Serum bilirubin levels are inversely associated with nonalcoholic fatty liver disease
Article information
Abstract
Background/Aims
Serum bilirubin exerts antioxidant and cytoprotective effects. In addition, elevated serum bilirubin levels are associated with a decreased risk of metabolic and cardiovascular diseases. However, few studies have evaluated whether serum bilirubin is associated with non-alcoholic fatty liver disease (NAFLD), which is closely associated with other metabolic diseases. The aim of this study was thus to elucidate the association between serum total bilirubin levels and NAFLD.
Methods
A cross-sectional study of 17,348 subjects undergoing a routine health check-up was conducted. Subjects positive for hepatitis B or hepatitis C virus, or with other hepatitis history were excluded. NAFLD was diagnosed on the basis of typical ultrasonographic findings and an alcohol consumption of less than 20 g/day.
Results
The mean age of the subjects was 49 years and 9,076 (52.3%) were men. The prevalence of NAFLD decreased steadily as the serum bilirubin level increased in both men and women (P<0.001 for both). Multivariate regression analysis adjusted for other metabolic risk factors showed that serum bilirubin level was inversely associated with the prevalence of NAFLD [odds ratio (OR)=0.88, 95% confidence interval (CI)=0.80-0.97]. Furthermore, there was an inverse, dose-dependent association between NAFLD and serum total bilirubin levels (OR=0.83, 95% CI=0.75-0.93 in the third quartile; OR=0.80, 95% CI=0.71-0.90 in the fourth quartile vs. lowest quartile, P for trend <0.001).
Conclusions
Serum bilirubin levels were found to be inversely associated with the prevalence of NAFLD independent of known metabolic risk factors. Serum bilirubin might be a protective marker for NAFLD.
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) has been recognized as the most common liver disease, with an estimated prevalence of 20-30%.1,2 NAFLD includes a spectrum of hepatic dysfunctions ranging from simple steatosis to nonalcoholic steatohepatitis (NASH), cirrhosis and hepatocellular carcinoma.3 NAFLD is also closely related to insulin resistance, obesity, dyslipidemia, type 2 diabetes, and coronary artery disease.4 Therefore, it is considered to be a hepatic manifestation of metabolic syndrome.5,6
Although the pathogenic mechanisms that result in the development of NAFLD remain unknown, oxidative stress has been suggested as an etiopathogenic mechanism in NAFLD.7-9 Previous studies showed that the administration of the free radical-generating azo compound to mice or rats induced fat accumulation in the liver by increasing triacylglycerol and decreasing phospholipid.10-12 In addition, fat accumulation in the liver was suppressed through the simultaneous administration of free radical-scavenging antioxidants.11 Therefore, several antioxidant agents, such as vitamin E, have been suggested to be an effective treatment option.13
Serum bilirubin, the end product of heme catabolism, has potent antioxidant and cytoprotective effects.14,15 At the molecular level, bilirubin scavenges peroxyl radicals, hydroxyl radicals, and reactive nitrogen species.14 In this way, it prevents the oxidation of intracellular lipids.16 Several lines of clinical evidence strongly support the beneficial cytoprotective effects of bilirubin. Higher bilirubin levels are inversely associated with insulin level, insulin resistance, and diabetes.17,18 Elevated bilirubin levels are also related to the reduced risk of cardiovascular diseases, including coronary artery disease, stroke, and peripheral vessel disease.19,20
Therefore, it can be hypothesized that high serum bilirubin can reduce oxidative stress, decrease inflammation, and decrease the risk of NAFLD. However, only a few studies have been conducted on the association between the serum bilirubin level and NAFLD.21-23 Therefore, we conducted a large-scale cross-sectional study to evaluate the association between NAFLD and serum bilirubin level in an apparently healthy population.
