KASL clinical practice guidelines: Management of nonalcoholic fatty liver disease
Article information
PREAMBLE
Until recently, the major causes of end-stage liver disease in Korea were chronic hepatitis B virus (HBV) and chronic hepatitis C virus (HCV) infections and alcoholic liver disease. However, hepatitis B vaccinations and antiviral drugs are anticipated to significantly reduce end-stage liver disease caused by hepatitis viruses. In contrast, the incidence of obesity-related metabolic syndrome has rapidly increased in Korea, resulting in a high prevalence of nonalcoholic fatty liver disease (NAFLD), ranging from 16-33%. NAFLD had not received much attention in the past because of its relatively favorable clinical progress. However, it has received increased attention since NAFLD was identified to progress in some patients to end-stage liver diseases, such as cirrhosis and hepatocellular carcinoma. For this reason, the epidemiology, diagnosis, and treatment of NAFLD have been proactively investigated in recent years. However, clinical practice guidelines for the diagnosis and treatment of NAFLD have not been established in Korea. This need prompted the Korean Association for the Study of the Liver (KASL) to develop the "KASL Clinical Practice Guidelines for the Management of Nonalcoholic Fatty Liver Disease", based on a systematic approach that reflects evidence-based medicine and expert opinions.
Target population
Patients diagnosed with NAFLD based on clinical, biochemical, radiological, or pathological findings, without significant alcohol consumption or liver diseases, including viral hepatitis, were primarily involved in the development of these guidelines. These guidelines were also based on pediatric and adolescent patients with NAFLD with unique findings that distinguish these cases from adult NAFLD.
Intended users
The aim of these guidelines is to provide useful clinical information and direction to healthcare providers involved in the diagnosis and treatment of NAFLD patients. Moreover, these guidelines are intended to provide definite and practical information to resident physicians, practitioners, and trainers.
Developer and funding information
The Clinical Practice Guideline Committee for the Management of NAFLD (Committee) was organized in accordance with the proposals and approval of the KASL Board of Executives, consisting of ten gastroenterologists and two pediatricians specializing in hepatology. All expenses were paid by KASL. Each committee member collected and analyzed the source data in his or her own field, and the members then wrote the manuscript together.
Evidence collection
The committee systematically collected and reviewed the international and domestic literature published in PubMed, MEDLINE, KoreaMed, and other databases. The literature was limited to research papers published in the English and Korean languages. The keywords used were 'nonalcoholic fatty liver disease', 'nonalcoholic fatty liver', 'nonalcoholic steatohepatitis', 'fatty liver', 'hepatic steatosis', and 'steatohepatitis'. In addition, specific key words related to clinical questions were included.
Levels of evidence and grades of recommendations
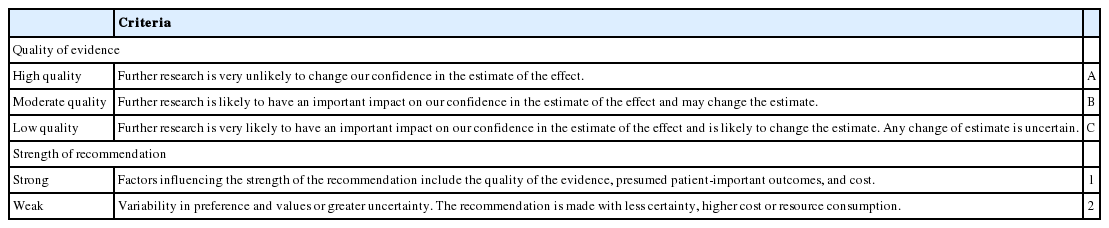
The literature gathered for data collection was analyzed by a systematic review, and the quality of evidence was classified based on the modified GRADE System (Grading of Recommendations, Assessment, Development and Evaluation) (Table 1). According to the types of studies, randomized, controlled studies were approached from a high level of evidence, while observational studies were approached from a low level of evidence. Subsequently, the level of evidence basis sets in corresponding studies was elevated or lowered by accounting for the factors influencing the quality of the studies. Through follow-up studies, the level of evidence was defined as follows: A, indicating the highest level of evidence with the smallest possibility of any changes in the conclusion; B, indicating a moderate level of potential changes; and C, indicating the lowest level of evidence with the greatest possibility of any changes.
The strength of a recommendation was suggested according to the GRADE system. In addition to the level of evidence, the results of studies were considered based on aspects of clinical multipliers and socio-economic factors, such as cost. Grading of the recommendations was performed as follows: 1, strong recommendation, or 2, weak recommendation.
A strong recommendation indicated, for example, that the interventions could be applied in most patients with strong certainty, there was a greater possibility of desirable effects, and there was high-quality evidence, as well as presumed patient-important outcomes, cost-effectiveness, preference, and compliance. A weak recommendation indicated a suggestion made with less certainty but that could be considered favorable for many patients. Alternative interventions could be chosen for "weak recommendations", according to cost and the preferences of the patients or medical practitioners.
These Clinical Practice Guidelines for the Management of NAFLD have been developed based on reviews of medical experts to be used practically for treatment, research, and education. These recommendations are not absolute standards for treatment, and adoption of these guidelines in clinical practice may differ for individual patients.
List of key questions
The committee considered the following clinical questions as key components to be covered in these guidelines.
What is the definition of and what are diagnostic tests for NAFLD?
Can NAFLD progress to end-stage liver disease?
What are the conditions associated with NAFLD and the major causes of death in patients with NAFLD?
What are the prognostic tests that could forecast the presence of fibrosis or steatohepatitis in patients with NAFLD?
Can lifestyle modification improve NAFLD?
What are the drugs that alleviate NASH?
What is the role of bariatric surgery in NAFLD patients?
What are the characteristics of NAFLD that occurs in children and adolescents?
What are the considerations for the treatment of pediatric and adolescent NAFLD patients?
Review of the manuscript and approval process
Manuscripts written by the committee members were reviewed and approved through meetings of the committee. The quality of manuscripts was evaluated based on the integrity of the contents and on the standards of AGREE II (Appraisal of Guidelines for Research and Evaluation II). The guidelines were reviewed at a meeting of an external review board, consisting of 11 specialists in the field of hepatology, and at a symposium open to all KASL members, and it was further modified prior to publication. The final manuscript was endorsed by the Board of Executives of KASL.
Release of the guidelines and plan for updates
The Korean version of the KASL Clinical Practice Guideline for the Management of NAFLD was released and published in August 2013 on the KASL Web site (http://www.kasl.org). Updates are planned when new reliable evidence is accumulated. Detailed plans for updates will be posted on the KASL Web site.
DEFINITION
Definition of NAFLD
NAFLD is a condition characterized by the findings of fat infiltration of the liver on radiological exams or biopsy, without significant alcohol intake, medication intake causing fatty liver, or other causes. NAFLD is a generic term encompassing a spectrum of nonalcoholic fatty liver (NAFL), nonalcoholic steatohepatitis (NASH), and NASH cirrhosis (Table 2).
