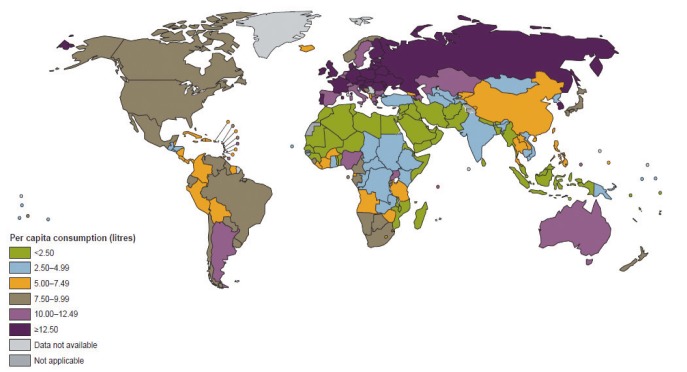
2. Room R, Babor T, Rehm J. Alcohol and public health. Lancet 2005;365:519-530. 15705462.


4. Corrao G, Ferrari P, Zambon A, Torchio P. Are the recent trends in liver cirrhosis mortality affected by the changes in alcohol consumption? Analysis of latency period in European countries. J Stud Alcohol 1997;58:486-494. 9273913.


5. Smart RG, Mann RE. Large decreases in alcohol-related problems following a slight reduction in alcohol consumption in Ontario 1975-83. Br J Addict 1987;82:285-291. 3471259.


6. Ramstedt M. Per capita alcohol consumption and liver cirrhosis mortality in 14 European countries. Addiction 2001;96(Suppl 1):S19-S33. 11228075.


7. Chung WJ, Chun HJ, Lee SM. Socioeconomic costs of alcohol drinking in Korea. J Prev Med Public Health 2006;39:21-29. 16613068.

8. Lee S, Chung W, Kim IS, Kim HJ, Cho W, Shin E, et al. Socioeconomic costs of alcohol drinking in Korea. J Korean Acad Fam Med 2008;29:201-212.
9. Park SC, Oh SI, Lee MS. Korean status of alcoholics and alcohol-related health problems. Alcohol Clin Exp Res 1998;22(3 Suppl):170S-172S. 9622398.


10. Kim SS, Gulick EE, Nam KA, Kim SH. Psychometric properties of the alcohol use disorders identification test: a Korean version. Arch Psychiatr Nurs 2008;22:190-199. 18640538.


11. Park SH, Kim CH, Kim DJ, Suk KT, Park HY, Lee JG, et al. Secular trends in prevalence of alcohol use disorder and its correlates in Korean adults: results from Korea National Health and Nutrition Examination Survey 2005 and 2009. Subst Abus 2012;33:327-335. 22989276.


12. Kim WR, Brown RS Jr, Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology 2002;36:227-242. 12085369.


14. Han YS, Kim BH, Baek IY, Lee DK, Kim KJ, Dong SH, et al. The change of the etiology, complications and cause of death of the liver cirrhosis in 1990s. Korean J Hepatol 2000;6:328-339.
15. Park SH. Association between alcohol consumption and metabolic syndrome among Korean adults: nondrinker versus lifetime abstainer as a reference group. Subst Use Misuse 2012;47:442-449. 22233521.


16. Park SH, Kim CH, Kim DJ, Park JH, Kim TO, Yang SY, et al. Prevalence of alcoholic liver disease among Korean adults: results from the fourth Korea National Health and Nutrition Examination Survey, 2009. Subst Use Misuse 2011;46:1755-1762. 21999409.


17. Rehm J, Gmel G, Sempos CT, Trevisan M. Alcohol-related morbidity and mortality. Alcohol Res Health 2003;27:39-51. 15301399.


19. Rehm J, Greenfield TK, Rogers JD. Average volume of alcohol consumption, patterns of drinking, and all-cause mortality: results from the US National Alcohol Survey. Am J Epidemiol 2001;153:64-71. 11159148.


20. Allen JP, Columbus M. Assessment in alcoholism treatment: An overview and quick reference instrument guide. In: Allen JP, Columbus M, eds. Assessing alcohol problems: a guide for clinicians and researchers. NIAAA treatment handbook series 4 (NIH Publication No. 95-3745). Bethesda: National Institute on Alcohol Abuse and Alcoholism; 1995. p. 1-15.
21. American Psychiatric Association. Diagnostic criteria from DSM-IV-TR. Washington D.C.: American Psychiatric Association; 2000.
22. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
23. Schuckit MA, Smith TL, Danko GP, Kramer J, Godinez J, Bucholz KK, et al. Prospective evaluation of the four DSM-IV criteria for alcohol abuse in a large population. Am J Psychiatry 2005;162:350-360. 15677601.


24. Regier DA, Narrow WE, Kuhl EA, Kupfer DJ. The conceptual development of DSM-V. Am J Psychiatry 2009;166:645-650. 19487400.


26. Ockene JK, Wheeler EV, Adams A, Hurley TG, Hebert J. Provider training for patient-centered alcohol counseling in a primary care setting. Arch Intern Med 1997;157:2334-2341. 9361574.


27. Fleming MF. Strategies to increase alcohol screening in health care settings. Alcohol Health Res World 1997;21:340-347. 15706746.


28. Reid MC, Fiellin DA, O'Connor PG. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med 1999;159:1681-1689. 10448769.


29. Fiellin DA, Reid MC, O'Connor PG. Screening for alcohol problems in primary care: a systematic review. Arch Intern Med 2000;160:1977-1989. 10888972.


30. Girela E, Villanueva E, Hernandez-Cueto C, Luna JD. Comparison of the CAGE questionnaire versus some biochemical markers in the diagnosis of alcoholism. Alcohol Alcohol 1994;29:337-343. 7945575.

31. Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry 1974;131:1121-1123. 4416585.


32. Dhalla S, Kopec JA. The CAGE questionnaire for alcohol misuse: a review of reliability and validity studies. Clin Invest Med 2007;30:33-41. 17716538.


33. Aertgeerts B, Buntinx F, Kester A. The value of the CAGE in screening for alcohol abuse and alcohol dependence in general clinical populations: a diagnostic meta-analysis. J Clin Epidemiol 2004;57:30-39. 15019008.


36. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 1993;88:791-804. 8329970.


37. Steinbauer JR, Cantor SB, Holzer CE 3rd, Volk RJ. Ethnic and sex bias in primary care screening tests for alcohol use disorders. Ann Intern Med 1998;129:353-362. 9735062.


38. Isaacson JH, Butler R, Zacharek M, Tzelepis A. Screening with the Alcohol use Disorders Identification Test (AUDIT) in an inner-city population. J Gen Intern Med 1994;9:550-553. 7823225.


40. Kim JS, Oh MK, Park BK, Lee MK, Kim GJ. Screening criteria of alcoholism by alcohol use disorders identification test (AUDIT) in Korea. J Korean Acad Fam Med 1999;20:1152-1159.
41. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158:1789-1795. 9738608.