PATIENTS AND METHODS
Study populations
A total of 21,130 subjects visited the Seoul National University Hospital Gangnam Healthcare Center (Seoul, Republic of Korea) for a routine health check-up between January 2006 and December 2006. Among the total subjects, 21,128 subjects over 18 years old who underwent a serum bilirubin level test and abdominal ultrasonography were initially selected. Then, we excluded participants with other potential causes of chronic liver disease, including those with excessive alcohol consumption (≥20 g/day), those with hepatitis B virus (determined by the presence of hepatitis B surface antigen), those with hepatitis C virus (determined by the presence of hepatitis C antibody), or those with some other history of hepatitis, as identified by detailed medical history taking and a questionnaire (Wilson's disease, hemochromatosis, autoimmune hepatitis, and primary biliary cirrhosis). We also excluded subjects who had taken medications known to have a potential to provoke fatty liver in the past year. Subjects with chronic medical diseases, such as coronary artery disease, and malignancy were also excluded. Finally, 17,348 participants were included for analysis. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Review Board of Seoul National University Hospital.
Clinical and laboratory assessments
Each participant completed a questionnaire, an anthropometric assessment, and laboratory tests on the same day. The presence of diabetes mellitus was defined as either a fasting serum glucose level equal to or greater than 126 mg/dL or taking anti-diabetic medication. The presence of hypertension was defined as having a systolic blood pressure over 140 mmHg or diastolic blood pressure over 90 mmHg or taking anti-hypertensive medication. Current smokers were defined as those who had smoked at least one cigarette per day during the previous year.
Height and body weight were measured using a digital scale, with subjects wearing a light gown. The body mass index (BMI) was calculated as follows: BMI=weight (kg)/height squared (m2). Waist circumference was measured using a tape measure to the nearest millimeter at the midpoint between the lower costal margin and the iliac crest by a well-trained examiner. Systolic and diastolic blood pressures were measured twice on the same day, and the mean values were used in the analysis.
Laboratory examinations included serum bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), total cholesterol, fasting glucose, hepatitis B surface antigen, and an antibody to hepatitis C virus. Blood samples were collected from all participants before 10 AM after a 12-h overnight fast. All of the biochemical determinations were carried out in the same laboratory using standard laboratory methods.
According to the revised NCEP criteria,24 an individual was diagnosed as having metabolic syndrome if he or she has three or more of the following criteria: 1) waist circumference >90 cm in men and >80 cm in women using the International Obesity Task Force criteria for the Asian-Pacific population to determine waist circumference25; 2) triglycerides ≥150 mg/dL or medication use; 3) HDL cholesterol <40 mg/dL in men and <50 mg/dL in women or medication use; 4) blood pressure ≥130/85 mmHg or antihypertensive medication use; and 5) fasting glucose ≥100 mg/dL or medication use (insulin or oral agents).
Serum bilirubin level
Fasting serum total bilirubin was measured with an automated Architect ci8200 Integrated System (Abbott Laboratories, Abbott Park, IL, USA) with the vanadate oxidation method. An elevated serum total bilirubin level was defined as a fasting serum total bilirubin level >1.2 mg/dL (upper reference levels used at Seoul National University Hospital). In addition, serum bilirubin levels were divided into quartiles both in men and women. In men, total bilirubin quartile 1 included participants with serum bilirubin levels ≤0.8 mg/dL, quartile 2 was 0.9-1.0 mg/dL, quartile 3 was 1.1-1.4 mg/dL, and quartile 4 was ≥1.5 mg/dL. In women, quartile 1 of serum bilirubin level was serum bilirubin ≤0.6 mg/dL, quartile 2 was 0.7-0.8 mg/dL, quartile 3 was 0.9-1.0 mg/dL, and quartile 4 was ≥1.1 mg/dL.