Definition of significant alcohol consumption in NAFLD
The significant safe limits of daily alcohol intake that distinguish NAFLD from alcoholic fatty liver disease range from 10-40 g (pure alcohol), and this range varies between studies. For these reasons, definite criteria are difficult to recommend. The agreed recommendation of America1 and the Clinical Practice Guideline of the Italian and the American Association for the Study of Liver Disease (AASLD)2,3 have defined the amount of significant alcohol consumption as weekly alcohol consumption exceeding 210 g in men and 140 g in women for the previous 2 years. No ethnic differences have been reported regarding safe alcohol limits not resulting in liver damage. The KASL Clinical Practice Guideline for NAFLD uses the amount of significant alcohol consumption stated above in clinical treatment and in studies for international comparison with the results of future studies.
EPIDEMIOLOGY
Incidence and prevalence of NAFLD
Only a limited number of studies on the incidence of NAFLD have been performed.4-7 The annual incidence of NAFLD was approximately 86 cases per 1,000 persons in a study performed in Japan.4 In contrast, the annual incidence was considerably lower, at approximately 29 cases per 100,000 persons, in a study performed in the UK.6 According to a 5-year retrospective cohort study performed domestically in health screening examinees, the annual incidence was approximately 26 cases per 1,000 persons.7
The prevalence of NAFLD has varied according to the study subjects, diagnostic standards, and definition of NAFLD. In a domestic study in 589 living liver donors, histological findings revealed that the prevalence of NAFLD was 51%.8 Histological findings revealed that the prevalences of NAFL and NASH were 46% and 12.2%, respectively, in a large-scale study performed in middle-aged Americans.9 In a large-scale cohort study from the Framingham Heart Study, using computed tomography (CT), a diagnostic standard, revealed that the prevalence of NAFLD was 17%.10 According to a study performed in a demographic group of ordinary people participating in the National Health and Nutrition Examination Survey III, the prevalences of NAFLD and advanced fibrosis were 34% and 3.2%, respectively, based on ultrasonography scans, which are used as a diagnostic standard.11 In summary, the prevalences of NAFLD and NASH have been estimated to range from approximately 6-35% (median: 20%) and 3-5%, respectively. In a few domestic studies performed in health screening examinees diagnosed by ultrasonography, the prevalence of NAFLD ranged from 16-33%.12-14
Risk factors for NAFLD (Table 3)
NAFLD shows profound correlations with obesity, type 2 diabetes, dyslipidemia, metabolic syndrome, and other conditions. According to a study in severely obese patients who underwent bariatric surgery, the prevalences of NAFLD and steatohepatitis were 91% and 37%, respectively.15 The prevalence of NAFLD was found to be 69% in patients with type 2 diabetes in a recent study.16 Moreover, NAFLD was identified as an independent risk factor for the occurrence of type 2 diabetes in Korean men in a cohort study.17 According to a study on the relationship of NAFLD with hypothyroidism, the prevalence of NAFLD was 19.5% when thyroid function was normal. In contrast, the prevalence of NAFLD was significantly greater in patients with hypothyroidism, at 30.2%.18 Meanwhile, an association between polycystic ovary syndrome (PCOS) and NAFLD was suggested.19 The prevalences of NAFLD were 19% in the control group and 41% in patients with PCOS.20 Other risk factors for and conditions associated with NAFLD include obstructive sleep apnea syndrome, hypopituitarism, and hypogonadism.21
Natural history of NAFLD
Most follow-up studies on histological changes in NAFLD have had limitations of small sample sizes and insufficient follow-up durations. NAFL has often shown favorable outcomes; in contrast, NASH has been recognized to progress to end-stage liver diseases, such as cirrhosis or hepatocellular carcinoma.21,24-27 The natural history of NAFLD can be summarized as follows:28-39 1) the overall mortality rate is higher in NAFLD patient groups than in normal control groups; 2) the most common cause of death is cardiovascular disease; and 3) the liver-related mortality rate increases in patients with NASH.
According to some cohort studies in patients with NAFL and NASH, the rate of progression to cirrhosis varies.28-37 In a cohort study in 420 NAFLD patients followed up for 7.6 years, the incidence of cirrhosis was 3% for all of the subjects.28 The incidences of cirrhosis were 0.9% in a study of 109 NAFL patients followed up for 16.7 years30 and 1.2% in a study of 170 NAFL patients followed up for 20.4 years.32 The incidence of cirrhosis is relatively higher in patients diagnosed with NASH, based on liver biopsy, compared with that in patients diagnosed with NAFL. In a cohort study of 71 patients with NASH followed up for 13.7 years, 10% of the patients progressed to end-stage liver disease.29
Other evidence of the progression of NASH to cirrhosis includes the frequent association of metabolic risk factors for NASH, including type 2 diabetes, obesity, or metabolic syndrome, with cryptogenic cirrhosis. This association implies that NASH is likely to be the principal preceding disease of cryptogenic cirrhosis.39,40 Some prospective studies compared the natural history of cirrhosis progressing from NASH and from HCV infection, and the authors concluded that decompensation rates and overall mortality rates were lower in patients with NASH cirrhosis.41-43 In a multinational cohort study recently performed in 247 NAFLD patients with advanced fibrosis or cirrhosis, the overall mortality rates were similar in both groups of patients with cirrhosis induced by NASH and by the HCV.39 The annual cumulative incidence of hepatocellular carcinoma was estimated to be 2.6% in patients with NASH cirrhosis, which was 2- to 3-fold lower than that in patients with cirrhosis induced by the HCV. Hepatocellular carcinoma mainly develops in patients with advanced fibrosis or cirrhosis, and it is rarely observed in patients without either disease. Although the exact mechanism remains unclear, the risk factors for carcinogenesis are assumed to include old age, type 2 diabetes, and obesity.27,41
NAFLD-related diseases (comorbidities)
Because various metabolic diseases have frequently been associated with NAFLD, the high mortality rate associated with NAFLD is thought to be attributable to cardiovascular disease. However, several recent studies have verified that NAFLD itself is an independent risk factor for various metabolic diseases.44,45 According to a study of 2,839 patients with type 2 diabetes, patients with NAFLD showed a higher prevalence of cardiovascular disease than patients without type 2 diabetes (26.6% vs. 18.3%).45 In another study in 250 patients with type 1 diabetes, the prevalence of cardiovascular diseases was higher in patients with NAFLD (10.8% vs. 1.1%).46 In large-scale cohort studies performed in healthy individuals, the risk of cardiovascular disease was higher in patients with NAFLD than in healthy individuals without it.47-51 According to a meta-analysis performed on the above-mentioned studies, the odds ratio for the association of NAFLD with cardiovascular diseases was 2.05 (95% CI 1.81-2.31).24
As shown in previously performed large-scale cohort studies, the risk of type 2 diabetes was higher in patients with NAFLD, and this condition became more distinctive in patients with NASH.17,52,53 Additional studies are essential to further investigate whether the presence of NAFLD could be a prognostic factor for predicting the incidences of cardiovascular and metabolic diseases, such as type 2 diabetes.