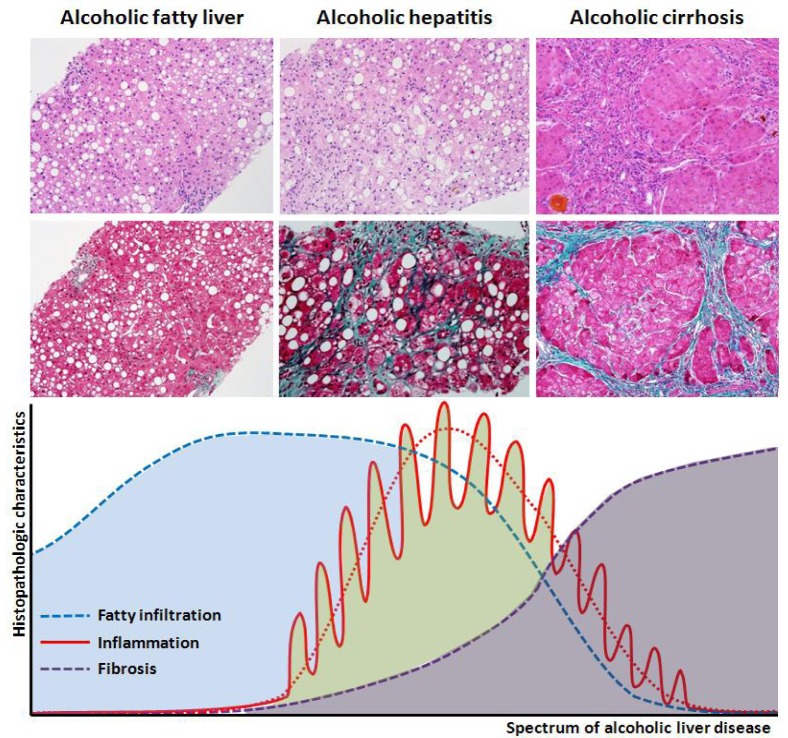
44. Lefkowitch JH. Morphology of alcoholic liver disease. Clin Liver Dis 2005;9:37-53. 15763228.


45. Méndez-Sánchez N, Almeda-Valdes P, Uribe M. Alcoholic liver disease. An update. Ann Hepatol 2005;4:32-42. 15798659.


46. O'Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology 2010;51:307-328. 20034030.


47. Yim HJ, Kim DJ, Kim JH, Heo J, Woo HY, Bae SH, et al. Prognosis of patients with alcoholic liver disease in Korea: Comparisons of prognostic models by a national-wide survey [Abstract]. Hepatol Int 2013;7(Suppl):S44.
48. Veldt BJ, Laine F, Guillygomarc'h A, Lauvin L, Boudjema K, Messner M, et al. Indication of liver transplantation in severe alcoholic liver cirrhosis: quantitative evaluation and optimal timing. J Hepatol 2002;36:93-98. 11804670.


49. Leevy CM. Fatty liver: a study of 270 patients with biopsy proven fatty liver and review of the literature. Medicine (Baltimore) 1962;41:249-276. 14463641.


50. Sørensen TI, Orholm M, Bentsen KD, Hoybye G, Eghoje K, Christoffersen P. Prospective evaluation of alcohol abuse and alcoholic liver injury in men as predictors of development of cirrhosis. Lancet 1984;2:241-244. 6146805.


51. Stickel F, Seitz HK. Alcoholic steatohepatitis. Best Pract Res Clin Gastroenterol 2010;24:683-693. 20955970.


53. Teli MR, Day CP, Burt AD, Bennett MK, James OF. Determinants of progression to cirrhosis or fibrosis in pure alcoholic fatty liver. Lancet 1995;346:987-990. 7475591.


54. Orrego H, Blake JE, Blendis LM, Medline A. Prognosis of alcoholic cirrhosis in the presence and absence of alcoholic hepatitis. Gastroenterology 1987;92:208-214. 3781189.


55. Carithers RL Jr, Herlong HF, Diehl AM, Shaw EW, Combes B, Fallon HJ, et al. Methylprednisolone therapy in patients with severe alcoholic hepatitis. A randomized multicenter trial. Ann Intern Med 1989;110:685-690. 2648927.


57. Lucey MR, Mathurin P, Morgan TR. Alcoholic hepatitis. N Engl J Med 2009;360:2758-2769. 19553649.


58. Cortez-Pinto H, Baptista A, Camilo ME, De Moura MC. Nonalcoholic steatohepatitis--a long-term follow-up study: comparison with alcoholic hepatitis in ambulatory and hospitalized patients. Dig Dis Sci 2003;48:1909-1913. 14627331.


59. Parés A, Caballeria J, Bruguera M, Torres M, Rodes J. Histological course of alcoholic hepatitis. Influence of abstinence, sex and extent of hepatic damage. J Hepatol 1986;2:33-42. 3950362.


60. Sandahl TD, Jepsen P, Thomsen KL, Vilstrup H. Incidence and mortality of alcoholic hepatitis in Denmark 1999-2008: a nationwide population based cohort study. J Hepatol 2011;54:760-764. 21126790.


62. Propst A, Propst T, Zangerl G, Ofner D, Judmaier G, Vogel W. Prognosis and life expectancy in chronic liver disease. Dig Dis Sci 1995;40:1805-1815. 7648984.


63. Jepsen P, Ott P, Andersen PK, Sorensen HT, Vilstrup H. Clinical course of alcoholic liver cirrhosis: a Danish population-based cohort study. Hepatology 2010;51:1675-1682. 20186844.


64. Fleming KM, Aithal GP, Card TR, West J. The rate of decompensation and clinical progression of disease in people with cirrhosis: a cohort study. Aliment Pharmacol Ther 2010;32:1343-1350. 21050236.


66. Uzunalimoğlu O, Yurdaydin C, Cetinkaya H, Bozkaya H, Sahin T, Colakoglu S, et al. Risk factors for hepatocellular carcinoma in Turkey. Dig Dis Sci 2001;46:1022-1028. 11341644.


67. N'Kontchou G, Paries J, Htar MT, Ganne-Carrie N, Costentin L, Grando-Lemaire V, et al. Risk factors for hepatocellular carcinoma in patients with alcoholic or viral C cirrhosis. Clin Gastroenterol Hepatol 2006;4:1062-1068. 16844421.


68. Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 2004;127(5 Suppl 1):S35-S50. 15508101.


69. Schafer DF, Sorrell MF. Hepatocellular carcinoma. Lancet 1999;353:1253-1257. 10217098.


70. Horie Y, Yamagishi Y, Kajihara M, Kato S, Ishii H. National survey of hepatocellular carcinoma in heavy drinkers in Japan. Alcohol Clin Exp Res 2003;27(8 Suppl):32S-36S. 12960504.


71. Fleming KM, Aithal GP, Card TR, West J. All-cause mortality in people with cirrhosis compared with the general population: a population-based cohort study. Liver Int 2012;32:79-84. 21745279.

73. Diehl AM. Alcoholic liver disease: natural history. Liver Transpl Surg 1997;3:206-211. 9346741.


74. Diehl AM. Liver disease in alcohol abusers: clinical perspective. Alcohol 2002;27:7-11. 12062630.


75. Alvarez MA, Cirera I, Sola R, Bargallo A, Morillas RM, Planas R. Long-term clinical course of decompensated alcoholic cirrhosis: a prospective study of 165 patients. J Clin Gastroenterol 2011;45:906-911. 21814145.


76. Borowsky SA, Strome S, Lott E. Continued heavy drinking and survival in alcoholic cirrhotics. Gastroenterology 1981;80:1405-1409. 6971772.


77. Bellentani S, Tiribelli C, Saccoccio G, Sodde M, Fratti N, De Martin C, et al. Prevalence of chronic liver disease in the general population of northern Italy: the Dionysos Study. Hepatology 1994;20:1442-1449. 7982643.


78. Kamper-Jørgensen M, Gronbaek M, Tolstrup J, Becker U. Alcohol and cirrhosis: dose--response or threshold effect? J Hepatol 2004;41:25-30. 15246203.


82. Batey RG, Burns T, Benson RJ, Byth K. Alcohol consumption and the risk of cirrhosis. Med J Aust 1992;156:413-416. 1545749.


83. Zakhari S, Li TK. Determinants of alcohol use and abuse: Impact of quantity and frequency patterns on liver disease. Hepatology 2007;46:2032-2039. 18046720.


