| Clin Mol Hepatol > Volume 21(2); 2015 > Article |
ABSTRACT
Background/Aims
Methods
Results
Abbreviations
REFERENCES
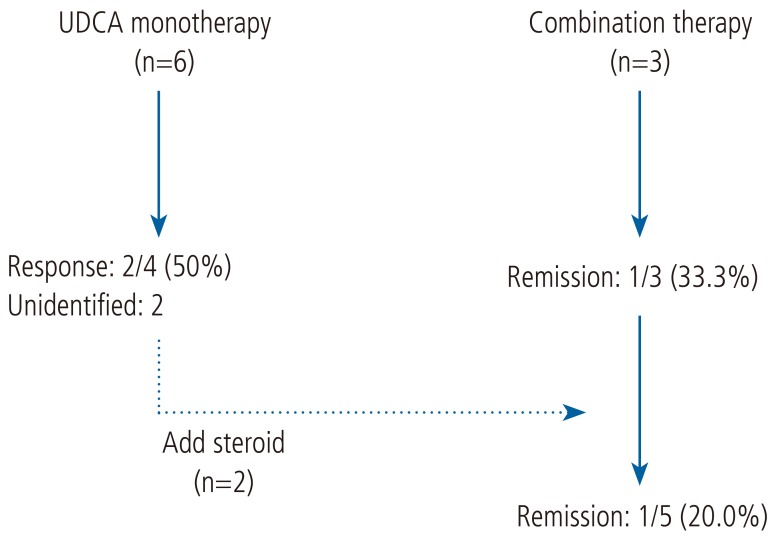
Figure┬Ā1
Treatment progress of patients with AIH-PBC overlap syndrome. UDCA, ursodeoxycholic acid; AIH, autoimmune hepatitis; PBC, primary biliary cirrhosis.
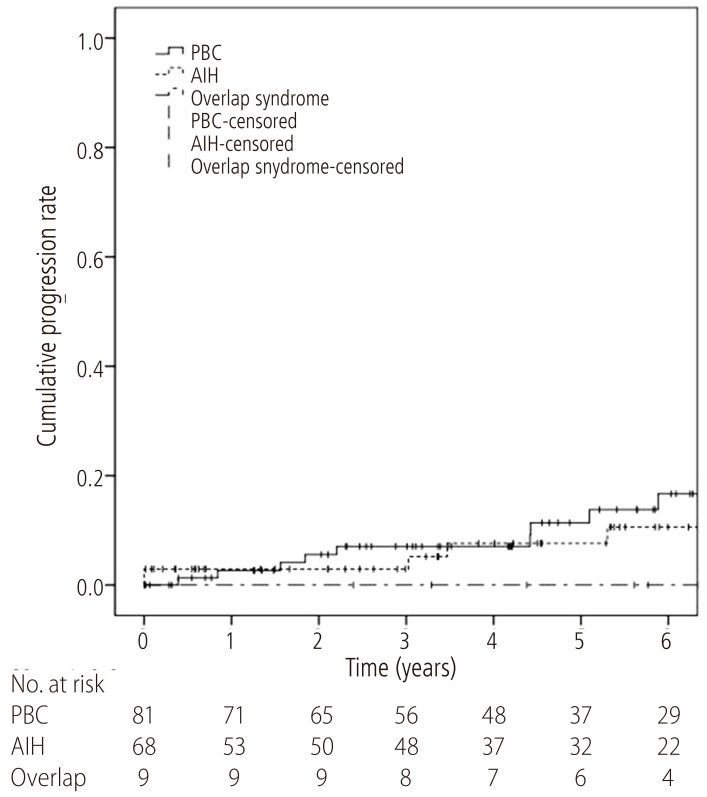
Figure┬Ā2
Time-to-progression curves of liver cirrhosis for patients with AIH-PBC overlap syndrome (dash-dotted line), PBC (solid line), and AIH (dashed line). The 1-year and 5-year progression rate were 3.4% and 24.4%, respectively, for the PBC patients, 4.7% and 9.8% for the AIH patients, and 0.0% and 34.4% for the AIH-PBC overlap syndrome patients. Liver cirrhosis developed significantly faster in patients with AIH-PBC overlap syndrome than in the AIH patients (P=0.013). The progression rate of the AIH-PBC overlap syndrome patients did not differ significantly from that of the PBC patients (P=0.163). AIH, autoimmune hepatitis; PBC, primary biliary cirrhosis.