DIAGNOSIS
Diagnosis of and screening for NAFLD
For the diagnosis of NAFLD, it is important to exclude other causes of liver disease and to examine the liver for fatty changes. Therefore, in cases that are clinically suspicious for chronic liver diseases or that have abnormal findings on liver function tests, medical history taking and serological testing must be performed to exclude critical causes of chronic liver disease in Korea, such as chronic hepatitis virus B or C infection, alcoholic liver diseases, drug-induced liver diseases, autoimmune liver diseases, and Wilson's disease. In addition, abdominal ultrasonography can be performed to assess the liver for steatosis. In cases of a lack of abnormal findings on liver function tests, which patients should be candidates for NAFLD screening? There is currently no consensus on the answer to this question. Insulin resistance is known to be a critical risk factor for the incidence of NAFLD. However, performing a screening test remains controversial for identifying the presence of NAFLD in patients with metabolic syndrome, in whom insulin resistance plays a crucial role in NAFLD pathogenesis. The 2009 Special Conference of the European Association for the Study of the Liver recommended blood tests and abdominal ultrasonography for NAFLD in patients who present with insulin resistance and related diseases, because they are likely to have NASH.54 However, in the 2012 Clinical Practice Guideline of AASLD, these examinations were not recommended because the diagnosis and treatment of NAFLD remained unclear and the long-term benefit and cost-effectiveness of screening tests had not been clarified.3 The importance of performing screening tests on family members of patients with NAFLD has also been unclear until now. According to one report, NASH occurred in 18% of the brothers/sisters of patients with NAFLD.55 According to another study, fatty liver disease was observed in 59% of siblings and 78% of parents of overweight children with NAFLD. In contrast, NAFLD was detected in 17% of siblings and 37% of parents of overweight children without NAFLD. Therefore, the probability of having NAFLD is significantly higher among the family members of overweight children with NAFLD.56 Similarly, some studies with a small sample size have reported that NAFLD is significantly correlated with family history and genetic predisposition. However, a study of twins failed to show a significant relationship between genetic factors and the presence of NAFLD.57
Several types of NAFLD screening tests have been developed. However, to date, there is no established screening test. In general, liver function tests, such as AST and ALT, and abdominal sonography have commonly been performed. Because liver function test results can be normal in patients with NAFL or NASH, liver function tests have low sensitivity as screening tests. Abdominal ultrasonography has a higher sensitivity, but this examination has the disadvantage of high cost. Other tests, such as serum ferritin and uric acid testing, have been studied for screening, but further studies are necessary to evaluate the efficacy of these tests.58,59
In actual clinical practice, fatty liver disease can be incidentally detected in abdominal imaging performed as examinations for other disorders or for regular check-ups. However, in these cases, only a small number of studies have investigated additional tests to be performed for the evaluation of liver disease or associated conditions. When abnormal findings are detected by liver function tests, the patient's alcohol and drug history must be identified, and tests must be performed to exclude other liver diseases to achieve an accurate diagnosis. When liver function test results are normal, the need for a screening test to identify the presence of other associated conditions is uncertain. In a recently performed prospective cohort study of NAFLD patients undergoing screening, the risk of metabolic syndrome increased with the degree of fatty changes in the liver.60 Another study reported that increased ALT levels and fatty changes on abdominal ultrasonography were risk factors for the incidence of type 2 diabetes.61 In addition, NAFLD had a significant relationship with the degree of coronary artery calcification, which is a strong risk factor for ischemic heart disease. Therefore, NAFLD was an independent risk factor for coronary artery disease.62 The point to consider when deciding whether to perform screening tests for NAFLD-associated disorders is that, unlike the case for NAFLD, there are therapeutic methods that are effective in preventing the progression of metabolic diseases and their complications. Therefore, screening for metabolic syndrome, type 2 diabetes, coronary artery disease, and other diseases could be considered in cases of incidental detection of fatty changes upon radiological evaluation of the liver.
[Recommendation]
1. When liver function tests reveal an increase in AST or ALT, medical history taking and examinations are essential for distinguishing muscular and liver diseases, including viral hepatitis, alcohol liver diseases, drug-induced hepatitis, autoimmune liver diseases, and Wilson's disease, in the diagnosis of NAFLD, and abdominal ultrasonography can be performed primarily to assess the steatosis of the liver. (B1)
Non-invasive testing in NASH and advanced fibrosis
Because significant differences can be found in the prognosis of NAFLD, depending on the histological findings, confirmation of the presence of steatohepatitis or fibrosis is clinically crucial. Currently, liver biopsy is the standard test for identifying hepatic inflammation and fibrosis. However, liver biopsy has some limitations, such as high cost, invasiveness, risk of complications, and intra- and inter-observer variability in its interpretation. Additionally, liver biopsy yields insufficient amounts of collected liver tissue to represent the entire condition of the liver.63,64 For these reasons, many studies have been undertaken to determine a non-invasive method for estimating the histological severity of NAFLD instead of liver biopsy, mainly in the field of radiological and biochemical testing.
Radiological examination
Abdominal ultrasonography is commonly used in the screening of asymptomatic patients with abnormal findings on liver function tests. However, this examination is subjective, and its diagnostic sensitivity is less than 70% when the amount of fat in the liver is less than 30%. Moreover, the testing does not distinguish NAFL from NASH.65,66 CT has high specificity but low sensitivity for evaluating the amount of fat in the liver. Magnetic resonance imaging (MRI) is known to be more favorable than ultrasonography in assessing small degrees of fatty infiltration.67-69 Magnetic resonance spectroscopy (MRS) can very precisely measure the amount of triglycerides in the liver. However, these expensive tests are also limited in distinguishing NAFL from NASH.67,70
Transient elastography
Several studies using transient elastography (TE, Fibroscan®) to evaluate fibrosis have been performed in NAFLD patients.71 In a recent meta-analysis, TE showed high sensitivity and specificity in the assessment of hepatic fibrosis in NAFLD. However, in cases of obesity (body mass index [BMI] ≥30 kg/m2), which commonly occurs in patients with NAFLD, the accuracy of TE decreased, and performance of the test may not be possible in some cases (5-13%).24 The recently introduced Controlled Attenuation Parameter (CAP) is known to relatively accurately evaluate the degree of fatty infiltration, and a large number of clinical studies are anticipated to report meaningful results.72-74
Magnetic resonance elastography
The recently developed magnetic resonance elastography (MRE) technique, which has only utilized in a few studies, was demonstrated to be useful in distinguishing between NAFL, NASH, and fibrosis.75 Unlike TE, MRE enables the assessment of the entire liver; it has no observer dependency; and it can be performed in obese patients.76 However, this technique is expensive and cannot yet be regularly used in all medical institutions.