Ultrasonographic examinations
NAFLD was defined as the presence of fatty liver by ultrasonography (US), in the absence of the following: (1) excessive alcohol intake (≥20 g/day), (2) positivity for hepatitis B surface antigen or an antibody to hepatitis C virus, (3) known etiologies of liver disease, and (4) medications known to produce fatty liver. Hepatic US examinations were carried out by experienced radiologists who were blinded to the clinical and laboratory details of participants at the time of the procedure. The diagnosis of fatty liver was performed by US (Acuson, Sequoia 512, Siemens, Mountain View, CA) using previously described standardized criteria.4
Statistical analysis
A chi-square test for categorical variables and Student's t-test or ANOVA for continuous variables were used to compare variables between subjects with and without NAFLD and among subjects according to quartiles of serum bilirubin levels as appropriate. Variables with P value <0.05 in the univariate analyses and known risk factors were included in the multivariate logistic regression analysis. All statistical analyses were conducted using SPSS 19 (SPSS Inc., Chicago, IL, USA). A two-tailed P value <0.05 was regarded to be statistically significant.
RESULTS
Among the 17,348 participants (9,076 men and 8,272 women; mean ages, 50.1±11.6 and 48.7±11.5 years, respectively), 5,768 had US-diagnosed NAFLD. The baseline characteristics of subjects with and without NAFLD according to sex are shown in Table 1. The factors found to be significantly associated with NAFLD in the univariate analyses were as follows: higher BMI, higher waist circumference, higher blood pressure, elevated AST, ALT, total cholesterol, fasting glucose, and the presence of diabetes, hypertension, and metabolic syndrome (P<0.001, respectively). Serum total bilirubin level was also significantly lower in NAFLD group (P<0.001).

Clinical, anthropometric, and biochemical parameters of NAFLD subjects and controls stratified according to sex
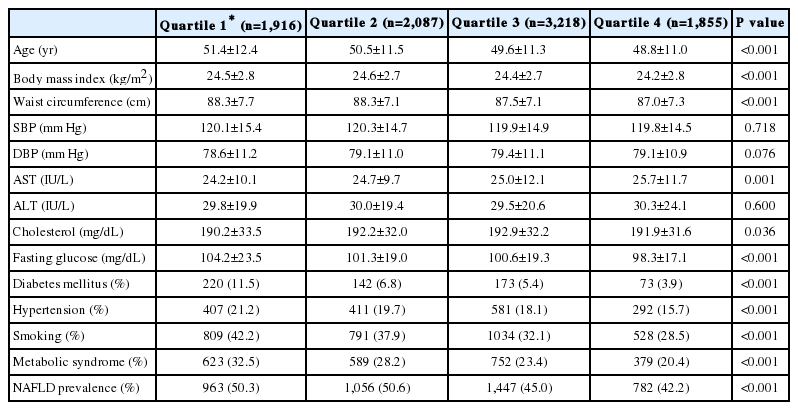
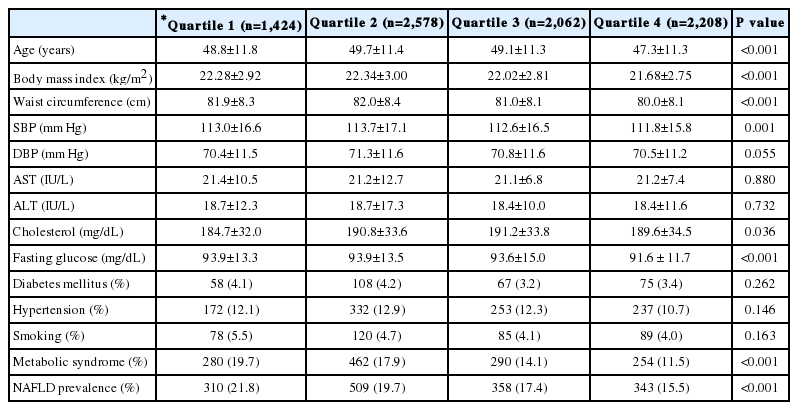
Table 2 and Table 3 show characteristics according to the quartiles of serum bilirubin level in men and women, respectively. Consistent to our expectation, increasing serum total bilirubin level was associated with a less severe metabolic profile including lower BMI, lower waist circumference, lower serum cholesterol, fasting glucose level and lower prevalence of metabolic syndrome (P<0.05, both in men and women). Also, increasing levels of serum total bilirubin were significantly associated with a decreasing prevalence of NAFLD (P for trend <0.001, respectively, Fig. 1). In addition, multivariate regression analysis showed that NAFLD was significantly associated with the grade of total serum bilirubin levels in a dose-dependent manner [odds ratio (OR) 0.80, 95% confidence interval (CI), 0.71-0.90 in the 4th quartile; OR 0.83, 95% CI 0.75-0.93 in the 3rd quartile vs. the 1st quartile, P for trend <0.001, Table 4].

