| Clin Mol Hepatol > Volume 20(3); 2014 > Article |
ABSTRACT
Methimazole and propylthiouracil have been used in the management of hyperthyroidism for more than half a century. However, hepatotoxicity is one of the most deleterious side effects associated with these medications. The mechanism(s) of hepatic injury induced by antithyroid agents is not fully recognized yet. Furthermore, there are no specific tools for predicting the occurrence of hepatotoxicity induced by these drugs. The purpose of this article is to give an overview on possible susceptibility factors in liver injury induced by antithyroid agents. Age, gender, metabolism characteristics, alcohol consumption, underlying diseases, immunologic mechanisms, and drug interactions are involved in enhancing antithyroid drugs-induced hepatic damage. An outline on the clinically used treatments for antithyroid drugs-induced hepatotoxicity and the potential therapeutic strategies found to be effective against this complication are also discussed.
A large number of drugs have deleterious effects on liver and drug-induced liver injury (DILI) is a major clinical problem. Actually, drugs are responsible for a large number of cases of acute liver failure.1 Acetaminophen accounts for the approximately half of cases of DILI in the United States.2 In other world's regions, for instance in developing countries, other drugs such as antituberculosis medications might be the leading cause of DILI.3 In some cases of DILI such as acetaminophen-induced hepatotoxicity, the mechanism of liver injury is fairly well understood, hepatic damage is dose dependent, and the toxicity is reproducible in animal models. In contrast, a large number of other drugs have been associated with liver injury which their mechanisms of hepatotoxicity are less elucidated. Characteristically, these types of DILI are uncommon, not obviously related to drug dose, and multifactorial dependent; therefore, these reactions are termed 'idiosyncratic' DILI (IDILI).4 Many drugs have been identified to cause IDILI in humans.5 Antithyroid drugs-induced hepatic injury is categorized as IDILI.6
Due to its high morbidity and mortality, and unpredictable nature, DILI has become a major clinical challenge.7 Moreover, DILI accounts for a large number of drug withdrawals from the marketplace, or discontinuation of further development of a drug candidate. Hence, DILI not only cause patient hospitalization and sometimes need for liver transplantation and even death, but also involve the loss of potentially useful drugs.
Elucidating the mechanisms of toxicity and probable susceptibility factors which make patients vulnerable to DILI, will lead us to the safer pharmaceuticals development and reducing adverse drug reactions (ADRs).
Antithyroid drugs are chemically thioamide derivatives which are used more than 60 years for managing hyperthyroid patients. Methimazole and propylthiouracil (PTU) are two frequently used antithyroid agents in different countries. Despite the great effects of these drugs in controlling hyperthyroidism, their administration is associated with hepatotoxicity as a serious side effect.8,9 Hepatic injury induced by these agents could be so severe that might lead to hepatic failure and requirement for liver transplantation,10,11,12 and even death has been reported in some cases.13,14
Liver transaminase abnormality, that might indicate subclinical liver injury, is a common event after PTU administration.12,15 Kim et al. reported that asymptomatic elevation of serum ALT developed in 14.3% of investigated patients in a single center retrospective study.16 Yun et al. suggested that PTU therapy might be continued with caution in the presence of elevated liver transaminases, when no hyperbilirubinemia is present.15 However, regular monitoring of liver biochemistry has been suggested to allow discontinuation of PTU in suspected cases of hepatic injury.15,17 The diagnosis of PTU hepatotoxic effect should always be suspected in the patient receiving PTU therapy in whom clinical or biochemical evidence of acute hepatitis develops. The frequency of PTU-related severe liver damage is approximately 0.1% based on the available data.16,18 Nakamura et al. found a very high incidence of elevation of transaminase values with PTU in comparison with methimazole.19 Methimazole-induced hepatotoxicity usually develops in the first few weeks of drug consumption with an estimated incidence of 0.1-0.2%.6,20
The figure of hepatic injury induced by antithyroid agents seems different according the histopathological findings. The pattern of liver injury induced by methimazole is predominantly as cholestatic type,21,22,23 where those induced by PTU is of hepatocellular type in most cases.20,24,25 Pathologic findings of PTU-induced hepatic injury in human subjects revealed that this drug caused parenchymal necrosis with hemorrhage, collapse of lobular architecture, and preportal mixed inflammatory infiltrate.26 Hepatic abnormalities associated with methimazole are typical of a cholestatic process.22 Biopsy specimens from patients with methimazole-induced hepatic injury showed oedema and inflammation of portal tract with intracanalicular cholestasis and moderate microvascular steatosis.27,28
Fewer studies on the mechanisms and the pathogenesis of liver damage induced by these drugs are available. The mechanisms by which methimazole and/or PTU cause hepatotoxicity are not clarified completely yet, but it seems that these mechanisms might be different between currently available antithyroid drugs.29 Furthermore, the risk factors that render patients more susceptible to antithyroid drugs-induced hepatic injury are not fully recognized.
There are numerous factors that can contribute to differences among individuals in their sensitivity to xenobiotics. These include variation in age, gender, chemical metabolism in liver, underlying disease, coexposure to additional xenobiotics, and dietary status. Moreover, environmental and genetic factors have the capacity to apply significant influences on the onset of these determinants. The presence of susceptibility factors might make patients vulnerable to hepatic injury induced by xenobiotics (Fig. 1) and non-toxic chemical (e.g drugs) might become hepatotoxic in lower doses in the presence of risk factors (Fig. 1).
The following is a review of data supporting different hypotheses on the factors which might influence antithyroid drugs-induced hepatic injury. In addition, an outline on the therapeutic strategies against antithyroid drugs-induced hepatotoxicity is given here.
Drugs are generally transformed to biologically inactive structures and eliminated from the body, chiefly by hepatic metabolism. However, certain drugs undergo biotransformation to metabolites that can interfere with cellular functions. Drugs such as acetaminophen, tamoxifen,30 isoniazid,31,32 and amodiaquine33,34 are good examples of reactive, and possibly hepatotoxic, metabolite forming xenobiotics. The main theme of this section is to review the evidence for reactive intermediates as factors for antithyroid drugsinduced hepatotoxicity. Moreover, the role of variation in drug metabolizing enzymes between different individuals and its possible impact on the hepatic injury induced by these drugs is discussed here.