Biochemical panels
Many biochemical markers and their combination panels have been developed and proposed. However, the diagnostic ability of most of these tests has been insufficiently verified, so tests that have been validated by several studies are introduced in this section. AST, ALT, and the AST/ALT ratio are the most commonly used in clinical practice. However, these liver function tests alone do not accurately reflect the degree of fibrosis or inflammation in the liver, or the effects of treatment.77-79
The NAFLD Fibrosis Score (NFS) is the most widely studied among biochemical panels. It consists of six parameters (age, BMI, diabetes/impaired glucose tolerance, platelet count, albumin level, and AST/ALT ratio), which can be measured clinically or biochemically, and can be calculated easily on a Web site (http://nafldscore.com). The NFS has two cut-off values used to evaluate liver fibrosis, namely, <-1.455 (low probability) and >+0.676 (high probability). According to a meta-analysis of 13 studies performed in 3,064 patients,24,25,80-91 NFS showed a high area under the receiver operating characteristic curve (AUROC) value of 0.85 in diagnosing liver fibrosis worse than stage F3. Taking <-1.455 as a cut-off, the sensitivity was 90% and the specificity was 60% in excluding advanced liver fibrosis. Using >+0.676 as the cut-off, the sensitivity was 67% and the specificity was 97% in diagnosing advanced liver fibrosis. Moreover, NFS has been verified in patients with various clinical conditions and demographics (e.g., ethnicity, BMI, and DM), and it is simple and cost-effective to perform. In an investigation in Korean patients with relatively lower BMIs than Western people, similar diagnostic ability was shown, in agreement with the results of international studies.92 However, approximately 20-58% of patients exhibited values between the two cut-off values (intermediate probability); thus, in these cases, liver biopsy had to be considered.24
The Enhanced Liver Fibrosis (ELF) test, which measures three liver fibrosis-related matrix proteins (hyaluronic acid, tissue inhibitor of metalloproteinase 1, and aminoterminal peptide of procollagen III), recently underwent an evaluation of its usefulness in the estimation of various causes of liver fibrosis in many European studies. One study reported favorable results, with an AUROC of 0.90, sensitivity of 80%, and specificity of 90% for advanced liver fibrosis, but this test must be investigated further.83 A cytokeratin-18 fragment in plasma indicated apoptosis of liver cells and was a marker for NASH.24,93 Plasma cytokeratin-18 fragment levels increased significantly in patients with steatohepatitis compared with normal subjects or patients with simple fatty liver.94 Assessment of cytokeratin-18 fragment levels showed potential as a screening test for NASH with favorable results (sensitivity of 78%, specificity of 87%, AUROC of 0.82) in a meta-analysis.24 However, this marker is currently unavailable in clinical practice, and the standard cut-off value for diagnosis must also be established.
In summary, the non-invasive tests described above have shown promising results. However, further studies must be performed on their availability and usefulness in the assessment of disease progression and treatment response.
[Recommendations]
2. Ultrasonography, CT, MRI, and MRS could be helpful in the evaluation of the amount of fat in the liver. However, these tests are not helpful for distinguishing NAFL from NASH. (A1)
3. NAFLD fibrosis score, transient elastography, and magnetic resonance elastography could be helpful in the estimation of advanced liver fibrosis in NAFLD. (B1)
Liver biopsy
Non-invasive tests can be helpful in the detection of advanced fibrosis or steatohepatitis; however, liver biopsy remains the gold standard for diagnosing NAFLD. Biopsy enables the evaluation of the degree of liver fibrosis, the prediction of prognosis, and the provision of information essential for planning patients' treatment and management, as well as the distinction of steatohepatitis from NAFL.95,96 Furthermore, liver biopsy can be helpful in distinguishing drug-induced hepatitis, Wilson's disease, and autoimmune hepatitis, etc.97 The data from previous studies have been insufficient to clarify when liver biopsy is essential, and therefore biopsy must be performed only in cases in which it can be helpful in determining the diagnosis, treatment, and prognosis. According to previous studies, age, BMI, diabetes/impaired glucose tolerance, AST/ALT ratio, platelet count, albumin level, insulin resistance, and other factors have been identified as factors predictive of steatohepatitis or advanced fibrosis.54,80,98,99
[Recommendations]
4. Liver biopsy should be considered in cases in which NASH or advanced liver fibrosis is suspected in NAFLD patients. (B1)
5. Liver biopsy should be considered when concurrent other chronic liver diseases cannot be excluded in patients suspected of having NAFLD. (B1)
TREATMENT
Lifestyle modification
Weight reduction
A large amount of evidence suggests that lifestyle modifications, such as dietary control with or without exercise, improve NAFLD. In overweight or obese (BMI >25.0 kg/m2) NAFLD patients, dietary therapy alone or exercise along with dietary and lifestyle changes significantly reduced liver fat content, as revealed by ultrasonography,100-102 MRI,103-105 or liver biopsy.106 It was also confirmed that a 5% reduction in body weight due to exercise and diet induced a significant decrease in liver fat content,107 and a few prospective studies using MRS have also reported that weight loss was associated with a decrease in liver fat content.105,108,109 Moreover, in two randomized, controlled studies in which liver histology was evaluated before and after lifestyle modifications, weight loss of more than 7-10% was associated not only with fat infiltration reduction but also with hepatic inflammation, hepatocyte ballooning, and degeneration.110,111 However, the numbers of patients in these studies were rather small; therefore, further studies with larger sample sizes are still needed. Additionally, it remains controversial whether weight loss is associated with normalization of liver enzyme levels (AST, ALT).105,111-113 Regarding the pace of weight loss, a study showed that a weight reduction-targeted gradual decrease of a maximum of 1 kg/week of body weight improved NASH and NAFLD activity scores (NAS).114 However, a rapid decrease of more than 1.6 kg/week of body weight worsened portal inflammation and fibrosis in approximately 24% of morbidly obese patients.115 In summary, weight reduction by lifestyle modification decreases liver fat content in NAFLD patients. However, a rapid reduction in weight should be considered cautiously.115 Moreover, further studies are needed to investigate the influence of weight reduction on improvements in histological scores and enzyme levels.
[Recommendation]
6. In overweight or obese NAFLD patients, weight reduction mediated by dietary and exercise therapies decreases liver fat content. (A1) A reduction of more than 7-10% of total body weight is necessary to improve hepatic inflammation. (B2)
Dietary therapy
Reduction in the intake of total energy and control of food intake are crucial aspects of NAFLD treatment. Daily caloric intake varies according to age, gender, weight, and physical activity and should be optimally adjusted; however, on average, the daily recommended caloric intake in Korea is approximately 2,000-2,500 kcal for men and 1,700-2,000 kcal for women. The reduction in total energy intake is generally approximately 25% less than the daily recommended caloric intake.116 Thus, the amount of caloric decrease is approximately 400-500 kcal per day.