85. Klatsky AL, Armstrong MA, Friedman GD. Alcohol and mortality. Ann Intern Med 1992;117:646-654. 1530196.


86. Bouchier IA, Hislop WS, Prescott RJ. A prospective study of alcoholic liver disease and mortality. J Hepatol 1992;16:290-297. 1487605.


88. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 2012;55:2005-2023. 22488764.


89. Hrubec Z, Omenn GS. Evidence of genetic predisposition to alcoholic cirrhosis and psychosis: twin concordances for alcoholism and its biological end points by zygosity among male veterans. Alcohol Clin Exp Res 1981;5:207-215. 7018299.


91. Wilkinson P, Santamaria JN, Rankin JG. Epidemiology of alcoholic cirrhosis. Australas Ann Med 1969;18:222-226. 5351239.


92. Renaud SC. Diet and stroke. J Nutr Health Aging 2001;5:167-172. 11458287.

93. Mathurin P, Deltenre P. Effect of binge drinking on the liver: an alarming public health issue? Gut 2009;58:613-617. 19174416.


94. Hatton J, Burton A, Nash H, Munn E, Burgoyne L, Sheron N. Drinking patterns, dependency and life-time drinking history in alcohol-related liver disease. Addiction 2009;104:587-592. 19215600.


96. Grønbaek M, Becker U, Johansen D, Gottschau A, Schnohr P, Hein HO, et al. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann Intern Med 2000;133:411-419. 10975958.


97. Becker U, Deis A, Sorensen TI, Gronbaek M, Borch-Johnsen K, Muller CF, et al. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology 1996;23:1025-1029. 8621128.


98. Frezza M, di Padova C, Pozzato G, Terpin M, Baraona E, Lieber CS. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med 1990;322:95-99. 2248624.


101. Ashley MJ, Olin JS, le Riche WH, Kornaczewski A, Schmidt W, Rankin JG. Morbidity in alcoholics. Evidence for accelerated development of physical disease in women. Arch Intern Med 1977;137:883-887. 879927.


102. Marshall AW, Kingstone D, Boss M, Morgan MY. Ethanol elimination in males and females: relationship to menstrual cycle and body composition. Hepatology 1983;3:701-706. 6618437.


103. Baraona E, Abittan CS, Dohmen K, Moretti M, Pozzato G, Chayes ZW, et al. Gender differences in pharmacokinetics of alcohol. Alcohol Clin Exp Res 2001;25:502-507. 11329488.


104. Stewart SH. Racial and ethnic differences in alcohol-associated aspartate aminotransferase and gamma-glutamyltransferase elevation. Arch Intern Med 2002;162:2236-2239. 12390068.


105. Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res 2001;25:1181-1187. 11505049.


106. Wickramasinghe SN, Corridan B, Izaguirre J, Hasan R, Marjot DH. Ethnic differences in the biological consequences of alcohol abuse: a comparison between south Asian and European males. Alcohol Alcohol 1995;30:675-680. 8554653.

107. Mendenhall CL, Anderson S, Weesner RE, Goldberg SJ, Crolic KA. Protein-calorie malnutrition associated with alcoholic hepatitis. Veterans Administration Cooperative Study Group on Alcoholic Hepatitis. Am J Med 1984;76:211-222. 6421159.


108. Mendenhall C, Roselle GA, Gartside P, Moritz T. Relationship of protein calorie malnutrition to alcoholic liver disease: a reexamination of data from two Veterans Administration Cooperative Studies. Alcohol Clin Exp Res 1995;19:635-641. 7573786.


111. Diehl AM. Obesity and alcoholic liver disease. Alcohol 2004;34:81-87. 15670669.


114. Tsai J, Ford ES, Zhao G, Li C, Greenlund KJ, Croft JB. Co-occurrence of obesity and patterns of alcohol use associated with elevated serum hepatic enzymes in US adults. J Behav Med 2012;35:200-210. 21626151.


115. Shen Z, Li Y, Yu C, Shen Y, Xu L, Xu C, et al. A cohort study of the effect of alcohol consumption and obesity on serum liver enzyme levels. Eur J Gastroenterol Hepatol 2010;22:820-825. 19829121.


119. Raynard B, Balian A, Fallik D, Capron F, Bedossa P, Chaput JC, et al. Risk factors of fibrosis in alcohol-induced liver disease. Hepatology 2002;35:635-638. 11870378.


121. Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology 1997;25:108-111. 8985274.


122. Goodwin DW, Schulsinger F, Hermansen L, Guze SB, Winokur G. Alcohol problems in adoptees raised apart from alcoholic biological parents. Arch Gen Psychiatry 1973;28:238-243. 4684290.


123. Kaprio J, Koskenvuo M, Langinvainio H, Romanov K, Sarna S, Rose RJ. Social and genetic influences on drinking patterns of adult men: a study of 5638 Finnish twin brothers. Alcohol Alcohol Suppl 1987;1:373-377. 3426703.

124. Zintzaras E, Stefanidis I, Santos M, Vidal F. Do alcohol-metabolizing enzyme gene polymorphisms increase the risk of alcoholism and alcoholic liver disease? Hepatology 2006;43:352-361. 16440362.


126. Kim MS, Lee DH, Kang HS, Park HS, Jung S, Lee JW, et al. Genetic polymorphisms of alcohol-metabolizing enzymes and cytokines in patients with alcohol induced pancreatitis and alcoholic liver cirrhosis. Korean J Gastroenterol 2004;43:355-363. 15220553.

128. Sookoian S, Pirola CJ. Meta-analysis of the influence of I148M variant of patatin-like phospholipase domain containing 3 gene (PNPLA3) on the susceptibility and histological severity of nonalcoholic fatty liver disease. Hepatology 2011;53:1883-1894. 21381068.


130. Marcos M, Pastor I, Chamorro AJ, Ciria-Abad S, Gonzalez-Sarmiento R, Laso FJ. Meta-analysis: glutathione-S-transferase allelic variants are associated with alcoholic liver disease. Aliment Pharmacol Ther 2011;34:1159-1172. 21967547.


132. Harris DR, Gonin R, Alter HJ, Wright EC, Buskell ZJ, Hollinger FB, et al. The relationship of acute transfusion-associated hepatitis to the development of cirrhosis in the presence of alcohol abuse. Ann Intern Med 2001;134:120-124. 11177315.


133. Walter SR, Thein HH, Gidding HF, Amin J, Law MG, George J, et al. Risk factors for hepatocellular carcinoma in a cohort infected with hepatitis B or C. J Gastroenterol Hepatol 2011;26:1757-1764. 21615789.


134. Anand BS, Currie S, Dieperink E, Bini EJ, Shen H, Ho SB, et al. Alcohol use and treatment of hepatitis C virus: results of a national multicenter study. Gastroenterology 2006;130:1607-1616. 16697724.


136. French SW. Ethanol and hepatocellular injury. Clin Lab Med 1996;16:289-306. 8792073.


137. Corrao G, Lepore AR, Torchio P, Valenti M, Galatola G, D'Amicis A, et al. Provincial Group for the Study of Chronic Liver Disease. The effect of drinking coffee and smoking cigarettes on the risk of cirrhosis associated with alcohol consumption. A case-control study. Eur J Epidemiol 1994;10:657-664. 7672043.


138. Muriel P, Arauz J. Coffee and liver diseases. Fitoterapia 2010;81:297-305. 19825397.


139. Klatsky AL, Morton C, Udaltsova N, Friedman GD. Coffee, cirrhosis, and transaminase enzymes. Arch Intern Med 2006;166:1190-1195. 16772246.


140. Corrao G, Zambon A, Bagnardi V, D'Amicis A, Klatsky A. Coffee, caffeine, and the risk of liver cirrhosis. Ann Epidemiol 2001;11:458-465. 11557177.