Figure┬Ā3
Time-to-progression curves of hepatic decompensation for patients with AIH-PBC overlap syndrome (dash-dotted line), PBC (solid line), and AIH (dashed line). The progression curve for AIH-PBC patients (1-year and 5-year progression rates both 0.0%) did not differ from that of PBC patients (1-year and 5-year progression rates of 2.7% and 11.4%, respectively; P=0.740) or AIH patients (1-year and 5-year progression rates of 2.9% and 7.6%, respectively; P=0.996). AIH, autoimmune hepatitis; PBC, primary biliary cirrhosis.
Table┬Ā1.
Baseline characteristics of the patients with AIH, PBC, and AIH-PBC overlap syndrome
| PBC (n=81) | AIH (n=68) | Overlap syndrome (n=9) | |
|---|---|---|---|
| Sex (M/F) | 13/68 | 6/62 | 0/9 |
| Age (years) | 53 (27-69) | 50 (20-70) | 49 (25-69) |
| Follow-up time (years) | 4.7 (0.0-12.4) | 5.3 (0.0-12.7) | 5.8 (2.4-13.0) |
| AST (IU/L) | 65 (24-419) | 180 (31-1,530) | 132 (53-448)* |
| ALT (IU/L) | 70 (11-485) | 172 (19-3,260) | 116 (39-319)* |
| ALP (IU/L) | 265 (59-810) | 128 (44-305) | 361 (119-570)ŌĆĀ |
| GGT (IU/L) | 361 (156-1,405) | 112 (23-771) | 418 (179-616)ŌĆĀ |
| PT (INR) | 0.97 (0.85-1.70) | 1.12 (0.84-3.17) | 0.94 (0.81-1.17)ŌĆĀ |
| Albumin (g/dL) | 4.2 (2.5-4.7) | 3.7 (2.2-4.9) | 4.1 (3.0-4.6)ŌĆĪ |
| Bilirubin (mg/dL) | 0.9 (0.4-15.4) | 1.6 (0.4-28.4) | 1.1 (0.4-2.7) |
| IgG (mg/dL) | 1636 (1011-2,892) | 2306 (1,129-6,860) | 2242 (1,880-3,235) |
| IgM (mg/dL) | 533 (255-982) | 187 (47-941) | 225 (146-1,344) |
| AMA (positive/total) | 81/81 (100%) | 4/59 (6.8%) | 6/9 (66.7%)*, ŌĆĀ |
| ANA (positive/total) | 27/58 (46.6%) | 55/67 (82.1%) | 9/9 (100%)* |
| SMA (positive/total) | 2/50 (4.0%) | 24/68 (35.3%) | 1/9 (11.1%) |
| Liver cirrhosis at diagnosis (cirrhosis/total) | 19/81 (23.5%) | 15/68 (22.0%) | 1/9 (11.1%) |
Data are presented as the median (min-max) or number/total (percent).
AIH, autoimmune hepatitis; ALP, alkaline phosphatase; ALT, alanine transaminase; AMA, antimitochondrial antibody; ANA, antinuclear antibody; AST, aspartate transaminase; GGT, gamma-glutamyl transpeptidase; IgG, immunoglobulin G; IgM, immunoglobulin M; INR, international normalized ratio; PBC, primary biliary cirrhosis; PT, prothrombin time; SMA, anti-smooth muscle antibody.
Table┬Ā2.