In addition to total energy intake, the macronutrient (carbohydrate, fat, protein) ratio has recently been discovered to play an important role in the development of obesity and NAFLD. Carbohydrate intake was found to be associated with metabolic syndrome and with the degree of hepatic inflammation in NAFLD patients.117,118 Interestingly, in Western patients with NAFLD, a low-carbohydrate diet was more effective in reducing liver fat content than a low-fat diet.119 The Korean National Institute of Food and Drug Safety Evaluation also reported that increased carbohydrate and fructose intake was associated with an increased prevalence of fatty liver and elevated liver enzymes.120 Furthermore, a randomized, controlled study involving 220 NAFLD patients revealed that, compared with low-fat dietary training, low-carbohydrate dietary training was more effective in reducing both liver enzymes and liver fat content in Korean patients.120 However, a randomized controlled study by Haufe et al revealed that both low-fat and low-carbohydrate diets effectively reduced liver fat content.121
Korean people maintain a relatively high carbohydrate intake compared with Western people. The greater effectiveness of low-carbohydrate diets in Korean patients is thought to be attributable to the proportion of dietary carbohydrates accounting for more than 65% and fat accounting for less than 20% of the total calorie intake. Therefore, in addition to a reduction in total energy intake, a low-carbohydrate and low-fructose diet is recommended for Korean NAFLD patients.122
[Recommendation]
7. A reduction in total energy consumption, as well as a low-carbohydrate and low-fructose diet, is recommended for NAFLD patients. (B1)
Exercise
Exercise improves both insulin resistance and metabolic disorders. The radiological findings of four studies demonstrated that exercise, without dietary therapy or weight loss, can decrease liver fat content.108,109,123,124 The exercise in the aforementioned studies was aerobic exercise, in addition to daily activity. The most common types of aerobic exercise in previous studies have included walking, running, swimming, and cycling. It was recommended to perform exercise at moderate intensity (50-70% of maximal heart rate) for 30-60 minutes more than twice per week and for at least 6 weeks.108,109,123,124 However, there is still no consensus regarding the type, intensity, or duration of exercise therapy as a treatment for NAFLD. Moreover, these studies have been insufficient in validating whether exercise therapy alone can improve hepatic inflammation.
[Recommendation]
8. Exercising for at least 30 minutes twice per week can reduce the amount of fat in the liver. (B1)
Anti-obesity medications
A study reported the effects of anti-obesity medication on weight reduction in NAFLD patients. In a small number of obese NASH patients, orlistat, a lipase inhibitor, administered for 6 months decreased body weight and improved liver enzyme levels.110 In two randomized, controlled studies using orlistat, one study showed liver enzyme and radiological liver fat content improvements in the treatment group compared with the placebo group, but the other study failed to show these improvements.125,126 Therefore, more evidence is needed before the use of anti-obesity medications can be recommended for obesity treatment in addition to correction of lifestyle habits.
Medication treatment
Antioxidants
Vitamin E (alpha-tocopherol)
Vitamin E is a powerful antioxidant that reduces inflammation in the liver by lowering oxidative stress, which causes improvement of steatohepatitis.127,128 In short-term (6 months), randomized, controlled studies with small sample sizes or pilot studies, vitamin E was effective in improving ALT, fat, and inflammation in the liver.128-132 In a recent meta-analysis, the histological findings of the liver revealed that vitamin E yielded no improvement in NASH patients.133,134 Furthermore, the administration of high-dose (more than 400 IU/day) vitamin E for long durations increased the mortality rate in another study.135 In contrast, the administration of high-dose vitamin E (800 IU/day) resulted in significant improvements in liver tissue compared with the control group in a recent large-scale, randomized, controlled trial, the PIVENS study (43% vs. 19%, P=0.001).136 Furthermore, there was no incidence of severe complications compared with the control group and the pioglitazone group resulting from long-term administration of high-dose vitamin E. In the TONIC study, a large-scale, randomized, controlled study of 173 children with NASH aged between 8 and 17 years, the effects of high-dose vitamin E (800 IU/day) and metformin (1,000 mg/day) were compared with a control group. The administration of high-dose vitamin E showed no effect on ALT compared with the control group. In contrast, the percentage of patients with alleviated NASH was significantly higher (58% vs. 28%, P=0.006). The study concluded that the administration of high-dose vitamin E was safe in children.137 A recent study proved that the previously reported risks associated with high-dose vitamin E, as revealed by meta-analyses, were due to errors in study methods.138-140 Furthermore, as shown in the PIVENS and TONIC studies, the administration of high-dose vitamin E did not increase the mortality rate in patients with NASH. However, according to the SELECT study, which compared the effects of vitamin E (400 IU/day) and selenium in 35,533 healthy men, the incidence of prostate cancer was higher in patients administered vitamin E compared with the control group (HR, 1.17; 99% CI, 1.004-1.36, P=0.008).141
Other antioxidants
There have been no randomized, controlled studies with significant results related to antioxidants other than vitamin E. Several antioxidants, such as N-acetylcysteine142 (glutathione precursor), betaine143 (agent involving glutathione storage), probucol144 (novel antihyperlipidemic agent), viusid,145 and silibinin (milk thistle)146 have been investigated in the NASH population, but it is difficult to make definitive recommendations on their use.
[Recommendation]
9. High-dose vitamin E (800 IU/day) can be used as a therapeutic agent to improve the histological findings in liver tissue in patients with NASH confirmed by biopsy. However, there are still safety concerns associated with long-term use of high-dose vitamin E. (B1)
Insulin sensitizers
Thiazolidinediones (TZDs)
TZDs (rosiglitazone, pioglitazone) are PPAR-γ agonists that improve insulin resistance in the fat tissue, muscle, and liver; improve liver cell injury; and reduce the amount of fat in the liver by promoting the secretion of adiponectin, which inhibits inflammation.147,148 In several recent randomized, controlled studies, TZDs improved ALT levels, regardless of the presence of diabetes, and they improved fatty infiltration, ballooning degeneration, lobular inflammation, and other markers of liver cell damage.136,149-152 However, improvement in liver fibrosis, an important prognostic marker of liver disease progression, was either absent or showed only a tendency.136,150-153 In the PIVENS study of 247 NASH patients without diabetes, Sanyal et al136 administered medication for 24 months by classifying subjects into a pioglitazone (30 mg/day) group, a vitamin E (800 IU/day) group, and a control group. The primary endpoint of this study was improvement in the NAS of more than two points. Effectiveness was observed in both the pioglitazone and vitamin E groups, compared with the control group, with improvements of 19% in the control group, 34% in the pioglitazone group (P=0.04 vs. control group), and 43% in the vitamin E group (P=0.001 vs. control group). In the PIVENS study, pioglitazone was not proven to be effective in improving the histological findings of the liver, as P-values of less than 0.025 were considered statistically significant in the comparison of two groups (pioglitazone vs. control group or vitamin E vs. control group).
However, the secondary outcome, the disappearance of NASH, occurred in 47% of all the subjects in the pioglitazone group, which was significantly higher than the rate in the control group of 21% (P=0.001). The most common complication of TZDs is weight gain (mean value: 4.4 kg, some differences occurred based on the durations of studies),154 and other complications include lower extremity edema, muscle cramps, fractures in cases of long-term use,155 a higher risk of bladder cancer,156 and congestive heart failure.157 In a comparative study of TZDs and other hypoglycemic agents administered to 159,026 diabetic elderly patients, rates of heart failure, acute myocardial infarction, and mortality were higher in patients treated with rosiglitazone than in patients treated with other diabetes medications. In contrast, no differences were found between patients treated with pioglitazone and the control group.158 Lincoff et al157 performed a meta-analysis of 19 studies (16,390 subjects) on the treatment of diabetes with pioglitazone. Death, myocardial infarction, and cerebral infarction were reduced in the pioglitazone group compared with the control group (who received other diabetes treatments) (4.4% vs. 5.7%, P=0.005). However, heart failure developed more frequently in the pioglitazone group than in the control group (2.3% vs. 1.8%, P=0.002). Recently, the use of rosiglitazone for treating diabetes and NASH has been suspended by the EMA (European Medicines Agency) and the KFDA (Korea Food and Drug Administration) due to the risk of complications.