141. Gallus S, Tavani A, Negri E, La Vecchia C. Does coffee protect against liver cirrhosis? Ann Epidemiol 2002;12:202-205. 11897178.


142. Tverdal A, Skurtveit S. Coffee intake and mortality from liver cirrhosis. Ann Epidemiol 2003;13:419-423. 12875799.


143. European Association for the Study of Liver. EASL Clinical Practical Guidelines: Management of Alcoholic Liver Disease. J Hepatol 2012;57:399-420. 22633836.


145. Baraona E, Lieber CS. Alcohol and lipids. Recent Dev Alcohol 1998;14:97-134. 9751944.


147. Ji C, Chan C, Kaplowitz N. Predominant role of sterol response element binding proteins (SREBP) lipogenic pathways in hepatic steatosis in the murine intragastric ethanol feeding model. J Hepatol 2006;45:717-724. 16879892.


148. Nakajima T, Kamijo Y, Tanaka N, Sugiyama E, Tanaka E, Kiyosawa K, et al. Peroxisome proliferator-activated receptor alpha protects against alcohol-induced liver damage. Hepatology 2004;40:972-980. 15382117.


152. Seth D, Gorrell MD, Cordoba S, McCaughan GW, Haber PS. Intrahepatic gene expression in human alcoholic hepatitis. J Hepatol 2006;45:306-320. 16797773.


153. Urbaschek R, McCuskey RS, Rudi V, Becker KP, Stickel F, Urbaschek B, et al. Endotoxin, endotoxin-neutralizing-capacity, sCD14, sICAM-1, and cytokines in patients with various degrees of alcoholic liver disease. Alcohol Clin Exp Res 2001;25:261-268. 11236841.


154. Thurman RG. II. Alcoholic liver injury involves activation of Kupffer cells by endotoxin. Am J Physiol 1998;275:G605-G611. 9756487.


157. Moreno M, Bataller R. Cytokines and renin-angiotensin system signaling in hepatic fibrosis. Clin Liver Dis 2008;12:825-852. ix. 18984469.


158. McQuade WH, Levy SM, Yanek LR, Davis SW, Liepman MR. Detecting symptoms of alcohol abuse in primary care settings. Arch Fam Med 2000;9:814-821. 11031387.


159. Eckardt MJ, Rawlings RR, Martin PR. Biological correlates and detection of alcohol abuse and alcoholism. Prog Neuropsychopharmacol Biol Psychiatry 1986;10:135-144. 2875489.


161. Sherman HI, Hardison JE. The importance of a coexistent hepatic rub and bruit. A clue to the diagnosis of cancer in the liver. JAMA 1979;241:1495. 430691.


162. Goldstein LI. Enlarged, tortuous arteries and hepatic bruit. JAMA 1968;206:2518-2520. 5754993.


163. Mendenhall CL. Alcoholic hepatitis. Clin Gastroenterol 1981;10:417-441. 7018751.


164. Estruch R, Nicolas JM, Villegas E, Junque A, Urbano-Marquez A. Relationship between ethanol-related diseases and nutritional status in chronically alcoholic men. Alcohol Alcohol 1993;28:543-550. 8274178.

165. Anderson P, Cremona A, Paton A, Turner C, Wallace P. The risk of alcohol. Addiction 1993;88:1493-1508. 8286995.


166. Lazarević AM, Nakatani S, Neskovic AN, Marinkovic J, Yasumura Y, Stojicic D, et al. Early changes in left ventricular function in chronic asymptomatic alcoholics: relation to the duration of heavy drinking. J Am Coll Cardiol 2000;35:1599-1606. 10807466.


168. Klatsky AL, Chartier D, Udaltsova N, Gronningen S, Brar S, Friedman GD, et al. Alcohol drinking and risk of hospitalization for heart failure with and without associated coronary artery disease. Am J Cardiol 2005;96:346-351. 16054455.


169. Preedy VR, Adachi J, Ueno Y, Ahmed S, Mantle D, Mullatti N, et al. Alcoholic skeletal muscle myopathy: definitions, features, contribution of neuropathy, impact and diagnosis. Eur J Neurol 2001;8:677-687. 11784353.


170. Yersin B, Nicolet JF, Dercrey H, Burnier M, van Melle G, Pecoud A. Screening for excessive alcohol drinking. Comparative value of carbohydrate-deficient transferrin, gamma-glutamyltransferase, and mean corpuscular volume. Arch Intern Med 1995;155:1907-1911. 7677558.


171. Reynaud M, Schellenberg F, Loisequx-Meunier MN, Schwan R, Maradeix B, Planche F, et al. Objective diagnosis of alcohol abuse: compared values of carbohydrate-deficient transferrin (CDT), gamma-glutamyl transferase (GGT), and mean corpuscular volume (MCV). Alcohol Clin Exp Res 2000;24:1414-1419. 11003208.


172. Conigrave KM, Degenhardt LJ, Whitfield JB, Saunders JB, Helander A, Tabakoff B. CDT, GGT, and AST as markers of alcohol use: the WHO/ISBRA collaborative project. Alcohol Clin Exp Res 2002;26:332-339. 11923585.


173. Rinck D, Frieling H, Freitag A, Hillemacher T, Bayerlein K, Kornhuber J, et al. Combinations of carbohydrate-deficient transferrin, mean corpuscular erythrocyte volume, gamma-glutamyltransferase, homocysteine and folate increase the significance of biological markers in alcohol dependent patients. Drug Alcohol Depend 2007;89:60-65. 17234365.


174. Nanji AA, French SW, Mendenhall CL. Serum aspartate aminotransferase to alanine aminotransferase ratio in human and experimental alcoholic liver disease: relationship to histologic changes. Enzyme 1989;41:112-115. 2707213.


175. Cohen JA, Kaplan MM. The SGOT/SGPT ratio--an indicator of alcoholic liver disease. Dig Dis Sci 1979;24:835-838. 520102.


178. Wu A, Slavin G, Levi AJ. Elevated serum gamma-glutamyl-transferase (transpeptidase) and histological liver damage in alcoholism. Am J Gastroenterol 1976;65:318-323. 7137.

180. Litten RZ, Bradley AM, Moss HB. Alcohol biomarkers in applied settings: recent advances and future research opportunities. Alcohol Clin Exp Res 2010;34:955-967. 20374219.


181. Wu A, Chanarin I, Levi AJ. Macrocytosis of chronic alcoholism. Lancet 1974;1:829-831. 4132788.

182. Whitehead TP, Clarke CA, Whitfield AG. Biochemical and haematological markers of alcohol intake. Lancet 1978;1:978-981. 76902.


183. Sharpe PC. Biochemical detection and monitoring of alcohol abuse and abstinence. Ann Clin Biochem 2001;38:652-664. 11732647.


184. Morgan MY, Camilo ME, Luck W, Sherlock S, Hoffbrand AV. Macrocytosis in alcohol-related liver disease: its value for screening. Clin Lab Haematol 1981;3:35-44. 7226720.


185. Arndt T. Carbohydrate-deficient transferrin as a marker of chronic alcohol abuse: a critical review of preanalysis, analysis, and interpretation. Clin Chem 2001;47:13-27. 11148172.


186. Bortolotti F, De Paoli G, Tagliaro F. Carbohydrate-deficient transferrin (CDT) as a marker of alcohol abuse: a critical review of the literature 2001-2005. J Chromatogr B Analyt Technol Biomed Life Sci 2006;841:96-109.


187. Salaspuro M. Carbohydrate-deficient transferrin as compared to other markers of alcoholism: a systematic review. Alcohol 1999;19:261-271. 10580517.