Methimazole is metabolized through cytochrome P450 (CYP) enzymes35,36 and flavoprotein mixed-function oxidase (FMO).37,38 Methimazole metabolism through CYP450 enzymes gives N-methylthiourea and glyoxal as two major metabolites.36 Nmethylthiourea is further oxidized with FMO enzyme to give sulfinic and sulfenic acid species.38 Glyoxal, is a reactive compound capable of interacting with different intracellular targets, such as proteins.39 Sulfenic acids are high electrophilic species that form irreversible adduct with cellular nucleophilic sites,40 and may have a role in methimazole-induced hepatotoxicity. N-methylthiourea is proposed to be the main methimazole reactive metabolite responsible for the hepatotoxicity induced by this drug.36 But, we recently showed that glyoxal also might has an important role in cellular injury induced by methimazole in an in vitro model of isolated rat hepatocytes.41
PTU is metabolized by glucuronidation in liver and prepared to exert from body (Fig. 2).42 In another study, the methylated and sulfate conjugate PTU was detected in rat urine.43 No PTU-related reactive metabolite(s) has been suggested yet to induce hepatotoxic reactions. But, it has been founded that myeloperoxidase (MPO)-mediated metabolism of PTU led to a reactive metabolite formation which covalently bounded to leukocytes proteins.44 This reactions might be responsible for agranulocytosis as a deleterious adverse effect of PTU.44,45
Many variations in drug metabolizing enzymes in humans has been identified.46 As methimazole is suspected to metabolized to reactive intermediate(s) which might involve in the hepatic injury induced by this drug,36,41 polymorphism in drug metabolizing enzymes might has a role in the idiosyncratic nature of the hepatic injury induced by this antithyroid medication. The exact CYP enzyme involved in methimazole and/or PTU metabolism is not characterized yet, hence further investigations are required to elucidate the possible role of enzyme variation in the hepatotoxicity induced by these drugs. Moreover, future investigations could focus on the possibility of reactive metabolite formation during PTU biotransformation in liver.
As mentioned, glucuronidation is a one of the metabolic pathways for antithyroid drugs (especially PTU) to preparing them for excretion (Fig. 2).42 The polymorphism in uridine diphosphoglucuronosyl transferase enzymes (UGTs) activity is also identified between human populations.47 Hence, another proposed mechanism for hepatotoxicity induced by antithyroid agents could be attributed to their impaired detoxification process, due to lower activity of UGTs. Consequently, some populations might be at a greater risk for these drugs to induce hepatic injury.
The selenium-containing analogues of antithyroid drugs are synthesized, and seems to have some advantages in comparison to their sulfur containing counterparts.48,49 These compounds could be newer antithyroid drug candidates. Since some investigations mentioned a potential role for "sulfur" atom in antithyroid agents to induce toxicity during metabolism,50 substituting "sulfur" with "selenium" might reduce the risk of antithyroid drugs-induced liver injury. However, the possibility if their serious adverse effects such as hepatotoxicity is lower than conventional drugs, remains to be elucidated in more future investigations.
Some investigations mentioned the critical role of cellular defense mechanisms such as glutathione (GSH) in preventing antithyroid drugsinduced hepatotoxicity.41,51,52 On the other hand, the liver GSH content might be variable in different situations. For example, it has been proven that liver GSH reservoirs are lower in malnourished patients53 and/or in some pathophysiological conditions such as alcoholism,54 so it seems that the risk of methimazole hepatotoxicity might be highest in these situations. Hence, particular attention should be given to the possibility that unexpected toxic reactions may be encountered under conditions of tissue GSH depletion. Physicians might advise their patient to avoiding alcohol consumption during antithyroid therapy.
The role of immune system in xenobiotics-induced hepatotoxicity is discussed in previous investigations.55 Immune-mediated reactions are suggested to play a role in antithyroid drug-induced hepatotoxicity.56 Although the mechanism(s) underlying this event is not fully elucidated yet 56, but cytokines are thought to play a role in immunemediated liver injury caused by methimazole.56 Cytokines could play an important role in DILI.57,58 Hence, another possible mechanism(s) for antithyroid drugsinduced hepatotoxicity could be immune system-mediated. The release of cytokines and autoantibodies are reported in antithyroid drugs-treated patients and/or laboratory animals.56,59 It has been shown that cytokine-mediated liver injury could has a critical role in methimazole-treated mice.56 Furthermore, some cases of PTU-induced hepatic damage are reported in which autoantibodies are demonstrated.60 Lymphocyte sensitization in a patient with neonatal liver injury probably by placental transfer of PTU has been reported.61 All these reports are in line with the hypothesis that patient immune system might play a role in the pathogenesis of hepatic injury induced by antithyroid medications. Antineutrophil cytoplasmic antibody (ANCA) positive cases are usually connected with deleterious immune system-mediated side effects such as vasculitis and autoimmune hepatitis induced by antithyroid medications.62,63 The presence of other autoantibodies such as preneuclear antineutrophil cytoplasmic antibody and antimyeloperoxidase antineutrophil cytoplasmic antibody all indicate that the immune system might be involved in antithyroid drugs side effects.64,65
"Hapten hypothesis" is an intriguing theory for immune-mediated drugs-induced hepatotoxicity.66 According to this hypothesis, reactive intermediates of different drugs, undergo covalent binding with different cellular proteins. The drug-protein complex is then recognized by immune system and consequently the activation of this system might led to hepatotoxicity.67 As mentioned, the reactive metabolites of antithyroid agents are capable of interacting with different targets including proteins. Hence, these modified proteins might act as haptens and consequently stimulate the immune system.
Recently an increasing interest has been made to new experimental models for studying idiosyncratic drug induced liver injury. "Drug-inflammation interaction" is one of these models.68 In this model, it is proposed that a modest inflammation will enhance some drugs induced hepatotoxicity.69 Evaluating antithyroid drugs-induced hepatotoxicity in such new experimental models, could be the subject of future investigations to elucidate the precise mechanism(s) of liver injury induced by these drugs.