Metformin
Metformin, a diabetic drug, improves insulin resistance in the liver and muscles, and it inhibits the production of fats in the liver by activating adenosine monophosphate-activated protein kinase (AMPK) within the liver. Therefore, metformin was anticipated to be beneficial in treating NASH.159,160 The drug showed efficacy in patients with NAFLD associated with diabetes, and it improved insulin resistance and normalized ALT in patients without diabetes in early studies.130,161,162 However, the drug was almost ineffective in improving findings in liver tissues.130,162 Metformin has the effect of weight loss, and its combination with TZDs, which have the effect of weight gain, has been reported to offset the shortcomings of TZDs. Thus, studies of the combined administration of these drugs are in progress.163 However, this combined administration has been reported to be ineffective in improving histological findings and insulin resistance in the liver, and it was ineffective in changing ALT levels compared with the control group in a recent randomized, controlled study and in several other studies.130,164-168 Moreover, no improvement was detected in either the normalization of ALT levels or the alleviation of histological findings, regardless of the presence of diabetes or the dose of metformin, according to a meta-analysis performed by Musso et al.169
[Recommendations]
10. Pioglitazone alleviates the ALT levels and improves hepatic fat accumulation and inflammation in patients with biopsy-proven NASH, making it possible for pioglitazone to be used as a therapeutic drug. However, the appropriate duration and dosage of the drug and complications of long-term use must be further investigated. (B1)
11. Metformin is not recommended for NASH treatment because it has shown no improvements in histological findings or ALT levels. (A1) However, this drug could be used preferentially in NAFLD patients with diabetes.
Lipid-lowering drugs
The most common cause of death in patients with NAFLD is cardiovascular disease. Thus, the use of lipid-lowering agents, such as statins (hydroxy-methyl-glutaryl coenzyme A reductase inhibitors),170 fibric acid derivatives (fibrates), niacin, ezetimibe, and n-3 polyunsaturated fatty acids (PUFA), could be considered in NAFLD patients with hyperlipidemia.171
Statins
Although elevated aminotransferase level is not uncommon in patients receiving statins, serious hepatotoxicity from statins has very rarely been seen in patients with compensated liver disease. For this reason, the use of statins is relatively safe.172 According to some studies on the effects of statins in NASH, statins improved liver function and histology in patients with NASH.173,174 The only randomized, double-blind, controlled trial of statins was published by Nelson et al,175 in which 16 patients were randomized to receive 12 months of simvastatin 40 mg daily or placebo. However, there were no improvements in steatosis, necroinflammation, or fibrosis according to the liver histology.175 This study was limited by a small sample size and mild NASH (grade 1, stage 1) at baseline in most of the patients, making it difficult to demonstrate improvement.175
Fibrates
Fibric acid derivatives, such as clofibrate, are used for the treatment of hypertriglyceridemia, hypercholesterolemia, and mixed hyperlipidemia. However, the only controlled study using 12 months of clofibrate to treat NAFLD showed no effects on liver histology or liver function.176
Omega-3 polyunsaturated fatty acid supplementation (n-3 PUFAs)
In a recently performed meta-analysis, n-3 PUFAs showed no significant effects in patients with NAFLD.177 Zhu et al178 performed a randomized, controlled study of 144 NAFLD patients with hyperlipidemia, and the treatment group received 2 g of n-3 PUFA from seal oil three times per day for 24 weeks. Consequently, PUFA supplementation significantly decreased serum ALT levels and lipid profiles and reduced liver fat (as measured by ultrasonography) compared with controls. These outcomes are, however, insufficient to be used as a standard because liver biopsy was not performed. Therefore, further comparative studies are needed to assess the efficacy of n-3 PUFAs using liver biopsy. In addition, a randomized, controlled study is crucial for standardizing the types, dosages, and durations of n-3 PUFA treatment. To summarize the above study results, n-3 PUFAs are not recommended for the treatment of NASH. However, they could be considered as therapeutic agents for hypertriglyceridemia in patients with NAFLD.
Ezetimibe
Ezetimibe is a strong inhibitor of Niemann-Pick C1-like 1 (NPC1L1) protein, which is essential for cholesterol absorption in intestinal and liver cells.179
Although there was no significant change in fibrosis, ezetimibe treatment (10 mg) in NAFLD/NASH patients with concurrent hyperlipidemia showed similar improvement in liver histology and metabolic parameters in a small pilot study and in a recent uncontrolled long-term study.180,181 These data imply the possibility of using ezetimibe for the treatment of NASH.180,181 However, large-scale, randomized, controlled studies must be performed to prove the efficacy of ezetimibe.
[Recommendations]
12. Although statins are not recommended for the specific treatment of NASH, they could be considered for reducing cardiovascular complications in NAFLD patients with hyperlipidemia. (B1)
13. Omega-3 fatty acids are not recommended for the specific treatment of NASH. However, they could be considered as medication for treating hypertriglyceridemia in patients with NAFLD. (B1)
Pentoxifylline
Pentoxifylline, as a non-selective TNF-α antagonist, has been thought to facilitate the treatment of NAFLD by reducing oxidative stress and apoptosis by inhibiting the release of TNF-α, which plays a crucial role in NASH onset.182 Furthermore, recent studies have identified that pentoxifylline prevents liver injury caused by oxidized lipid products by slowing the fat oxidation rate.183 In a pilot study of a small number of patients with NASH, pentoxifylline showed improvement in AST and ALT levels and insulin resistance.184-186 Wagner et al administered pentoxifylline for 12 months to 30 patients with NASH in a randomized, controlled study. However, no significant differences were found in the improvement of ALT levels, ballooning degeneration, or NAS compared with the control group (P=0.63, P=0.46, P=0.17).187 Recently, Zein et al performed a 12-month, randomized, controlled study in 55 patients with NASH by dividing the subjects into pentoxifylline and control groups. The percentages of patients showing improvement in the NAS, the primary evaluation criterion, by more than 2 points were 38.5% in the pentoxifylline group and 13.8% in the control group, which was a significant difference (P=0.036, intention-to-treat analysis). In a per protocol analysis, improvement in NAS was observed in 50% of the pentoxifylline group and 15.4% of the control group (P=0.001). However, no significant differences were detected in patients showing improvement in ballooning degeneration and fibrosis (P=0.60, P=0.17).188 According to two randomized, controlled studies, long-term intervention with pentoxifylline (1,200 and 400 mg, 3 times/day) resulted in no difference in the occurrence of severe complications compared with the control group.