188. Zoli M, Cordiani MR, Marchesini G, Iervese T, Labate AM, Bonazzi C, et al. Prognostic indicators in compensated cirrhosis. Am J Gastroenterol 1991;86:1508-1513. 1928047.

189. Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol 2010;53:372-384. 20494470.


190. d'Assignies G, Ruel M, Khiat A, Lepanto L, Chagnon M, Kauffmann C, et al. Noninvasive quantitation of human liver steatosis using magnetic resonance and bioassay methods. Eur Radiol 2009;19:2033-2040. 19280194.


191. Mancini M, Prinster A, Annuzzi G, Liuzzi R, Giacco R, Medagli C, et al. Sonographic hepatic-renal ratio as indicator of hepatic steatosis: comparison with (1)H magnetic resonance spectroscopy. Metabolism 2009;58:1724-1730. 19716568.


192. Lee JY, Choi BI. Ultrasound-based Liver Elastography: Recent Advances. J Korean Soc Ultrasound Med 2011;30:239-244.
194. Wang QB, Zhu H, Liu HL, Zhang B. Performance of magnetic resonance elastography and diffusion-weighted imaging for the staging of hepatic fibrosis: A meta-analysis. Hepatology 2012;56:239-247. 22278368.


197. Hall PD. Pathological spectrum of alcoholic liver disease. Alcohol Alcohol Suppl 1994;2:303-313. 8974350.


198. Mathurin P, Beuzin F, Louvet A, Carrie-Ganne N, Balian A, Trinchet JC, et al. Fibrosis progression occurs in a subgroup of heavy drinkers with typical histological features. Aliment Pharmacol Ther 2007;25:1047-1054. 17439505.


199. Kalambokis G, Manousou P, Vibhakorn S, Marelli L, Cholongitas E, Senzolo M, et al. Transjugular liver biopsy--indications, adequacy, quality of specimens, and complications--a systematic review. J Hepatol 2007;47:284-294. 17561303.


201. Naveau S, Gaude G, Asnacios A, Agostini H, Abella A, Barri-Ova N, et al. Diagnostic and prognostic values of noninvasive biomarkers of fibrosis in patients with alcoholic liver disease. Hepatology 2009;49:97-105. 19053048.


202. Levin DM, Baker AL, Riddell RH, Rochman H, Boyer JL. Nonalcoholic liver disease. Overlooked causes of liver injury in patients with heavy alcohol consumption. Am J Med 1979;66:429-434. 433949.


203. Mathurin P, Duchatelle V, Ramond MJ, Degott C, Bedossa P, Erlinger S, et al. Survival and prognostic factors in patients with severe alcoholic hepatitis treated with prednisolone. Gastroenterology 1996;110:1847-1853. 8964410.


205. Mookerjee RP, Lackner C, Stauber R, Stadlbauer V, Deheragoda M, Aigelsreiter A, et al. The role of liver biopsy in the diagnosis and prognosis of patients with acute deterioration of alcoholic cirrhosis. J Hepatol 2011;55:1103-1111. 21376092.


206. Alcoholic liver disease: morphological manifestations. Review by an international group. Lancet 1981;1:707-711. 6110925.

207. Nalpas B, Vassault A, Le Guillou A, Lesgourgues B, Ferry N, Lacour B, et al. Serum activity of mitochondrial aspartate aminotransferase: a sensitive marker of alcoholism with or without alcoholic hepatitis. Hepatology 1984;4:893-896. 6148299.


209. Maddrey WC, Boitnott JK, Bedine MS, Weber FL Jr, Mezey E, White RI Jr. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology 1978;75:193-199. 352788.


210. Mathurin P, O'Grady J, Carithers RL, Phillips M, Louvet A, Mendenhall CL, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut 2011;60:255-260. 20940288.


211. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PCJ. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000;31:864-871. 10733541.


212. Dunn W, Jamil LH, Brown LS, Wiesner RH, Kim WR, Menon KVN, et al. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology 2005;41:353-358. 15660383.


213. Srikureja W, Kyulo NL, Runyon BA, Hu KQ. MELD score is a better prognostic model than Child-Turcotte-Pugh score or Discriminant Function score in patients with alcoholic hepatitis. J Hepatol 2005;42:700-706. 15826720.


218. Dominguez M, Rincón D, Abraldes JG, Miquel R, Colmenero J, Bellot P, et al. A new scoring system for prognostic stratification of patients with alcoholic hepatitis. Am J Gastroenterol 2008;103:2747-2756. 18721242.


219. Rincon D, Lo Iacono O, Ripoll C, Gomez-Camarero J, Salcedo M, Catalina MV, et al. Prognostic value of hepatic venous pressure gradient for in-hospital mortality of patients with severe acute alcoholic hepatitis. Aliment Pharmacol Ther 2007;25:841-848. 17373923.


221. Jeong JY, Sohn JH, Son BK, Paik CH, Kim SH, Han DS, et al. Comparison of model for end-stage liver disease score with discriminant function and child-Turcotte-Pugh scores for predicting short-term mortality in Korean patients with alcoholic hepatitis. Korean J Gastroenterol 2007;49:93-99. 17322788.

222. Ali S, Hussain S, Hair M, Shah A. Comparison of Maddrey Discriminant Function, Child-Pugh Score and Glasgow Alcoholic Hepatitis Score in predicting 28-day mortality on admission in patients with acute hepatitis. Ir J Med Sci 2013;182:63-68. 22544466.


223. Mathurin P, Louvet A, Dharancy S. Treatment of severe forms of alcoholic hepatitis: Where are we going? J Gastroenterol Hepatol 2008;23(Suppl 1):S60-S62. 18336666.


224. Mathurin P, Abdelnour M, Ramond MJ, Carbonell N, Fartoux L, Serfaty L, et al. Early change in bilirubin levels is an important prognostic factor in severe alcoholic hepatitis treated with prednisolone. Hepatology 2003;38:1363-1369. 14647046.


225. Morris JM, Forrest EH. Bilirubin response to corticosteroids in severe alcoholic hepatitis. Eur J Gastroenterol Hepatol 2005;17:759-762. 15947554.


226. Louvet A, Naveau S, Abdelnour M, Ramond MJ, Diaz E, Fartoux L, et al. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology 2007;45:1348-1354. 17518367.


227. Mayo-Smith MF, Beecher LH, Fischer TL, Gorelick DA, Guillaume JL, Hill A, et al. Management of alcohol withdrawal delirium. An evidence-based practice guideline. Arch Intern Med 2004;164:1405-1412. 15249349.


228. Kim HY, Lee HK, Lee KS, Joe KH, Choi SW, Seo JS. Korean addiction treatment guidelines series (II): Pharmacological treatment of alcohol withdrawal. J Korean Neuropsychiatr Assoc 2013;52:67-75.

229. Hayashida M, Alterman AI, McLellan AT, O'Brien CP, Purtill JJ, Volpicelli JR, et al. Comparative effectiveness and costs of inpatient and outpatient detoxification of patients with mild-to-moderate alcohol withdrawal syndrome. N Engl J Med 1989;320:358-365. 2913493.


230. Saitz R, O'Malley SS. Pharmacotherapies for alcohol abuse. Withdrawal and treatment. Med Clin North Am 1997;81:881-907. 9222259.


231. O'coner PG. Alcohol abuse and depence. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine. 24th Edition. PA: ELSEVIER SAUNDERS; 2012. p. 146-153.
232. American Society of Helth-system Pharmacists. AHFS Drug Information 2012. MD: American Society of Health-System Pharmacists; 2011. p. 2542-2627.
233. Day E, Bentham P, Callaghan R, Kuruvilla T, George S. Thiamine for Wernicke-Korsakoff Syndrome in people at risk from alcohol abuse. Cochrane Database Syst Rev 2004;CD004033. 14974055.