It should be noted that PTU was widely used in the past in an attempt to treat alcohol-induced liver complications and severe alcoholic hepatitis.70,71 However, the beneficial effects of PTU against alcoholism appeared quite limited.70,71 Since alcoholism and alcohol-induced liver injury is an inflammatory-mediated process at least in part,72 one may argue that PTU might hasten liver injury in these patients. Although it seems that PTU doesn't increase liver-related events when it was investigated for treating alcoholic liver disease,71 but as many effective therapeutic options are developed against ethanol-induced liver injury,73 PTU administration against this complication seems to be just an antiquated and ineffective strategy. The interrelationship between inflammatory processes, PTU-induced hepatotoxicity and the druginflammationinteraction theory in alcoholic liver disease need more in depth experimental investigations.
Age is a risk factor for drug-induced hepatotoxicity from specific medications.3 Younger age is a risk factor for particular medications such as valproic acid and aspirin.74 In contrast, older ages might be more susceptible to some other medications such as isoniazid,75 amoxicillin/clavulanate,76 erythromycin,3 and many other drugs.
Some comparative evaluation of adverse events including hepatotoxicity, related to antithyroid drugs has been done previously.29,77,78 In these investigations, the authors tried to find a relationship between the age of patients and the development of hepatotoxicity induced by methimazole and/or PTU. One of these investigations resulted that methimazole administration caused lower severe hepatotoxic events and vasculitis in children than the other drug, PTU.29 Interestingly, it has been reported that there are no reports of liver failure or liver transplantation in association with methimazole use in children in united states.11 Furthermore, there are fewer and less serious adverse events reported in FDA database for methimazole than for PTU.11 A substantial amount of data obtained from evidence based and prospective studies are indicated that methimazole is a safer pharmaceutical in management of hyperthyroidism in children.11,79 Some severe and even fatal PTU-induced liver injury cases are reported in children treated with this medication.80,81 Hence, some investigators suggested that PTU should no longer be used as a first line treatment for Graves' disease in children.11 Some studies showed that a shift in propylthiouracil prescription has occurred during years (Fig. 3) and methimazole is more prescribed in lower ages,78 probably due to its lower risk of liver damage in children.29,78
Although increased number of reports of severe propylthiouracil-induced hepatic injury in children favors methimazole administration (Fig. 3), but this doesn't mean that methimazole is completely safe in pediatrics.82 The mechanisms of hepatotoxicity induced by antithyroid drugs are not fully elucidated yet, and methimazole-induced liver injury categorized as an idiosyncratic reaction,6 hence physicians should be aware of this side effect in all age ranges including child's which in them might be a misconception about methimazole safety.
As the mechanism(s) of antithyroid drugs-induced hepatotoxicity is unknown completely yet, it is impossible to draw specific conclusions, but some probable hypothesis which differ pediatric and older patients in the sensitivity to antithyroid drugs is given below.
Besides the simple explanation that with increasing age the average consumption of drugs is higher (including multiple medications) and the risk for an additional disease that could influence the manifestation of idiosyncratic DILI is greater in older patients, there are other reasons based on a mechanistic base. For example, mitochondrial function (which is a frequent intracellular target of many drugs) is gradually weakening with advancing age, and cumulative oxidative damage to mitochondria keeps surging.83 Thus, oxidative damage to mitochondria is a critical factor of susceptibility. It seems that antithyroid drugs affect cellular mitochondria to induce cellular damage.41,84 On the other hand, significant differences in pharmacokinetic, and pharmacodynamics and enzymology are evident in pediatrics.85 These factors might bring this population different from older patients and antithyroid drugs hepatotoxic profile might be different in them. In addition, the variability in the activity of different enzymes which are responsible for the detoxification process of electrophilic species, namely glutathione transferase enzymes (GSTs), might also be involved in the different responses to antithyroid medications between adults and children.86 The critical role of glutathione in detoxification of antithyroid drugs is discussed in more details at next sections.
Although the choice of hyperthyroidism drug therapy might be a matter of clinicians' personal preference, but different factors such as patients' age should be noticed. Differences in the side effect profile of antithyroid drugs, might favor methimazole in children. On the other hand, methimazole should be administered cautiously in older persons with an appropriate dose, not only because of the concern for higher rate of agranulocytosis,87 but also probably because of more susceptibility of these patients to the hepatic injury induced by this drug.88
In conclusion, no clear and direct relationship between patients' age and antithyroid agents-induced hepatotoxicity has been founded yet, except for a higher rate of PTU-induced liver damage in pediatrics by an unknown mechanism(s).
Generally, drugs-induced hepatotoxicity is more prevalent in females.89 A large retrospective study has recognized that 76% of all patients who developed severe liver failure due to drugs were females.1 No clear reason has been identified for this increased susceptibility to many different drugs in women. Although more drugs are consumed by women as compared to men, and, although for some of the (dose-dependent) cases of DILI differences in the volume of distribution or drug-metabolizing enzyme expression have been suggested to account for the gender differences, there remains a significant part of all DILI cases where the sex-dependent increase in risk cannot be explained by increased exposure.90 Some authors has found no sex differences related to antithyroids-induced hepatotoxicity.82
Hyperthyroidism is more common in women91 and it has been found that the incidence of grave's disease is more frequent in females.92 Hence, any probable relationship between patients, sex and antithyroid drugs-induced hepatotoxicity might be simply due to the more rate of antithyroid drug prescription in females.
Drug-induced hepatotoxicity can be affected by drug interactions. Generally, drug interactions occur when two drugs are co-administered and both are metabolized by the same CYP450. But, in another situation when a drug toxic metabolite is responsible for hepatotoxic reactions, coadministration of enzyme-inducing agents might deteriorate its hepatotoxic properties. Previously we showed that methimazole becomes severely hepatotoxic in enzyme-induced mice.52 This mentioned the importance of reactive metabolites in methimazoleinduced toxicity. Furthermore, other drugs with enzyme-inducing properties such as carbamazepine, isoniazid, etc. might interact with methimazole to lead hepatotoxic reactions. Hence, we might be able to propose that, the authorities should be cautious about coadministrating the drugs with hepatic enzymeinducing properties, such as phenobarbital, with antithyroid medications.