Ursodeoxycholic acid (UDCA)
UDCA is a hepatoprotective drug, and it has been widely used in clinical practice for the treatment of acute and chronic liver disease patients with abnormal liver function tests. UDCA, a natural hydrophilic bile acid, is known for its anti-inflammatory, anti-apoptotic, and immunomodulatory properties, and it was predicted to prevent the progression of NAFLD.189 First, Lindor et al190 showed that the usual UDCA dose of 13-15 mg/kg/day was not significantly better than placebo in improving liver function or liver histology. A second study, by Dufour et al,132 compared the efficacy of the usual dose of UDCA with a combination of UDCA and vitamin E. Leuschner et al191 and Ratziu et al192 investigated the effects of high-dose UDCA (25-35 mg/kg/day) on liver biopsy results and liver enzyme levels. After treatment, a second biopsy was conducted in all of the studies, except for the study by Ratziu et al.192 This study showed uniquely significant improvement with UDCA in NASH patients but only in liver function tests due to the lack of paired biopsies. A multi-arm, comparative study by Dufour et al (UDCA/vitamin E group; UDCA group; placebo group)132 failed to show any differences in improvement of NASH with UDCA monotherapy vs. placebo. However, the combination of UDCA and vitamin E did result in normalization of AST and ALT levels and significant improvement in liver histology. Because this study's sample was too small, further large-scale studies on the treatment of NASH with combination therapy (UDCA/vitamin E) vs. vitamin E monotherapy are necessary to draw any firm conclusions.
Based on the aforementioned results, the treatment effects of the usual dose of UDCA alone in patients with NASH have not yet been proven. Further studies are needed to prove the efficacy of high-dose UDCA. Additionally, clinical trials with new UDCA derivatives may be warranted in the near future.
Angiotensin-II receptor blockers
No randomized, controlled studies have been conducted to verify the effects of different anti-hypertensive agents on the liver in patients with NAFLD. Angiotensin-II receptor blockers have been anticipated to accelerate the apoptosis of hepatic stellate cells.193 A phase III, randomized, controlled study (FELINE study) is in progress to investigate the effects of losartan on liver fibrosis in patients with NASH. The study could prove the potentially beneficial effects of ARBs in NASH.
Other drugs and the current status of new drug development
In addition to UDCA, several hepatoprotective agents (e.g., silymarin, single or complex compounds of biphenyl dimethyl dicarboxylate) are widely used as therapeutic drugs for acute or chronic liver disease in patients with abnormal liver function tests. Because no clinical studies of these drugs have been conducted in patients with NAFLD, more studies are needed to better understand the effects of these drugs on NAFLD. In addition to the medications mentioned above, a few new agents, such as the caspase inhibitor GS-9450,194 IKK2 antagonists,195 farnesoid X receptor agonists (FXR agonists),196 glucagon-like peptide-1 receptor antagonists,197 and phospholipids acting as nuclear receptor ligands,198 are highly anticipated.
Bariatric surgery
Bariatric surgery has been performed in morbidly obese patients, i.e., patients with life-threatening severe obesity who do not respond to medical treatment for weight loss.199 In Western countries, the indication for bariatric surgery is a patient with a BMI greater than 35 kg/m2 and hypertension or diabetes, or a patient with a BMI greater than 40 kg/m2.200 Several studies have reported significant weight loss, in addition to NAFLD improvement, due to bariatric surgery. In a 5-year follow-up study of 381 patients who underwent bariatric surgery, the BMI, amount of fat in the liver, and NAS were found to be reduced. However, small increases in the fibrosis index detected during follow-up testing must be further investigated.201 Of two meta-analysis studies undertaken to identify the role of bariatric surgery in NASH patients, one of the studies concluded that bariatric surgery is effective in reducing the amount of fat in the liver, inflammation, and fibrosis,202 but the other study stated that the effectiveness of bariatric surgery in NASH is unclear because well-designed, randomized, controlled studies have not yet been performed.203 Another limitation of bariatric surgery is the risk of lethal liver failure due to rapid weight loss, although this complication has only been reported in some cases of jejuno-ileal bypass surgery, unlike other bariatric surgery procedures.204,205 Bariatric surgery also requires caution in cirrhotic patients because there is a concern about its safety vs. its limited benefit.206,207 Prior to the decision to recommend bariatric surgery, peri- and post-operative complications and long-term malnutrition must be comprehensively considered.208,209
[Recommendations]
14. Bariatric surgery can be considered in patients with life-threatening severe obesity who do not respond to medical treatment. However, it is not recommended as a primary surgery for NASH treatment. (B1)
15. The effectiveness and safety of bariatric surgery have not been established in patients with severe liver fibrosis or cirrhosis. (B1)
CHILDREN AND ADOLESCENTS WITH NAFLD
Epidemiology
Severe complications can occur in adults with NAFLD that appeared during the pediatric and adolescent periods. Pediatric NAFLD has the same definition as adult NAFLD. The youngest age at which NASH-induced cirrhosis has been found is reportedly 8 years, and NASH-induced cirrhosis was first seen domestically in a 16-year-old girl with hypopituitarism.210-212 The accurate prevalence of NASH is uncertain because liver biopsy is also difficult to perform in pediatric patients. According to the routine physical examination data in the United States, 23% of students aged 17-18 years exhibited findings of increased ALT in Minnesota, California, Texas, and Louisiana. The Korea National Health and Nutrition Examination Survey, performed in 1998, revealed that ALT levels greater than 40 U/L were detected in 3.6% of boys and 2.8% of girls. In the 2010 National Sample Survey of Korean students, the prevalence of obesity was 11.7% (elementary [8.3%], middle [12.6%], and high [16.3%] schools). When health screening was conducted in obese students, the finding of ALT increases was observed in 11.3% of examinees (elementary [11.9%], middle [11.4%], and high [11.1%] schools).211,213,214 Considering that the prevalence of pediatric and adolescent obesity has shown an increasing tendency in Korea, the prevalence of NAFLD is very likely to increase as well.213,215 According to autopsy results of 742 US children and adolescents who died at ages of 2-19 years, 9.6% showed histological findings of NAFLD.210 In a multivariate analysis, the independent risk factors for NAFLD included obesity, male gender, older age (adolescent period), and ethnicity (Hispanic). The natural progression and medium- to long-term prognosis of NAFLD during pediatric and adolescent periods have not been clarified. In an international study in 66 patients with NAFLD, liver fibrosis progressed in four out of five patients who underwent liver biopsy. Among these patients, two underwent liver transplantation.216 The risk of NAFLD associated with metabolic syndrome could be as high as that in adults. However, the prevalence of NAFLD related to metabolic syndrome remains unclear because the definition of pediatric metabolic syndrome has not been fully established.217
Characteristics