234. Pessione F, Ramond MJ, Peters L, Pham BN, Batel P, Rueff B, et al. Five-year survival predictive factors in patients with excessive alcohol intake and cirrhosis. Effect of alcoholic hepatitis, smoking and abstinence. Liver Int 2003;23:45-53. 12640727.


235. Luca A, Garcia-Pagan JC, Bosch J, Feu F, Caballeria J, Groszmann RJ, et al. Effects of ethanol consumption on hepatic hemodynamics in patients with alcoholic cirrhosis. Gastroenterology 1997;112:1284-1289. 9098014.


236. Morgan MY. The prognosis and outcome of alcoholic liver disease. Alcohol Alcohol Suppl 1994;2:335-343. 8974353.

237. Miguet M, Monnet E, Vanlemmens C, Gache P, Messner M, Hruskovsky S, et al. Predictive factors of alcohol relapse after orthotopic liver transplantation for alcoholic liver disease. Gastroenterol Clin Biol 2004;28:845-851. 15523219.


238. Davidoff RA. Antispasticity drugs: mechanisms of action. Ann Neurol 1985;17:107-116. 2858176.


239. Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet 2007;370:1915-1922. 18068515.


240. Liu J, Wang L. Baclofen for alcohol withdrawal. Cochrane Database Syst Rev 2011;CD008502. 21249712.


241. Heydtmann M. Baclofen effect related to liver damage. Alcohol Clin Exp Res 2011;35:848. 21303383.


242. Mann K, Lehert P, Morgan MY. The efficacy of acamprosate in the maintenance of abstinence in alcohol-dependent individuals: results of a meta-analysis. Alcohol Clin Exp Res 2004;28:51-63. 14745302.


244. Bouza C, Angeles M, Munoz A, Amate JM. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction 2004;99:811-828. 15200577.


245. Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 2006;295:2003-2017. 16670409.


246. Donovan DM, Anton RF, Miller WR, Longabaugh R, Hosking JD, Youngblood M, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence (The COMBINE Study): examination of posttreatment drinking outcomes. J Stud Alcohol Drugs 2008;69:5-13. 18080059.


247. Rösner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev 2010;CD001867. 21154349.


248. Soyka M, Rosner S. Opioid antagonists for pharmacological treatment of alcohol dependence-a critical review. Curr Drug Abuse Rev 2008;1:280-291. 19630726.


249. Roozen HG, de Waart R, van der Windt DA, van den Brink W, de Jong CA, Kerkhof AJ. A systematic review of the effectiveness of naltrexone in the maintenance treatment of opioid and alcohol dependence. Eur Neuropsychopharmacol 2006;16:311-323. 16361086.


250. Barth KS, Malcolm RJ. Disulfiram: an old therapeutic with new applications. CNS Neurol Disord Drug Targets 2010;9:5-12. 20201810.


251. Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction 2002;97:265-277. 11964100.


253. Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction 1993;88:315-335. 8461850.


254. Heather N, Brodie J, Wale S, Wilkinson G, Luce A, Webb E, et al. A randomized controlled trial of Moderation-Oriented Cue Exposure. J Stud Alcohol 2000;61:561-570. 10928726.


257. Kaner EF, Dickinson HO, Beyer F, Pienaar E, Schlesinger C, Campbell F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev 2009;28:301-323. 19489992.


258. Moyer A, Finney JW, Elworth JT, Kraemer HC. Can methodological features account for patient-treatment matching findings in the alcohol field? J Stud Alcohol 2001;62:62-73. 11271966.


259. Lee S, Jin Y, Kee C, Chang Y. Nutritional status in alcohol- and virus-related liver cirrhosis. Korean J Hepatol 2000;6:59-72.
260. Stickel F, Hoehn B, Schuppan D, Seitz HK. Review article: Nutritional therapy in alcoholic liver disease. Aliment Pharmacol Ther 2003;18:357-373. 12940921.


261. Henkel AS, Buchman AL. Nutritional support in patients with chronic liver disease. Nat Clin Pract Gastroenterol Hepatol 2006;3:202-209. 16582962.


262. Koretz RL, Avenell A, Lipman TO. Nutritional support for liver disease. Cochrane Database Syst Rev 2012;5:CD008344. 22592729.

263. Cabré E, Rodriguez-Iglesias P, Caballeria J, Quer JC, Sanchez-Lombrana JL, Pares A, et al. Short- and long-term outcome of severe alcohol-induced hepatitis treated with steroids or enteral nutrition: a multicenter randomized trial. Hepatology 2000;32:36-42. 10869286.


264. Marchesini G, Dioguardi FS, Bianchi GP, Zoli M, Bellati G, Roffi L, et al. The Italian Multicenter Study Group. Long-term oral branched-chain amino acid treatment in chronic hepatic encephalopathy. A randomized double-blind casein-controlled trial. J Hepatol 1990;11:92-101. 2204661.


265. Hirsch S, Bunout D, de la Maza P, Iturriaga H, Petermann M, Icazar G, et al. Controlled trial on nutrition supplementation in outpatients with symptomatic alcoholic cirrhosis. JPEN J Parenter Enteral Nutr 1993;17:119-124. 8455312.


266. Plauth M, Cabre E, Riggio O, Assis-Camilo M, Pirlich M, Kondrup J, et al. ESPEN Guidelines on Enteral Nutrition: Liver disease. Clin Nutr 2006;25:285-294. 16707194.


267. Lochs H, Plauth M. Liver cirrhosis: rationale and modalities for nutritional support--the European Society of Parenteral and Enteral Nutrition consensus and beyond. Curr Opin Clin Nutr Metab Care 1999;2:345-349. 10453318.


269. Zillikens MC, van den Berg JW, Wattimena JL, Rietveld T, Swart GR. Nocturnal oral glucose supplementation. The effects on protein metabolism in cirrhotic patients and in healthy controls. J Hepatol 1993;17:377-383. 8315266.


270. Plauth M, Cabre E, Campillo B, Kondrup J, Marchesini G, Schutz T, et al. ESPEN Guidelines on Parenteral Nutrition: hepatology. Clin Nutr 2009;28:436-444. 19520466.


271. DiCecco SR, Francisco-Ziller N. Nutrition in alcoholic liver disease. Nutr Clin Pract 2006;21:245-254. 16772542.


272. Alvarez MA, Cabre E, Lorenzo-Zuniga V, Montoliu S, Planas R, Gassull MA. Combining steroids with enteral nutrition: a better therapeutic strategy for severe alcoholic hepatitis? Results of a pilot study. Eur J Gastroenterol Hepatol 2004;16:1375-1380. 15618848.


273. Spahr L, Rubbia-Brandt L, Pugin J, Giostra E, Frossard JL, Borisch B, et al. Rapid changes in alcoholic hepatitis histology under steroids: correlation with soluble intercellular adhesion molecule-1 in hepatic venous blood. J Hepatol 2001;35:582-589. 11690703.


275. Ramond MJ, Poynard T, Rueff B, Mathurin P, Theodore C, Chaput JC, et al. A randomized trial of prednisolone in patients with severe alcoholic hepatitis. N Engl J Med 1992;326:507-512. 1531090.


276. Imperiale TF, McCullough AJ. Do corticosteroids reduce mortality from alcoholic hepatitis? A meta-analysis of the randomized trials. Ann Intern Med 1990;113:299-307. 2142869.


277. Mathurin P, Mendenhall CL, Carithers RL Jr, Ramond MJ, Maddrey WC, Garstide P, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol 2002;36:480-487. 11943418.


278. Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: glucocorticosteroids for alcoholic hepatitis--a Cochrane Hepato-Biliary Group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther 2008;27:1167-1178. 18363896.