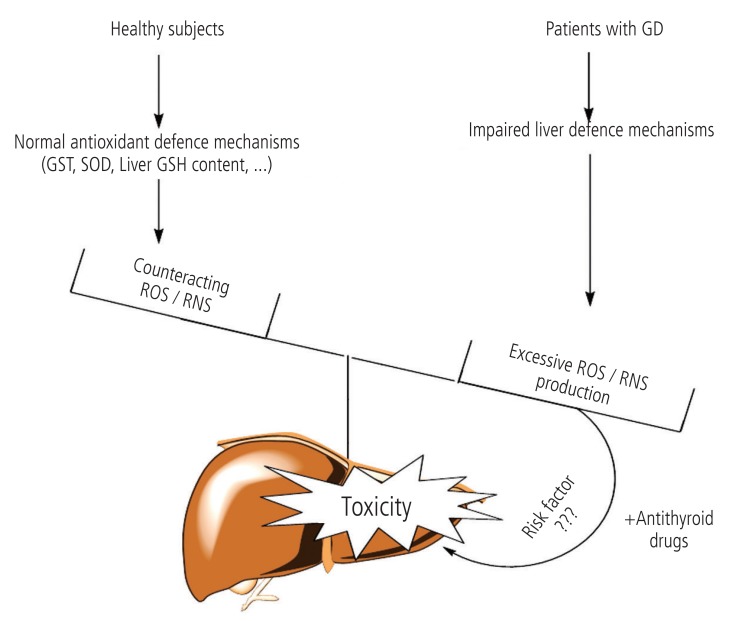
Several different disorders can cause hyperthyroidism. Graves' disease (GD), is the most common cause of hyperthyroidism in humans.93 Many investigations have been carried out on the complications which occur in hyperthyroid patients with GD. It has been shown that, the activity of different enzymes which are involved in the antioxidant defense mechanism of liver, are changed in hyperthyroidism.94 Komosinska et al. showed that glutathione reductase (GR) activity, was lower in hyperthyroid patients.95 In another investigation it has been observed that oxidative stress occurred in liver tissue of hyperthyroid animals probably due to impaired antioxidant defense mechanisms.96,97 As antithyroid drugsinduced hepatotoxicity is deteriorated in experimental models with defected liver protective mechanisms,41,51 the question arises if GD (the disease which antithyroid drugs are prescribed against) can sensitize individuals to the antithyroid medications' adverse hepatic effects (Fig. 4). The hypothesis that GD itself has a role in antithyroid drugs-induced hepatic injury, needs more controlled and in depth investigations to be clarified.
In many cases of antithyroid drugs-induced hepatic injury, no standard and specific treatment is available, except of drug discontinuation and monitoring patients' liver function during hospitalization.27,98 The most performed laboratory tests in antithyroid drugs-induced hepatotoxicity cases, are liver function tests as evaluated by serum aminotransferase levels (AST & ALT) and alkaline phosphatase (ALP) activity.8,99 Other assessments involve serum bilirubin, white blood cells count, prothrombin time (PT), and serum thyroid hormones and TSH levels.99,100 Moreover, abdominal ultrasonography is done to detect any cholestatic changes of patients' liver.6 Drug-induced hepatic injury could be certainly proven when other interacting factors such as viral hepatitis are ruled out.
Patients should be aware of symptoms which might indicate antithyroid drugs-induced hepatic injury. Indeed, all antithyroid taking patients must be trained to report symptoms such as abdominal discomfort and pain in upper right quadrant and other signs such as urine discoloration, which are connected to serious adverse reactions such as hepatotoxicity. As patients observed any of these symptoms, they must discontinue the medication and refer to their physician immediately. Liver biochemistry should be checked in clinically suspected cases.
As mentioned, no other medical intervention except for drug cessation and liver function monitoring has been made in the most cases of antithyroid drugs-induced hepatotoxicity.8,27,98 However, intra vascular glutathione was founded to be an effective treatment in a case of methimazole-induced hepatotoxicity and lowered transaminase levels in the patient.99 As mentioned, glutathione (GSH) has been proven to play a critical role in preventing methimazole-induced hepatic injury in different experimental models.41,51,52 Hence, using glutathione in patients with methimazole-induced liver injury seems to be a reasonable choice. In another study by Becker et al., it has been reported that corticosteroids might alleviate methimazoleinduced hepatitis.101 In another case, prednisolone administration rapidly recovered the patient from jaundice induced by antithyroid medications.102
Different protective agents have been identified to be effective against methimazole-induced hepatotoxicity in experimental models. For example we previously showed that organosulfur compounds103 and the amino acid, taurine,104 could ameliorate the toxic insult caused by methimazole. In another in vivo study, we showed that Nacetyl cysteine (NAC) successfully prevented methimazole-induced hepatic injury in different experimental conditions.52 These new protective strategies might help to develop a useful hepatoprotective agent against antithyroid drugs-induced liver injury in humans.
Sixty years after antithyroid drugs introduction, these medications continue to be important in managing hyperthyroidism, but because of their potentially serious side effects such as hepatotoxicity, there is concern about their administration especially in pediatrics. This mentioned the need to consider the development of alternative antithyroid agents, in order to minimize the risk of hepatotoxicity and possible fatal outcome. Considering the development of newer antithyroid drugs with safer profile of toxicity is the need of hour. Some studies are conducted to synthesis newer analogues of currently available antithyroid agents.105,106,107 Taking more attention to the biological implications of these molecules, and testing their pharmacological actions in animal models, can lead to the development of newer and safer drugs for hyperthyroidism therapy. Moreover, elucidating the exact mechanism(s) of toxicity induced by antithyroid medications will lead us to better management of the developed hepatotoxic reactions.
Although methimazole has been reported to show a better overall safety profile than PTU, but considering probable susceptibility factors could give a better insight in its hepatotoxic profile and consequently reduce its adverse effects (Fig. 5). Some proposed risk factors which might make patients more vulnerable to methimazole-induced hepatotoxicity are summarized in Figure 5.
Recently, new models have been used to understand and predict drug-induced hepatotoxicity. Novel animal models such as lipopolysaccharide (LPS)-rodent model,108 and/or Sod +/- mouse model,109 are experimental tools to investigate about IDILI. The hepatotoxicity induced by antithyroid medications could be the subject of future studies in these novel experimental models, to improve our understanding of the clinical spectrum and mechanism of liver injury induced by these agents.
Clinical use of methimazole and PTU as convenient antithyroid medications are associated with the serious side effect of hepatotoxicity. Methimazole has been the most prescribed antithyroid drug these years (Fig. 3). Factors such as higher potency, convenient daily dosing, and the better toxic profile, might cause methimazole to be a more preferred drug in managing hyperthyroid patients (Fig. 3). But, physicians should be aware that methimazole can be associated with hepatotoxicity. Hence, considering susceptibility factors which might bring a person more vulnerable to antithyroid drugs-induced liver injury, might bright a better view on hyperthyroidism treatment and lowering the adverse drug reactions (Fig. 5). Patients who take antithyroid drugs should be advised for the risk of liver injury and be aware of possible susceptibility factors such as alcohol consumption, which might hasten liver damage induced by their antithyroid medications.
Acknowledgments
The authors thank Dr. David Cooper (Professor of Medicine, Division of Endocrinology, Diabetes, & Metabolism, The Johns Hopkins University, School of Medicine) for his kind permission to reprint Figure 3.
REFERENCES
1. Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug induced liver injury in the United States. Liver Transpl 2004;10:1018-1023. 15390328.