Unlike in adult patients, the finding of fatty liver can be a commonly expressed phenotype in pediatric patients with metabolic syndrome caused by genetic disease. Therefore, Wilson's disease, Bardet-Biedl syndrome, PCOS, Prader-Willi syndrome, Turner syndrome, Cohen syndrome, alpha-1-antitrypsin deficiency, glycogen storage disease, hereditary tyrosinemia type 1, homocystinuria, Refsum disease, and citrullinemia, among others, must be distinguished through medical history, physical examination, and other tests before diagnosing NAFLD.218 The pathological findings in pediatric NAFLD are different from those in adult NAFLD. Macrovesicular hepatocellular steatosis, lobular inflammation, portal inflammation, portal fibrosis, and ballooning degeneration are commonly detected. NAFLD is divided into type 1, type 2, and mixed type based on the aspects of such findings. Pediatric NAFLD is characterized by macrovesicular steatosis, portal inflammation, and portal fibrosis, which are commonly observed in type 2 NAFLD and are distinct from adult NAFLD characteristics. Rather than the classification of typical type 1 and 2 NAFLD, portal inflammation has been recently underscored because it has been identified as a more distinctive condition in children.219,220 A domestic institution confirmed NAFLD in 80 children based on liver biopsy findings. Peri-sinusoidal fibrosis was observed in 45%, portal fibrosis was seen in 77%, simple steatosis was detected in 22%, type 1 NASH was present in 34%, and type 2 was present in 44% of subjects.221 Therefore, the conventionally used grading system was revised to incorporate the differences in pathological interpretation between adults and children. Consequently, the Pediatric NAFLD Histology Score has been presented and included along with portal inflammation in the grading system.222
Tests
Screening tests
There is no NAFLD screening guideline that has been verified in children. Instead, an expert consensus proposal has been suggested as a clinical practice guideline. Although ALT is generally used as an indirect marker of NAFLD in the non-invasive testing of obese pediatric patients, there is no universal standard.223,224 In a retrospective study of children and adolescents aged between 2 and 18 years, increases in serum ALT results and persistent increases in ALT values at the 6-month follow-up were considered to indicate NAFLD in overweight (BMI at or greater than the 85th percentile) and obese (BMI at or greater than the 95th percentile) subjects.225 In a prospective study of NAFLD-suspected children and adolescents aged between 6 and 17 years, NAFLD was diagnosed when ALT was maintained at greater than 60 U/L and steatosis was observed in liver biopsy samples.226 A committee consisting of experts from 15 associations under the supervision of the American Medical Association and the US Centers for Disease Control and Prevention recommended the performance of screening tests for AST and ALT biennially in children aged older than 10 years with a BMI at or greater than the 85th percentile, as well as the suspicion of NAFLD in cases of increased AST and ALT with findings of fatty liver on abdominal ultrasonography. In such cases, it is recommended to confirm NAFLD through liver biopsy.227 Despite these guidelines, the American Association for the Study of Liver Disease does not recommend general screening tests due to insufficient evidence.3 In a study of children and adolescents aged between 2 and 18 years, NAFLD was diagnosed through liver biopsy, and examinations were performed to assess the presence of hepatitis B or C virus, Wilson's disease, drug induced hepatitis, autoimmune hepatitis, and other diseases to distinguish NAFLD from chronic hepatitis.210,218 In accordance with related domestic laws, National Health Screening is performed in schools in 4th, 6th, 7th, and 10th graders to identify obesity in Korea. AST and ALT screening tests are additionally performed in overweight or obese students.213
Diagnosis
Liver biopsy plays a crucial role in the final diagnosis of NAFLD. In many studies, NAFLD was confirmed by liver biopsy in children and adolescents aged between 2 and 18 years with a BMI at or greater than the 85th percentile and with findings of increased ALT for more than 6 months.210,228 To distinguish NAFLD from chronic hepatitis due to other causes, screening tests were conducted for hepatitis B and C, Wilson's disease, metabolic disorders, muscular diseases, drug induced hepatitis, autoimmune hepatitis, and other diseases. It is essential to exclude the possibility of metabolic diseases in cases of young non-overweight or non-obese children who are suspected of having fatty liver disease.229 Some of the common findings of liver biopsy are severe liver cell injury, intralobular inflammation, and severe fibrosis in the peri-sinusoidal or periportal regions in children and adolescents, which are different from the findings in adults.219,220
[Recommendations]
16. For the diagnosis of NAFLD, screening tests for hepatitis B or C virus; metabolic syndromes, such as Wilson's disease; muscular diseases; drug-induced hepatitis; autoimmune hepatitis; and other diseases should be performed to distinguish chronic hepatitis from other causes. (B1)
17. Liver biopsy can be considered in cases of unclear diagnosis in children and adolescents suspected of having NASH. (B1)
18. During the interpretation of pediatric and adolescent liver biopsies, characteristic features of NASH in children should be considered to avoid confusing NASH with other fat-storing liver diseases in children. (B1)
Treatment
Lifestyle modification is the most important treatment for pediatric and adolescent patients with NAFLD.228,230 In a prospective study of NAFLD children and adolescents aged 3-19 years, lifestyle modification including diet and exercise, improved ALT levels and ultrasonographic findings.228 Moreover, a randomized, controlled study investigated the effects of placebo and antioxidants in 53 pediatric patients with NAFLD who made lifestyle modifications. A 24-month lifestyle modification intervention showed improvement in both liver biopsy findings and biochemical exam results. In this study, the daily administration of 600 IU of vitamin E combined with 500 mg of vitamin C yielded no additional benefits compared with the intervention of lifestyle modification alone.231 A randomized, controlled study of medication treatment compared the effects of 1,000 mg of metformin and 800 IU of vitamin E in patients aged 8-17 years who were diagnosed with NASH based on liver biopsy. Vitamin E failed to reduce the levels of liver enzymes, although it improved liver tissue findings, and metformin showed no significant differences.137 However, some studies have reported that the incidence of prostate cancer and the mortality rate of patients with head and neck cancer increased in adults who received high-dose vitamin E for long durations.141,232 The long-term use of high-dose vitamin E must be considered carefully in children and adolescents.
[Recommendations]
19. Lifestyle modification is recommended as a primary treatment, combined with dietary and exercise therapies, in children and adolescents with NAFLD. (A1)
20. Vitamin E can be administered to pediatric and adolescent patients with NASH confirmed by biopsy. (B1) However, there are safety concerns associated with the long-term use of vitamin E.
Acknowledgements
We thank KASL President: Chang Min Kim; KASL Director of the Medical Policy Committee: June Sung Lee (Inje University College of Medicine); KASL Clinical Practice Guidelines Reviewers: Jae Sung Ko (Seoul National University College of Medicine), Yeong-Oh Kwon (Kyungpook National University School of Medicine), Dae Ghon Kim (Chonbuk National University School of Medicine), Yun Soo Kim (Gachon Medical School), Hong Soo Kim (Soonchunhyang University College of Medicine), Joo Hyun Sohn (Hanyang University College of Medicine), Jong Eun Yeon (Korea University College of Medicine), Seung Kew Yoon (The Catholic University of Korea College of Medicine), Kwan Sik Lee (Yonsei University School of Medicine), Jeong Il Lee (Kyung Hee University College of Medicine) for their valuable discussions and helpful comments.
Notes
The authors have no conflicts to disclose.