279. Louvet A, Wartel F, Castel H, Dharancy S, Hollebecque A, Canva-Delcambre V, et al. Infection in patients with severe alcoholic hepatitis treated with steroids: early response to therapy is the key factor. Gastroenterology 2009;137:541-548. 19445945.


280. Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, Durand F, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med 2011;365:1790-1800. 22070476.


281. Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology 2000;119:1637-1648. 11113085.


282. Doherty GM, Jensen JC, Alexander HR, Buresh CM, Norton JA. Pentoxifylline suppression of tumor necrosis factor gene transcription. Surgery 1991;110:192-198. 1858029.

284. Kim DJ, Suk KT, Park SH, Tak WY, Yim HJ, Um SH, et al. Short-term survival in patients with severe alcoholic hepatitis treated with pentoxifylline vs. corticosteroid: a non-inferiority trial. - a preliminary report. [Abstract]. J Hepatol 2013;58(Suppl 1):S219-S220.

285. Sidhu SS, Goyal O, Singla P, Gupta D, Sood A, Chhina RS, et al. Corticosteroid plus pentoxifylline is not better than corticosteroid alone for improving survival in severe alcoholic hepatitis (COPE trial). Dig Dis Sci 2012;57:1664-1671. 22388710.


286. Louvet A, Diaz E, Dharancy S, Coevoet H, Texier F, Thevenot T, et al. Early switch to pentoxifylline in patients with severe alcoholic hepatitis is inefficient in non-responders to corticosteroids. J Hepatol 2008;48:465-470. 18164508.


287. Parker R, Armstrong MJ, Corbett C, Rowe IA, Houlihan DD. Systematic review: pentoxifylline for the treatment of severe alcoholic hepatitis. Aliment Pharmacol Ther 2013;37:845-854. 23489011.


288. Spahr L, Rubbia-Brandt L, Frossard JL, Giostra E, Rougemont AL, Pugin J, et al. Combination of steroids with infliximab or placebo in severe alcoholic hepatitis: a randomized controlled pilot study. J Hepatol 2002;37:448-455. 12217597.


289. Naveau S, Chollet-Martin S, Dharancy S, Mathurin P, Jouet P, Piquet MA, et al. A double-blind randomized controlled trial of infliximab associated with prednisolone in acute alcoholic hepatitis. Hepatology 2004;39:1390-1397. 15122768.


291. Moreno C, Langlet P, Hittelet A, Lasser L, Degre D, Evrard S, et al. Enteral nutrition with or without N-acetylcysteine in the treatment of severe acute alcoholic hepatitis: a randomized multicenter controlled trial. J Hepatol 2010;53:1117-1122. 20801542.


292. Nguyen-Khac E, Thevenot T, Piquet MA, Benferhat S, Goria O, Chatelain D, et al. Glucocorticoids plus N-acetylcysteine in severe alcoholic hepatitis. N Engl J Med 2011;365:1781-1789. 22070475.


293. Burra P, Senzolo M, Adam R, Delvart V, Karam V, Germani G, et al. Liver transplantation for alcoholic liver disease in Europe: a study from the ELTR (European Liver Transplant Registry). Am J Transplant 2010;10:138-148. 19951276.


294. Waki K, Tamura S, Sugawara Y, Yamashiki N, Kadowaki T, Kokudo N. An analysis of the OPTN/UNOS Liver Transplant Registry. Clin Transpl 2009;55-64. 20524276.

295. Dumortier J, Guillaud O, Adham M, Boucaud C, Delafosse B, Bouffard Y, et al. Negative impact of de novo malignancies rather than alcohol relapse on survival after liver transplantation for alcoholic cirrhosis: a retrospective analysis of 305 patients in a single center. Am J Gastroenterol 2007;102:1032-1041. 17313502.


296. Mackie J, Groves K, Hoyle A, Garcia C, Garcia R, Gunson B, et al. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transpl 2001;7:418-427. 11349262.


297. Burra P, Mioni D, Cecchetto A, Cillo U, Zanus G, Fagiuoli S, et al. Histological features after liver transplantation in alcoholic cirrhotics. J Hepatol 2001;34:716-722. 11434618.


298. Tomé S, Martinez-Rey C, Gonzalez-Quintela A, Gude F, Brage A, Otero E, et al. Influence of superimposed alcoholic hepatitis on the outcome of liver transplantation for end-stage alcoholic liver disease. J Hepatol 2002;36:793-798. 12044530.


299. Lucey MR, Schaubel DE, Guidinger MK, Tome S, Merion RM. Effect of alcoholic liver disease and hepatitis C infection on waiting list and posttransplant mortality and transplant survival benefit. Hepatology 2009;50:400-406. 19472315.


300. Poynard T, Naveau S, Doffoel M, Boudjema K, Vanlemmens C, Mantion G, et al. Evaluation of efficacy of liver transplantation in alcoholic cirrhosis using matched and simulated controls: 5-year survival. Multi-centre group. J Hepatol 1999;30:1130-1137. 10406193.


301. Vanlemmens C, Di Martino V, Milan C, Messner M, Minello A, Duvoux C, et al. Immediate listing for liver transplantation versus standard care for Child-Pugh stage B alcoholic cirrhosis: a randomized trial. Ann Intern Med 2009;150:153-161. 19189904.


302. Lucey MR, Brown KA, Everson GT, Fung JJ, Gish R, Keeffe EB, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg 1997;3:628-637. 9404965.


303. Everhart JE, Beresford TP. Liver transplantation for alcoholic liver disease: a survey of transplantation programs in the United States. Liver Transpl Surg 1997;3:220-226. 9346743.


304. Pfitzmann R, Schwenzer J, Rayes N, Seehofer D, Neuhaus R, Nussler NC. Long-term survival and predictors of relapse after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl 2007;13:197-205. 17205563.


305. Perney P, Bismuth M, Sigaud H, Picot MC, Jacquet E, Puche P, et al. Are preoperative patterns of alcohol consumption predictive of relapse after liver transplantation for alcoholic liver disease? Transpl Int 2005;18:1292-1297. 16221161.


306. De Gottardi A, Spahr L, Gelez P, Morard I, Mentha G, Guillaud O, et al. A simple score for predicting alcohol relapse after liver transplantation: results from 387 patients over 15 years. Arch Intern Med 2007;167:1183-1188. 17563028.


309. Schmeding M, Heidenhain C, Neuhaus R, Neuhaus P, Neumann UP. Liver transplantation for alcohol-related cirrhosis: a single centre long-term clinical and histological follow-up. Dig Dis Sci 2011;56:236-243. 20499174.


310. Jauhar S, Talwalkar JA, Schneekloth T, Jowsey S, Wiesner RH, Menon KV. Analysis of factors that predict alcohol relapse following liver transplantation. Liver Transpl 2004;10:408-411. 15004769.


311. DiMartini A, Day N, Dew MA, Javed L, Fitzgerald MG, Jain A, et al. Alcohol consumption patterns and predictors of use following liver transplantation for alcoholic liver disease. Liver Transpl 2006;12:813-820. 16528710.


312. Björnsson E, Olsson J, Rydell A, Fredriksson K, Eriksson C, Sjoberg C, et al. Long-term follow-up of patients with alcoholic liver disease after liver transplantation in Sweden: impact of structured management on recidivism. Scand J Gastroenterol 2005;40:206-216. 15764153.


313. Faure S, Herrero A, Jung B, Duny Y, Daures JP, Mura T, et al. Excessive alcohol consumption after liver transplantation impacts on long-term survival, whatever the primary indication. J Hepatol 2012;57:306-312. 22521352.