2. Watkins PB, Seeff LB. Drug-induced liver injury: Summary of a single topic clinical research conference. Hepatology 2006;43:618-631. 16496329.


3. Bell LN, Chalasani N. Epidemiology of idiosyncratic drug-induced liver injury. Semin Liver Dis 2009;29:337-347. 19826967.




4. Hussaini SH, Farrington EA. Idiosyncratic drug-induced liver injury: an overview. Expert Opin Drug Saf 2007;6:673-684. 17967156.


5. Bissell DM, Gores GJ, Laskin DL, Hoofnagle JH. Drug-induced liver injury: Mechanisms and test systems. Hepatology 2001;33:1009-1013. 11283870.


7. Watkins PB. Idiosyncratic liver injury: challenges and approaches. Toxicol Pathol 2005;33:1-5. 15805049.


10. Kang H, Choi JD, Jung IG, Kim DW, Kim TB, Shin HK, et al. A case of methimazole-induced acute hepatic failure in a patient with chronic hepatitis B carrier. Korean J Intern Med 1990;5:69-73. 2271514.



11. Rivkees SA, Mattison DR. Ending propylthiouracil-induced liver failure in children. N Engl J Med 2009;360:1574-1575. 19357418.

12. Williams KV, Nayak S, Becker D, Reyes J, Burmeister LA. Fifty years of experience with propylthiouracil-associated hepatotoxicity: what have we learned? J Clin Endocrinol Metab 1997;82:1727-1733. 9177371.


13. Carrion AF, Czul F, Arosemena LR, Selvaggi G, Garcia MT, Tekin A, et al. Propylthiouracil-induced acute liver failure: role of liver transplantation. Int J Endocrinol 2010;2010:910636. 21234410.




14. Malozowski S, Chiesa A. Propylthiouracil-induced hepatotoxicity and death. Hopefully, never more. J Clin Endocrinol Metab 2010;95:3161-3163. 20610609.




15. Liaw YF, Huang MJ, Fan KD, Li KL, Wu SS, Chen TJ. Hepatic injury during propylthiouracil therapy in patients with hyperthyroidism: a cohort study. Ann Intern Med 1993;118:424-428. 8439116.


16. Kim HJ, Kim BH, Han YS, Yang I, Kim KJ, Dong SH, et al. The incidence and clinical characteristics of symptomatic propylthiouracil-induced hepatic injury in patients with hyperthyroidism: a single-center retrospective study. Am J Gastroenterol 2001;96:165-169. 11197248.


17. Hanson JS. Propylthiouracil and hepatitis: two cases and a review of the literature. Arch Intern Med 1984;144:994-996. 6608933.


18. Cooper DS, Rivkees SA. Putting propylthiouracil in perspective. J Clin Endocrinol Metab 2009;94:1881-1882. 19401361.



19. Nakamura H, Noh JY, Itoh K, Fukata S, Miyauchi A, Hamada N, et al. Comparison of methimazole and propylthiouracil in patients with hyperthyroidism caused by Graves' disease. J Clin Endocrinol Metab 2007;92:2157-2162. 17389704.



22. Arab DM, Malatjalian DA, Rittmaster RS. Severe cholestatic jaundice in uncomplicated hyperthyroidism treated with methimazole. J Clin Endocrinol Metab 1995;80:1083-1085. 7714072.


23. Schwab GP, Wetscher GJ, Vogl W, Redmond E. Methimazole-induced cholestatic liver injury, mimicking sclerosing cholangitis. Langenbecks Arch Chir 1996;381:225-227. 8817448.