Prevalence of NAFLD in men and women according to quartiles of the serum total bilirubin level. Participants in quartiles 1-4 had serum bilirubin levels of ≤0.8, 0.9-1.0, 1.1-1.4, and ≥1.5 mg/dL, respectively, among men, and ≤0.6, 0.7-0.8, 0.9-1.0, and ≥1.1 mg/dL among women. *P for trend <0.001.
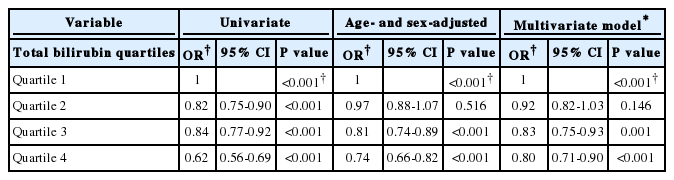
Univariate and multivariate ORs of risk factors for the presence of NAFLD relative to the spectrum of total bilirubin levels
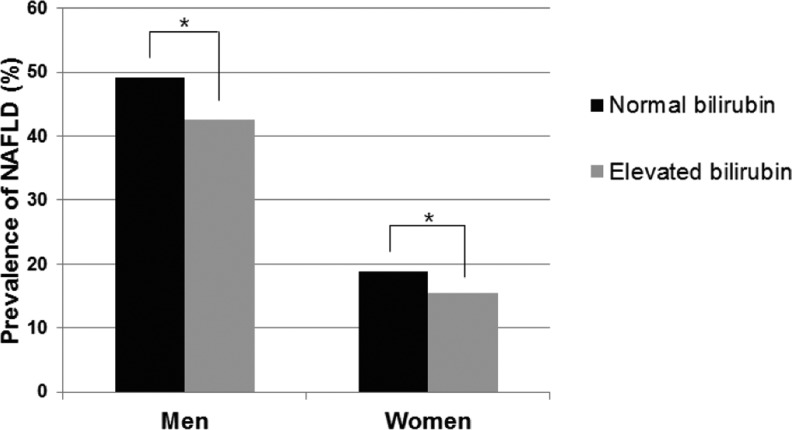
When we divided serum bilirubin levels into groups with normal levels (≤1.2 mg/dL) and elevated levels (>1.2 mg/dL), the prevalence of NAFLD was significantly lower in groups with elevated bilirubin in both sex groups (P<0.001, respectively, Fig. 2). In multivariate logistic model, subjects with abnormally elevated serum bilirubin levels had a 13% lower possibility of having NAFLD than those with normal serum bilirubin levels (OR 0.87, 95% CI, 0.80-0.95, P=0.002). Also, when serum bilirubin level was analyzed as a continuous variable, the fully adjusted model consistently revealed an inverse relationship between serum total bilirubin level and the prevalence of NAFLD (OR 0.88, 95% CI, 0.80-0.97). An increase of 1 mg/dL of bilirubin was associated with a 12% decrease in the possibility of NAFLD.
DISCUSSION
The main finding of this large-scale study was an inverse association between the serum bilirubin level and the prevalence of NAFLD. The prevalence of NAFLD was significantly lower in subjects with elevated serum bilirubin levels. Additionally, the serum total bilirubin level was found to be inversely related to NAFLD in a dose-dependent manner regardless of known metabolic risk factors.