Detailed characteristics of the patients with AIH-PBC overlap syndrome
| Patient number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Sex | F | F | F | F | F | F | F | F | F |
| Age (yr) | 25 | 62 | 49 | 36 | 69 | 47 | 49 | 51 | 62 |
| Follow-up (yr) | 13.0 | 7.8 | 5.6 | 4.4 | 8.0 | 2.4 | 6.4 | 5.8 | 3.3 |
| Initial diagnosis | AIH | AIH | AIH | Both | AIH | PBC | AIH | PBC | PBC |
| AST (IU/L) | 132 | 166 | 69 | 137 | 448 | 171 | 53 | 71 | 121 |
| ALT (IU/L) | 221 | 251 | 93 | 193 | 319 | 116 | 39 | 111 | 71 |
| ALP (IU/L) | 361 | 270 | 119 | 340 | 127 | 526 | 570 | 376 | 562 |
| GGT (IU/L) | 338 | 545 | 279 | 542 | 179 | 616 | 233 | 425 | 418 |
| Albumin (g/dL) | 4.1 | 4.2 | 4.1 | 4.0 | 3.0 | 4.2 | 3.7 | 4.6 | 4.3 |
| PT (INR) | 0.96 | 0.92 | 0.94 | 0.84 | 1.17 | 0.81 | 0.97 | 1.01 | 0.85 |
| Bilirubin (mg/dL) | 0.9 | 0.7 | 0.4 | 1.4 | 2.7 | 1.9 | 0.6 | 1.1 | 1.3 |
| IgG (mg/dL) | 3235 | 1880 | - | 1933 | 2775 | - | - | - | 2242 |
| IgM (mg/dL) | 146 | 225 | - | 203 | 1344 | - | - | - | 494 |
| AMA | - | O | O | O | - | - | O | O | O |
| ANA | 1:320 | 1:320 | 1:320 | + | 1:320 | 1:320 | 1:160 | 1:320 | + |
| SMA | O | - | - | - | - | - | - | - | - |
| Treatment | CombŌĆĪ | CombŌĆĪ | U>C┬¦ | U>C┬¦ | CombŌĆĪ | UDCA | UDCA | UDCA | UDCA |
| UDCA response | N/A | N/A | N/A | R | N/A | N/A | R | N | N |
| Steroid response | I | I | I | I | R | N/A | N/A | N/A | N/A |
| Progression to liver cirrhosis | O | O* | - | - | O | - | O | N/AŌĆĀ | - |
| Histological findings | |||||||||
| ŌĆāInterface hepatitis | O | O | O | O | O | O | O | O | - |
| ŌĆāLymphocytic infiltration | N/A | O | O | N/A | O | O | O | O | O |
| ŌĆāRossetting | - | - | - | - | - | - | - | - | - |
| ŌĆāBile duct lesion | O | - | - | O | O | O | - | O | O |
A positive test for AMA means at least 1:20; A positive test for ANA means at least 1:40; A positive test for SMA means at least 1:80.
AIH, autoimmune hepatitis; ALP, alkaline phosphatase; ALT, alanine transaminase; AMA, antimitochondrial antibody; ANA, antinuclear antibody; AST, aspartate transaminase; F, female; GGT, gamma-glutamyl transpeptidase; IgG, immunoglobulin G; IgM, immunoglobulin M; INR, international normalized ratio; PBC, primary biliary cirrhosis; PT, prothrombin time; SMA, anti-smooth muscle antibody; UDCA, ursodeoxycholic acid; N/A, not available; R, remission or response; I, incomplete response; N, no response.
Table┬Ā3.
Numbers of patients who achieved response or remission with each therapy
| UDCA* | SteroidŌĆĀ | CombinationŌĆĀ | |
|---|---|---|---|
| PBC | 47/65 (72.3%) | - | 3/3 (100%) |
| AIH | 6/8 (75.0%) | 34/45 (75.6%)ŌĆĪ | - |
| Overlap syndrome | 2/4 (50.0%) | - | 1/5 (20.0%)ŌĆĪ |
- TOOLS



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