24. Limaye A, Ruffolo PR. Propylthiouracil-induced fatal hepatic necrosis. Am J Gastroenterol 1987;82:152-154. 3812421.

25. Safani MM, Tatro DS, Rudd P. Fatal propylthiouracil-induced hepatitis. Arch Intern Med 1982;142:838-839. 7073426.

26. Carrion AF, Czul F, Arosemena LR, Selvaggi G, Garcia MT, Tekin A, et al. Propylthiouracil-induced acute liver failure: role of liver transplantation. Int J Endocrinol 2010;2010:910636. 21234410.




27. Gallelli L, Staltari O, Palleria C, De Sarro G, Ferraro M. Hepatotoxicity induced by methimazole in a previously healthy patient. Curr Drug Saf 2009;4:204-206. 19534646.


28. Hung YT, Yu WK, Chow E. Delayed cholestatic hepatitis due to methimazole. Hong Kong Med J 1999 6;5(2):200-201. 11821593.

29. Rivkees SA, Szarfman A. Dissimilar hepatotoxicity profiles of propylthiouracil and methimazole in children. J Clin Endocrinol Metab 2010;95:3260-3267. 20427502.



30. Fan PW, Bolton JL. Bioactivation of tamoxifen to metabolite E quinone methide: reaction with glutathione and DNA. Drug Metab Dispos 2001;29:891-896. 11353759.

31. Nelson SD, Mitchell JR, Timbrell JA, Snodgrass WR, Corcoran GB. Isoniazid and iproniazid: activation of metabolites to toxic intermediates in man and rat. Science 1976;193:901-903. 7838.


32. Heidari R, Babaei H, Eghbal MA. Cytoprotective effects of taurine against toxicity induced by isoniazid and hydrazine in isolated rat hepatocytes. Arh Hig Rada Toksikol 2013;64:15-24. 23819928.



33. Jewell H, Maggs JL, Harrison AC, O'Neill PM, Ruscoe JE, Park BK. Role of hepatic metabolism in the bioactivation and detoxication of amodiaquine. Xenobiotica 1995;25:199-217. 7618347.


34. Heidari R, Babaei H, Eghbal MA. Amodiaquine-induced toxicity in isolated rat hepatocytes and the cytoprotective effects of taurine and/or N-acetyl cysteine. Res Pharm Sci 2014;9:97-105.


35. Lee PW, Neal RA. Metabolism of methimazole by rat liver cytochrome P-450-containing monoxygenases. Drug Metab Dispos 1978;6:591-600. 30610.

36. Mizutani T, Yoshida K, Murakami M, Shirai M, Kawazoe S. Evidence for the involvement of N-methylthiourea, a ring cleavage metabolite, in the hepatotoxicity of methimazole in glutathione-depleted mice: structure-toxicity and metabolic studies. Chem Res Toxicol 2000;13:170-176. 10725113.


37. Poulsen LL, Hyslop RM, Ziegler DM. S-oxidation of thioureylenes catalyzed by a microsomal flavoprotein mixed-function oxidase. Biochem Pharmacol 1974;23:3431-3440. 4441423.


38. Kedderis GL, Rickert DE. Loss of rat liver microsomal cytochrome P-450 during methimazole metabolism. Role of flavin-containing monooxygenase. Drug Metab Dispos 1985;13:58-61. 2858378.

39. Shangari N, O'Brien PJ. The cytotoxic mechanism of glyoxal involves oxidative stress. Biochem Pharmacol 2004;68:1433-1442. 15345333.


40. Mansuy D, Dansette PM. Sulfenic acids as reactive intermediates in xenobiotic metabolism. Arch Biochem Biophys 2011;507:174-185. 20869346.


41. Heidari R, Babaei H, Eghbal M. Mechanisms of methimazole cytotoxicity in isolated rat hepatocytes. Drug Chem Toxicol 2013;36:403-411. 23256569.


42. Lindsay RH, Cash AG, Vaughn AW, Hill JB. Glucuronide conjugation of 6-n-propyl-2-thiouracil and other antithyroid drugs by guinea pig liver microsomes in vitro. Biochem Pharmacol 1977;26:617-623. 16610.


43. Lindsay RH, Hill JB, Kelly K, Vaughn A. Excretion of propylthiouracil and its metabolites in rat bile and urine. Endocrinology 1974;94:1689-1698. 4831131.



44. Lam DC, Lindsay RH. Oxidation and binding of [2-(14)C]propylthiouracil in human polymorhonuclear leukocytes. Drug Metab Dispos 1979;7:285-289. 40767.

45. Balkin MS, Buchholtz M, Ortiz J, Green AJ. Propylthiouracil (PTU)-induced agranulocytosis treated with recombinant human granulocyte colony-stimulating factor (G-CSF). Thyroid 1993;3:305-309. 7509672.


46. Ingelman-Sundberg M, Oscarson M, McLellan RA. Polymorphic human cytochrome P450 enzymes: an opportunity for individualized drug treatment. Trends Pharmacol Sci 1999;20:342-349. 10431214.


47. Miners JO, McKinnon RA, Mackenzie PI. Genetic polymorphisms of UDP-glucuronosyltransferases and their functional significance. Toxicology 2002;181:453-456. 12505351.


48. Taurog A, Dorris ML, Guziec LJ, Guziec FS Jr. The selenium analog of methimazole measurement of its inhibitory effect on type I 5'-deiodinase and of its antithyroid activity. Biochem Pharmacol 1994;48:1447-1453. 7524506.


49. Antoniadis CD, Blake AJ, Hadjikakou SK, Hadjiliadis N, Hubberstey P, Schroder M, et al. Structural characterization of selenium and selenium-diiodine analogues of the antithyroid drug 6-n-propyl-2-thiouracil and its alkyl derivatives. Acta Crystallogr B 2006;62:580-591. 16840807.



50. Brittebo EB. Metabolism-Dependent Toxicity of Methimazole in the Olfactory Nasal Mucosa. Pharmacol Toxicol 1995;76:76-79. 7753763.


51. Mizutani T, Murakami M, Shirai M, Tanaka M, Nakanishi K. Metabolism-dependent hepatotoxicity of methimazole in mice depleted of glutathione. J Appl Toxicol 1999;19:193-198. 10362270.


