including this case.3,4,5,6,7,8,9,10,11,12,13,14,15,16,17 Pericholedocal tuberculous lymphadenitis in Korea showed a 81.3% male preponderance. The initial total bilirubin level ranged from 0.5 to 21.1 mg/dL with a mean of 5.9 mg/dL. Including the present case, 11 cases were treated by surgery with anti-TB medication and five cases were treated by anti-TB medication alone or anti-TB medication with endoscopic nasobiliary drainage or prednisolone.9,12,14,15,17 In Korea, pericholedocal tuberculous lymphadenitis has been associated with intestinal TB (31.3%), pulmonary TB (25%), mediastinal tuberculous lymphadenitis (6.3%), cervical tuberculous lymphadenitis (6.3%) and tuberculous meningitis (6.3%) (Table 1).
Anti-TB medication without surgical intervention is desirable, but there are two emerging problems.2 First, multi-drug resistant strains of M. tuberculosis are becoming increasingly prevalent. Second, the bile duct can be severely damaged by repeated inflammatory reactions and may thus be irreversibly scarred.20 In this case, the conglomerated lymph nodes encased the main portal vein and this resulted in portal vein hypertension, thus causing the esophageal varices. In Korea, there were two previous reports of portal hypertension associated with portal vein obstruction by pericholedocal tuberculous lymphadenitis.11,13 Including the present case, all three cases of pericholedocal tuberculous lymphadenitis with portal hypertension were treated by surgical intervention. In this case, surgery was performed to relieve the tight obstruction of the CBD duct and to exclude malignancy.
Considering the worldwide prevalence of TB, tuberculous lymphadenitis is likely to be encountered. Pericholedocal tuberculous lymphadenitis needs to be considered in patients presenting with biliary obstruction, particularly in patients with risk factors such as the history of TB in endemic area.
Notes
The authors have no conflicts to disclose.
Abbreviations
AFB
acid-fast bacillus
AST
aspartate aminotransferase
ALT
alanine aminotransferase
BUN
blood urea nitrogen
CBD
common bile duct
CT
computed tomography
PCR
polymerase chain reaction
M. tuberculosis
Mycobacterium tuberculosis
PTBD
percutaneous transhepatic biliary drainage
TB
Tuberculosis