314. Pageaux GP, Bismuth M, Perney P, Costes V, Jaber S, Possoz P, et al. Alcohol relapse after liver transplantation for alcoholic liver disease: does it matter? J Hepatol 2003;38:629-634. 12713874.


315. Biselli M, Gramenzi A, Del Gaudio M, Ravaioli M, Vitale G, Gitto S, et al. Long term follow-up and outcome of liver transplantation for alcoholic liver disease: a single center case-control study. J Clin Gastroenterol 2010;44:52-57. 19581813.


317. Zetterman RK. Liver transplantation for alcoholic liver disease. Clin Liver Dis 2005;9:171-181. 15763235.


318. Wells JT, Said A, Agni R, Tome S, Hughes S, Dureja P, et al. The impact of acute alcoholic hepatitis in the explanted recipient liver on outcome after liver transplantation. Liver Transpl 2007;13:1728-1735. 18044757.


319. Singal AK, Bashar H, Anand BS, Jampana SC, Singal V, Kuo YF. Outcomes after liver transplantation for alcoholic hepatitis are similar to alcoholic cirrhosis: exploratory analysis from the UNOS database. Hepatology 2012;55:1398-1405. 22213344.


320. Zanus G, Carraro A, Vitale A, Gringeri E, D'Amico F, Valmasoni M, et al. Alcohol abuse and de novo tumors in liver transplantation. Transplant Proc 2009;41:1310-1312. 19460548.


321. Haagsma EB, Hagens VE, Schaapveld M, van den Berg AP, de Vries EG, Klompmaker IJ, et al. Increased cancer risk after liver transplantation: a population-based study. J Hepatol 2001;34:84-91. 11211912.


322. Park HW, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. De novo malignancies after liver transplantation: incidence comparison with the Korean cancer registry. Transplant Proc 2012;44:802-805. 22483500.


323. Mezey E. Commentary on the hypermetabolic state and the role of oxygen in alcohol-induced liver injury. Recent Dev Alcohol 1984;2:135-141. 6374779.


324. Orrego H, Blake JE, Blendis LM, Compton KV, Israel Y. Long-term treatment of alcoholic liver disease with propylthiouracil. N Engl J Med 1987;317:1421-1427. 3317042.


325. Rambaldi A, Gluud C. Propylthiouracil for alcoholic liver disease. Cochrane Database Syst Rev 2002;CD002800. 12076451.


326. Fede G, Germani G, Gluud C, Gurusamy KS, Burroughs AK. Propylthiouracil for alcoholic liver disease. Cochrane Database Syst Rev 2011;CD002800. 21678335.


327. Morgan TR, Weiss DG, Nemchausky B, Schiff ER, Anand B, Simon F, et al. Colchicine treatment of alcoholic cirrhosis: a randomized, placebo-controlled clinical trial of patient survival. Gastroenterology 2005;128:882-890. 15825072.


328. Kershenobich D, Uribe M, Suarez GI, Mata JM, Perez-Tamayo R, Rojkind M. Treatment of cirrhosis with colchicine. A double-blind randomized trial. Gastroenterology 1979;77:532-536. 378754.


329. Kershenobich D, Vargas F, Garcia-Tsao G, Perez Tamayo R, Gent M, Rojkind M. Colchicine in the treatment of cirrhosis of the liver. N Engl J Med 1988;318:1709-1713. 3287167.


330. Rambaldi A, Gluud C. Colchicine for alcoholic and non-alcoholic liver fibrosis and cirrhosis. Cochrane Database Syst Rev 2005;CD002148. 15846629.


331. Li J, Kim CI, Leo MA, Mak KM, Rojkind M, Lieber CS. Polyunsaturated lecithin prevents acetaldehyde-mediated hepatic collagen accumulation by stimulating collagenase activity in cultured lipocytes. Hepatology 1992;15:373-381. 1371980.


332. Lieber CS, Robins SJ, Li J, DeCarli LM, Mak KM, Fasulo JM, et al. Phosphatidylcholine protects against fibrosis and cirrhosis in the baboon. Gastroenterology 1994;106:152-159. 8276177.


333. Lieber CS, Weiss DG, Groszmann R, Paronetto F, Schenker S. II. Veterans Affairs Cooperative Study of polyenylphosphatidylcholine in alcoholic liver disease. Alcohol Clin Exp Res 2003;27:1765-1772. 14634492.


336. Mato JM, Camara J, Fernandez de Paz J, Caballeria L, Coll S, Caballero A, et al. S-adenosylmethionine in alcoholic liver cirrhosis: a randomized, placebo-controlled, double-blind, multicenter clinical trial. J Hepatol 1999;30:1081-1089. 10406187.


337. Rambaldi A, Gluud C. S-adenosyl-L-methionine for alcoholic liver diseases. Cochrane Database Syst Rev 2006;CD002235. 16625556.


338. Caballería J, Pares A, Bru C, Mercader J, Garcia Plaza A, Caballeria L, et al. Spanish Group for the Study of Alcoholic Fatty Liver. Metadoxine accelerates fatty liver recovery in alcoholic patients: results of a randomized double-blind, placebo-control trial. J Hepatol 1998;28:54-60. 9537864.


339. Kim MY, Cho MY, Baik SK, Jeong PH, Suk KT, Jang YO, et al. Beneficial effects of candesartan, an angiotensin-blocking agent, on compensated alcoholic liver fibrosis - a randomized open-label controlled study. Liver Int 2012;32:977-987. 22364262.


340. Llorent L, Richaud-Patin Y, Alcocer-Castillejos N, Ruiz-Soto R, Mercado MA, Orozco H, et al. Cytokine gene expression in cirrhotic and non-cirrhotic human liver. J Hepatol 1996;24:555-563. 8773910.


341. Austin AS, Mahida YR, Clarke D, Ryder SD, Freeman JG. A pilot study to investigate the use of oxpentifylline (pentoxifylline) and thalidomide in portal hypertension secondary to alcoholic cirrhosis. Aliment Pharmacol Ther 2004;19:79-88. 14687169.


342. Li Z, Yang S, Lin H, Huang J, Watkins PA, Moser AB, et al. Probiotics and antibodies to TNF inhibit inflammatory activity and improve nonalcoholic fatty liver disease. Hepatology 2003;37:343-350. 12540784.


343. Yokota T, Oritani K, Takahashi I, Ishikawa J, Matsuyama A, Ouchi N, et al. Adiponectin, a new member of the family of soluble defense collagens, negatively regulates the growth of myelomonocytic progenitors and the functions of macrophages. Blood 2000;96:1723-1732. 10961870.


344. Rambaldi A, Jacobs BP, Iaquinto G, Gluud C. Milk thistle for alcoholic and/or hepatitis B or C virus liver diseases. Cochrane Database Syst Rev 2005;CD003620. 15846671.


345. Ferenci P, Dragosics B, Dittrich H, Frank H, Benda L, Lochs H, et al. Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J Hepatol 1989;9:105-113. 2671116.


346. Rambaldi A, Jacobs BP, Iaquinto G, Gluud C. Milk thistle for alcoholic and/or hepatitis B or C liver diseases--a systematic cochrane hepato-biliary group review with meta-analyses of randomized clinical trials. Am J Gastroenterol 2005;100:2583-2591. 16279916.


347. Alcohol Project Supporting Commitee. National Alcohol Harm Reduction Strategy 2020. Seoul: Jung-moon Press; 2011. p. 2.
349. Chung WJ, Lee SM, Kim JY. Socioeconomic costs if alcohol drinking in Korea. Seoul: Jipmoonddang; 2009. p. 229-235.
350. Ministry of Health and Welfare. National Alcohol Policy: Blue Bird Plan 2020. Seoul: Ministry of Health and Welfare; 2011. p. 27-36.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