52. Heidari R, Babaei H, Roshangar L, Eghbal MA. Effects of Enzyme Induction and/or Glutathione Depletion on Methimazole-Induced Hepatotoxicity in Mice and the Protective Role of N-Acetylcysteine. Adv Pharm Bull 2014;4:21-28. 24409405.

53. Bray TM, Taylor CG. Tissue glutathione, nutrition, and oxidative stress. Can J Physiol Pharmacol 1993;71:746-751. 8313240.


54. Shaw S, Rubin KP, Lieber CS. Depressed hepatic glutathione and increased diene conjugates in alcoholic liver disease. Evidence of lipid peroxidation. Dig Dis Sci 1983;28:585-589. 6861588.


55. Liu ZX, Kaplowitz N. Immune-mediated drug-induced liver disease. Clin Liver Dis 2002;6:755-774. 12362579.


56. Kobayashi M, Higuchi S, Ide M, Nishikawa S, Fukami T, Nakajima M, et al. Th2 cytokine-mediated methimazole-induced acute liver injury in mice. J Appl Toxicol 2012;32:823-833. 22407903.


57. Diehl AM. Cytokine regulation of liver injury and repair. Immunol Rev 2000;174:160-171. 10807515.


58. Lacour S, Gautier JC, Pallardy M, Roberts R. Cytokines as potential biomarkers of liver toxicity. Cancer Biomark 2005;1:29-39. 17192030.


59. Thong HY, Chu CY, Chiu HC, others . Methimazole-induced antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis and lupus-like syndrome with a cutaneous feature of vesiculo-bullous systemic lupus erythematosus. Acta Derm Venereol 2002;82:206-208. 12353714.


60. Weiss M, Hassin D, Bank H. Propylthiouracil-induced hepatic damage. Arch Intern Med 1980;140:1184-1185. 6893265.


61. Hayashida CY, Duarte AJ, Sato AE, Yamashiro-Kanashiro EH. Neonatal hepatitis and lymphocyte sensitization by placental transfer of propylthiouracil. J Endocrinol Invest 1990;13:937-941. 2090674.


62. Maggiore G, Larizza D, Lorini R, De Giacomo C, Scotta MS, Severi F. Propylthiouracil hepatotoxicity mimicking autoimmune chronic active hepatitis in a girl. J Pediatr Gastroenterol Nutr 1989;8:547-548. 2723949.


63. Gunton JE, Stiel J, Caterson RJ, McElduff A. Clinical case seminar: Anti-thyroid drugs and antineutrophil cytoplasmic antibody positive vasculitis. A case report and review of the literature. J Clin Endocrinol Metab 1999;84:13-16. 9920055.


64. Bonaci-Nikolic B, Nikolic MM, Andrejevic S, Zoric S, Bukilica M. Antineutrophil cytoplasmic antibody (ANCA)-associated autoimmune diseases induced by antithyroid drugs: comparison with idiopathic ANCA vasculitides. Arthrit Res Ther 2005;7:R1072-R1081.



65. Sera N, Ashizawa K, Ando T, Abe Y, Ide A, Usa T, et al. Treatment with propylthiouracil is associated with appearance of antineutrophil cytoplasmic antibodies in some patients with Graves' disease. Thyroid 2000;10:595-599. 10958312.


67. Ju C, Uetrecht JP. Mechanism of idiosyncratic drug reactions: reactive metabolites formation, protein binding and the regulation of the immune system. Curr Drug Metab 2002;3:367-377. 12093356.


68. Ganey PE, Luyendyk JP, Maddox JF, Roth RA. Adverse hepatic drug reactions: inflammatory episodes as consequence and contributor. Chem Biol Interact 2004;150:35-51. 15522260.


69. Shaw PJ, Hopfensperger MJ, Ganey PE, Roth RA. Lipopolysaccharide and trovafloxacin coexposure in mice causes idiosyncrasy-like liver injury dependent on tumor necrosis factor-alpha. Toxicol Sci 2007;100:259-266. 17709330.



70. Fede G, Germani G, Gluud C, Gurusamy KS, Burroughs AK. Propylthiouracil for alcoholic liver disease. Cochrane Database Syst Rev 2011;(6):CD002800 doi: 10.1002/14651858. CD 002800.pub3. 21678335.



71. Tome S, Lucey MR. Review article: current management of alcoholic liver disease. Aliment Pharmacol Ther 2004;19:707-714. 15043511.


72. Yin M, Wheeler MD, Kono H, Bradford BU, Gallucci RM, Luster MI, et al. Essential role of tumor necrosis factor α in alcohol-induced liver injury in mice. Gastroenterology 1999;117:942-952. 10500078.


73. Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology 2011;141:1572-1585. 21920463.



74. Larrey D. Epidemiology and individual susceptibility to adverse drug reactions affecting the liver. Semin Liver Dis 2002;22:145-155. 12016546.


76. Lucena MI, Andrade RJ, Kaplowitz N, García-Cortes M, Fernández MC, Romero-Gomez M, et al. Phenotypic characterization of idiosyncratic drug-induced liver injury: The influence of age and sex. Hepatology 2009;49:2001-2009. 19475693.


77. Williams KV, Nayak S, Becker D, Reyes J, Burmeister LA. Fifty years of experience with propylthiouracil-associated hepatotoxicity: what have we learned? J Clin Endocrinol Metab 1997;82:1727-1733. 9177371.


78. Emiliano AB, Governale L, Parks M, Cooper DS. Shifts in propylthiouracil and methimazole prescribing practices: antithyroid drug use in the United States from 1991 to 2008. J Clin Endocrinol Metab 2010;95:2227-2233. 20335447.




79. Franklyn JA. Thyroid gland: Antithyroid therapy-best choice of drug and dose. Nat Rev Endocrinol 2009;5:592-594. 19844246.



80. Rivkees SA, Mattison DR. Propylthiouracil (PTU) hepatoxicity in children and recommendations for discontinuation of use. Int J Pediatr Endocrinol 2009;2009:132041. 19946400.