Recent clinical data have shown that elevated serum bilirubin levels are associated with a lower prevalence of oxidative stress-mediated diseases. Serum bilirubin has consistently been demonstrated to be negatively correlated to cardiovascular diseases, including coronary artery disease, peripheral atherosclerotic disease and ischemic stroke,26-29 and their risk factors, including hypertension, diabetes mellitus, metabolic syndrome, and obesity.30 As NAFLD is closely related to cardiovascular diseases and metabolic risk factors,4,31-33 it can be assumed that NAFLD is also negatively associated with serum bilirubin levels. However, there have been only a few studies on the correlation between the serum bilirubin level and NAFLD; therefore, it is hard to draw a consistent conclusion. Kumar et al23 showed that patients with unconjugated hyperbilirubinemia had significantly less severe liver disease, and Hjelkrem et al22 showed that patients with NASH had a significantly lower prevalence of unconjugated hyperbilirubinemia. However, the study population of these studies was too small to draw a conclusion. Recently, Chang et al showed an inverse relationship between the serum direct bilirubin level and the incidence of NAFLD. However, their cohort included only middle-aged Korean men.21 Therefore, it is difficult to generalize these results to the general population of both men and women. Our study showed that the serum bilirubin level is inversely associated with US-diagnosed NAFLD in an apparently healthy large-scale population.
Serum bilirubin has anti-oxidant and cytoprotective effects.14,15 Previous experimental research also supports the role of bilirubin as a protective marker of NAFLD. Hemeoxygenase-1 (HO-1) is a stress-responsive protein that leads to the degradation of prooxidant heme to biliverdin, which is subsequently converted to the antioxidant bilirubin.34 HO-1 can interrupt the progression of steatohepatitis in both in vitro and in vivo models by inducing an antioxidant pathway, suppressing the production of cytokines, and modifying fatty acid turnover.35 Therefore, bilirubin, the final product of HO-1, is also hypothesized to be a protective marker of NAFLD progression, although further study is warranted on the exact role of bilirubin in NAFLD progression.
Gilbert's syndrome, the most common inherited disorder of bilirubin glucuronidation presenting as unconjugated hyperbilirubinemia, is more commonly diagnosed in men. The underlying mechanism has been attributed to different effects of sex steroids on bilirubin metabolism and a relatively higher level of daily bilirubin production in men.36 Consistent with previous study results, elevated serum bilirubin was more common in men (34.8%) than women (13.8%) in this study. To identify differences between sexes, we evaluated the association of NAFLD and serum bilirubin level in men and women separately. Our study showed consistent results of an inverse association between serum bilirubin levels and NAFLD in both men and women.
This study has some limitations. First, because of its cross-sectional design, a causal relationship between serum bilirubin level and NAFLD could not be identified. Second, we did not determine unconjugated bilirubin and conjugated bilirubin separately in this study. As these two types of bilirubin have different characteristics, they may have different associations with NAFLD. Third, we used US for the diagnosis of NAFLD without histologic confirmation of the liver, which is regarded as the gold standard for the diagnosis of NAFLD. Therefore we could not differentiate simple steatosis from NASH, in which oxidative stress has more roles. In spite of these limitations, this study has several advantages. First, our sample size is large, even after subdividing to explore differences between sex. Second, the participants in our study are regarded to be representative of the general population based on a health check-up policy.
In conclusion, our study suggests that elevated serum bilirubin levels are inversely associated with the prevalence of NAFLD independent of known metabolic risk factors in a large healthy population. Serum total bilirubin might be a protective marker for NAFLD.
Acknowledgements
This research was supported by The GlaxoSmithKline Research Fund of the Korean Association for the study of the Liver.
Notes
The authors have no conflicts to disclose.
Abbreviations
ALT
alanine aminotransferase
AST
aspartate aminotransferase
BMI
body mass index
CI
confidence interval
HO-1
heme oxygenase-1
NAFLD
non-alcoholic fatty liver disease
NASH
non-alcoholic steatohepatitis
OR
odds ratio
US
ultrasonography