81. Jonas MM, Eidson MS. Propylthiouracil hepatotoxicity: two pediatric cases and review of the literature. J Pediatr Gastroenterol Nutr 1988;7:776-779. 3054039.


82. Rivkees SA, Stephenson K, Dinauer C. Adverse events associated with methimazole therapy of graves' disease in children. Int J Pediatr Endocrinol 2010;2010:176970. 20224800.



83. Boelsterli UA, Lim PL. Mitochondrial abnormalities--a link to idiosyncratic drug hepatotoxicity? Toxicol Appl Pharmacol 2007;220:92-107. 17275868.


84. Mete UÖ, Kaya M, Çolakoglu S, Polat S, Tap Ö, ÖZbilgin MK, et al. Ultra-structure of the liver in propylthiouracil induced hepatitis. J Isl Acad Sci 1993;6:268-276.
85. Strolin Benedetti M, Whomsley R, Baltes EL. Differences in absorption, distribution, metabolism and excretion of xenobiotics between the paediatric and adult populations. Expert Opin Drug Metab Toxicol 2005;1:447-471. 16863455.


86. Ginsberg G, Hattis D, Sonawane B. Incorporating pharmacokinetic differences between children and adults in assessing children's risks to environmental toxicants. Toxicol Appl Pharmacol 2004;198:164-183. 15236952.


87. Cooper DS, Goldminz D, Levin AA, Ladenson PW, Daniels GH, Molitch ME, et al. Agranulocytosis associated with antithyroid drugs: effects of patient age and drug dose. Ann Intern Med 1983;98:26-29. 6687345.


88. Ramos-Bonner LS, Goldberg TH, Moyer S, Anastasopoulou C. Methimazole-induced cholestatic jaundice in an elderly hyperthyroid patient. Am J Geriatr Pharmacother 2007;5:236-240. 17996663.


91. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-499. 11836274.


94. Seven A, Seymen O, Hatemi S, Hatemi H, Yiğit G, Candan G. Anti-oxidant status in experimental hyperthyrodism: effect of vitamin E supplementation. Clin Chim Acta 1996;256:65-74. 8960788.


95. Komosinska-Vassev K, Olczyk K, Kucharz EJ, Marcisz C, Winsz-Szczotka K, Kotulska A. Free radical activity and antioxidant defense mechanisms in patients with hyperthyroidism due to Graves' disease during therapy. Clin Chim Acta 2000;300:107-117. 10958867.


96. Venditti P, Balestrieri M, Di Meo S, De Leo T. Effect of thyroid state on lipid peroxidation, antioxidant defences, and susceptibility to oxidative stress in rat tissues. J Endocrinol 1997;155:151-157. 9390017.


97. Venditti P, Di Meo S. Thyroid hormone-induced oxidative stress. Cell Mol Life Sci 2006;63:414-434. 16389448.


98. Levy M. Propylthiouracil hepatotoxicity. A review and case presentation. Clin Pediatr (Phila) 1993;32:25-29. 8419095.

99. Yang J, Zhong J, Zhou LZ, Hong T, Xiao XH, Wen GB. Sudden onset agranulocytosis and hepatotoxicity after taking methimazole. Intern Med 2012;51:2189-2192. 22892501.


100. Vilchez FJ, Torres I, Garcia-Valero A, Lopez-Tinoco C, de Los Santos A, Aguilar-Diosdado M. Concomitant agranulocytosis and hepatotoxicity after treatment with carbimazole. Ann Pharmacother 2006;40:2059-2063. 17077174.


101. Becker CE, Gorden P, Robbins J. Hepatitis from methimazole during adrenal steroid therapy for malignant exophthalmos. JAMA 1968;206:1787-1789. 4177058.


102. Lee SO, Choi JK, Kim HS, Seo JS, Ahn DS. A case of similar pattern of hepatotoxicity after propylthiouracil and methimazole. Korean J Hepatol 1999;5:136-141.
103. Heidari R, Babaei H, Eghbal MA. Cytoprotective effects of organosulfur compounds against methimazole-induced toxicity in isolated rat hepatocytes. Adv Pharm Bull 2013;3:135-142. 24312826.


104. Heidari R, Babaei H, Eghbal MA. Ameliorative effects of taurine against methimazole-induced cytotoxicity in isolated rat hepatocytes. Sci Pharm 2012;80:987-999. 23264945.



105. Roy G, Bhabak KP, Mugesh G. Interactions of antithyroid drugs and their analogues with halogens and their biological implications. Cryst Growth Des 2011;11:2279-2286.

106. Manna D, Roy G, Mugesh G. Antithyroid drugs and their analogues: synthesis, structure, and mechanism of action. Acc Chem Res 2013;46:2706-2715. 23883148.


107. Roy G, Mugesh G. Anti-thyroid drugs and thyroid hormone synthesis: effect of methimazole derivatives on peroxidase-catalyzed reactions. J Am Chem Soc 2005;127:15207-15217. 16248663.


Figure 1
Susceptibility factors make patients more vulnerable to the toxicity induced by drugs. Presence of risk factors might make antithyroid drugs to be more hepatotoxic in lower doses.

Figure 2
Antithyroid drugs glucuronidation. UGTs catalyze glucuronic acid transfer to drugs: a way to prepare these medications for excretion. (A) Proposed glucuronic acid conjugates of the methimazole. (B) PTU glucuronidation. The differences in UGT enzymes activities between different persons might alter antithyroid drugs pharmacokinetic which consequently lead to hepatotoxicity. UGT, uridinediphospho glucuronosyltransferase.

Figure 3
Antithyroid drugs prescription in US, from year 1991 to 2008. This figure is reprinted from reference "78" with permission from corresponding author ( Dr. David Cooper, Professor of Medicine, Division of Endocrinology, Diabetes, & Metabolism, The Johns Hopkins University, School of Medicine). MMI, Methimazole; PTU, propylthiouracil.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




